Watch and wait in locally advance rectal cancer: Past, present and future
Miriam Alvarez-Aguilera, Rosa M Jimenez-Rodriguez
Miriam Alvarez-Aguilera, Rosa M Jimenez-Rodriguez, Departamento de Cirugía, Hospital Universitario Virgen del Rocio, Sevilla 41013, Spain
Abstract In rectal cancer, a complete pathological response after neoadjuvant therapy means better rates survival and better rates of local recurrence.Nevertheless, these patients suffer from complications following surgery such as low anterior resection syndrome, sexual dysfunction or colostomy for the rest of their lives.Due to this, several groups are working in an organ preservation strategy when a clinical response is diagnosed.This strategy is known as watch and wait.In this editorial, we review the past, present and future perspectives for this conservative management.
Key Words: Rectal cancer; Watch and wait; Neoadjuvant treatment; Organ preservation; Complete response
INTRODUCTION
The treatment for rectal cancer has changed in the last years due to technical advances: From the surgical technique, to stage and to pre and postop treatments.Nowadays, the standard treatment includes neoadjuvant therapy followed by total or subtotal mesorectal excision and adjuvant therapy[1] achieving excellent local control rates.Nevertheless, a third of the patients diagnosed with rectal cancer died due to distant metastasis[2].
Moreover, this multimodal treatment still has complications, including those coming from surgery: Infections, permanent ostomies, toxicity from chemo and radiotherapy, neurotoxicity or anterior resection syndrome and in some cases even death[3-5].
All these adverse effects cause a decrease in the quality of life of our patients.Due to this, current trend is to tailor the treatment regarding the tumor, its size, location stage and molecular characteristics as well as the own patient.
An example of this tailored treatment is the PROSPECT trial[6], a phase 2/3 clinical trial proposing to suppress systematic preoperative chemoradiotherapy.The authors describe the administration of 6 cycles of FOLFOX as neoadjuvant therapy followed by re-stage of the tumor and selectively use of radio and chemotherapy regarding the response of the tumor.
Despite the different schemas the final objective of all these preoperative treatments is maximize the number of tumor complete responses because these patients with pathological complete response (pCR) will develop a local recurrence rate of 1% and 95% 5-year survival[7-10].In addition to this, this patients without viable tumor in the specimen could benefit from a non-surgical management thus if we increase the rate in complete responses we will increase the number of patients which could benefit from a non-operative management.
This non-surgical management or watch and wait is not new.Traditionally it has been attempted in frail and old patients with high risk for surgery and with response to the neoadjuvant therapy.We could name this strategy as a “casual watch and wait” or “watch and wait by necessity”.
Recently this strategy has been published as intentional and not casual watch and wait.Habr-Gamaet al[11] described in their work in 2004 their results after treating with neoadjuvant therapy, 265 patients with rectal cancer.These patients were reassessed 8 wk after the end of the neoadjuvant therapy and those with complete clinical response entered into a watch and wait policy.Those patients without complete clinical response underwent surgery.Disease-free survival rates were 100% and 92% after 57 mo.In this work, authors reported 2 local regrowths who underwent salvage surgery and stayed alive and disease-free at the end of the study.
Habr-Gamaet al[11] concluded that in association with a careful follow-up, watch and wait for rectal cancer is safe and feasible.
More recent studies show pool analysis cases suggesting that watch and wait (WW) is feasible with similar survival rates to the traditional surgery and regrowth rates lower than 20%[12].
There is a difference between complete clinical response (cCR) and pCR.The first one is the absence of tumor after neoadjuvant therapy and the second one is the absence of viable tumor cells in the specimen after surgery.And sometimes these 2 options do not overlap.Current test cannot distinguish between tumor cells and fibrosis.In fact, up to 38% patients with an incomplete clinical response show after surgery pathological complete response[9].This is a difficult situation for a patient and for a surgeon who have to choose between planning one or other approach.
There are different ways of increasing clinical complete response with the aim of increasing the number of patients who can benefit from a watch and wait strategy.One strategy is by optimizing preoperative radiotherapy.There are 2 ways of administering radiotherapy: Short course (25 Gy in 5 fractions) or long course (2 Gy fractions for in 2 Gy sessions for a total of 40 Gy to 50.4 Gy).Two prospective randomized trials[13,14] analyzed differences between these 2 modalities.The findings suggest there are no differences regarding local recurrences, survival or toxicity but there are differences regarding the rate of complete response in the specimen (0.7% in the short course modality against 16% in patients receiving long course radiotherapy).Other studies such as the one published by Bujkoet al[13] and Cummingset al[15] studied the results of the short course in elderly population.These studies have a very small population, 30 and 20 cases respectively, and both studies concluded that WW is feasible after short course radiotherapy in elderly patients.Other studies such as the RAPIDO trial[16] randomized all patients to chemoradiotherapy (CRT) followed by surgery and optional adjuvant therapy or to total neoadjuvant therapy including short course radiotherapy, 6 cycles of CapeOx and followed by surgery will show more information about the role of short course radiotherapy in WW.
As far as increasing tumor radio sensibility, the German study CAO/ARO/AIO-04[17] demonstrated the benefit of adding oxaliplatin to CRT to maximize the outcomes of neoadjuvant therapy in terms of complete pathological response (17%vs13%).This finding was consolidated after the follow-up with a 76%vs71% 3-year disease-free survival (DFS).Nowadays the RAPIDO trial[16] has shown differences in toxicity in the experimental group (84%) but not in postoperative complications.
Another aspect is increasing waiting time after the end of neoadjuvant therapy.Tumor response to radiotherapy depends on the waiting time and sometimes a complete response could be delayed months.Although tumoral damage is produced during radiotherapy the lysis of the cells occurs days and even weeks after the end of the treatment.Surgery delay could increase the rate of pathological complete response from 0%, right after finishing CRT to 11% when the interval is 11 wk[15].From that moment the rate of pathological complete response does not increase.Other studies also showed that an increase in complete response rates means a decrease in complication and readmission rates after surgery and similar survival rates.The TiMiSNAR trial[18] included 300 patients divided in 2 groups: Those receiving surgery 8 wk after surgery and those who underwent surgery 12 wk after CRT to determine when we should diagnose a pCR without affecting oncological outcomes.
Another strategy is adding chemotherapy to neoadjuvant therapy like induction or consolidation.There are studies that analyzed the result of induction or consolidation therapies in patients that also receive the classical schema: CRT and surgery.Consolidation therapy[19] has been associated to less toxicity, higher rate of completion and higher rates of pCR (25%vs17%).Current evidence supports consolidation therapy as more favorable to increase the number of pCR and thus, WW.Nevertheless, we are still waiting the results coming from studies like the OPRA trial[20] where patients are randomized to induction or consolidation and surgery or WW.
All these strategies increase the rate of pCR and as consequence higher rates of WW.But once we decide we can offer a WW strategy, what should we do?
The first step is to determine the precise stage.Stage 2 and 3 tumors will benefit from neoadjuvant treatment, will possibly respond and will be candidates for a WW strategy.However, stage 1 tumors can also be included.This stage should be done with rectal exam, endoscopy and magnetic resonance imaging (MRI).Incomplete or complete response will be considered regarding our findings (Table 1).
Patient should be trustable and involved with the follow-up, to detect regrowths and perform surgery if needed.Follow-up should be performed as described in Table 2.
A group of patients will have more options of benefit from a WW strategy, for example those with more distal or smaller tumors requiring ultralow anastomosis or abdominoperineal resections.Bigger and circumferential tumors usually develop concentric scars inside the rectum obstructing the assessment of the tumor response.These patients could not be the ideal candidates for a WW program.Those with a higher risk of tumor progression might not be good candidates for this non-surgical management either.Smithet al[5] published a higher risk of distant metastasis in those patients who developed a regrowth (36%vs1%,P< 0.001).This author declares the higher rate in the regrowth group could be due to delays in surgery or to more aggressive tumors.
We should begin with neoadjuvant treatment including chemo and radiotherapy and assess after 8-12 wk.At this point, there are different options:
cCR: scar, telangiectasia, and findings in the MRI suggesting cCR.We could suggest follow-up.
Incomplete clinical response: surgery.
Nearly complete clinical complete response: A follow-up could be suggested every 6-8 wk if the tumor still responds.If there is a regrowth, we should recommend surgery.
These recommendations are likely to be modified in the next few months with the information obtained from the different ongoing studies described previously, such as the OPRA[20] trial, that aim to assess the results of consolidation chemotherapy.
As we mentioned before, a certain group of patients might experience tumor regrowth during WW follow-up.A variety of studies claim that this scenario is more likely to show up in the first 2 years after neoadjuvant treatment rather than later on[5].After carefully analyzing the graphical representation of these regrowth patterns, only a few patients are at risk of suffering this regrowth.Nevertheless, it is certainly hard to determine who will experience this, when it will happen, and which follow-up method may be the most effective one (DNAc, biopsies, imaging,etc.).
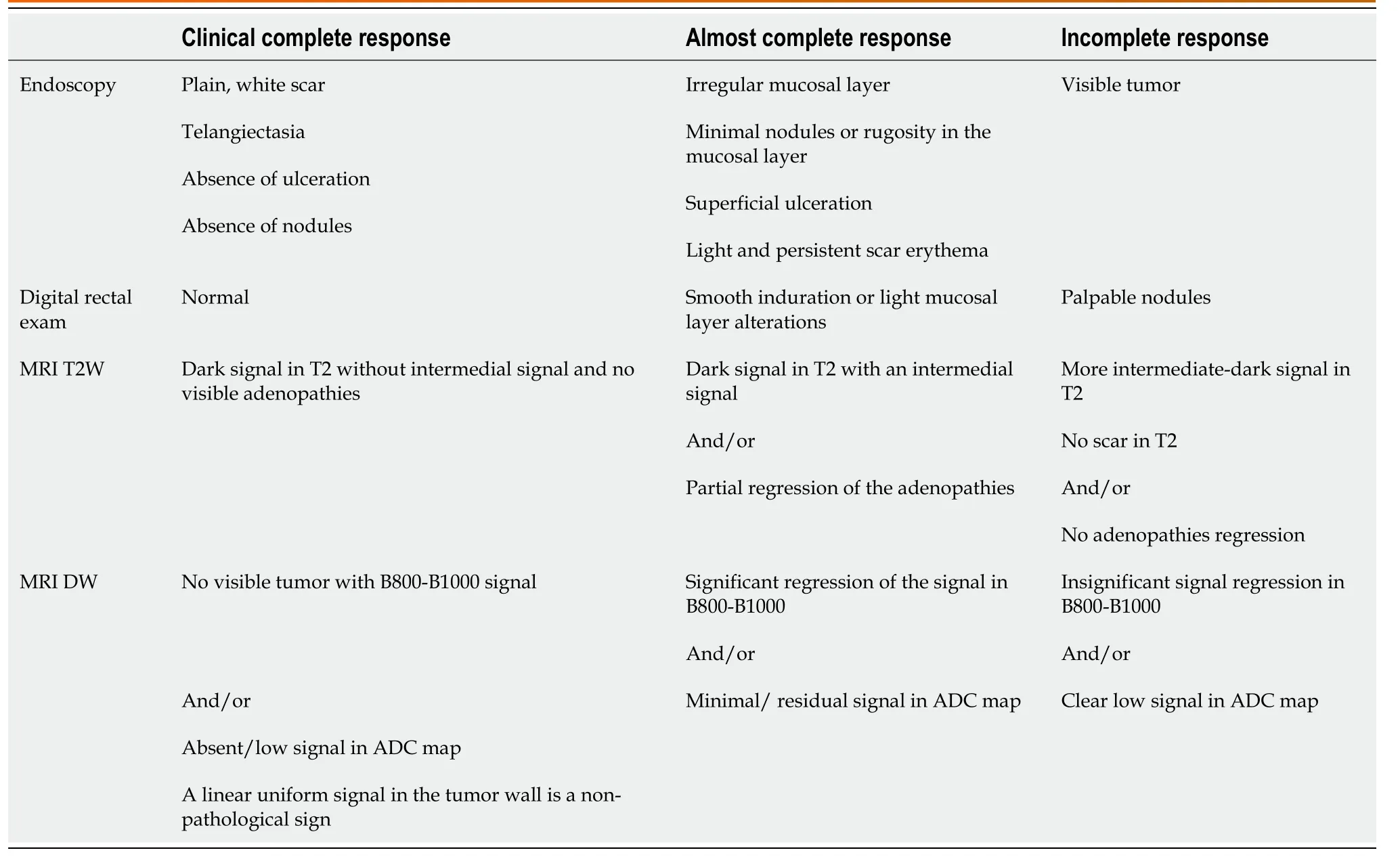
Table 1 Clinical response criteria regarding findings in rectal exam, endoscopy and magnetic resonance imaging described in OPRA trial[20]
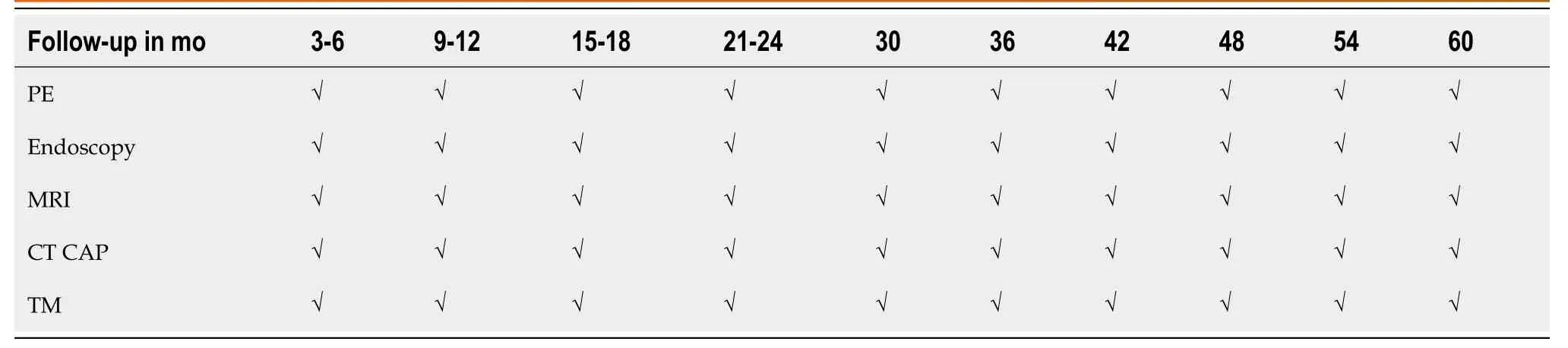
Table 2 Recommendations for follow-up for patients under a watch and wait strategy regarding OPRA trial[20]
Several authors have published failure rates after a WW trial reporting a wide range of results, from 3% described by Habr-Gamaet al[11] in his first study up to a 30% in other publications[21], clearly higher numbers when compared to the Brazilian group.It might be due to the exclusion of the first 12 mo of follow-up in the Brazilian group, and consequently the first 12-mo regrowth rate.
More recent studies show locoregional recurrence rate of about a 19%[5,20] as the closest to the real number.This recurrence might occur deep into the mucosal layer and therefore could be difficult to detect before the sphincteric complex is affected.However, in the presence of this scenario, savage surgery can be offered to the patient achieving a similar survival rate as to an initial surgery without a WW first step.
CONCLUSION
Patients with rectal cancer who undergo neoadjuvant therapy could present a complete clinical response.When this happens, these patients might benefit from a non-surgical strategy associated with an exhaustive follow-up as long as they are aware of the implications of this pathway.In the event of a tumor regrowth, savage surgery can be offered to them with similar oncological results.Nonetheless, future investigations are in order to elucidate the most proper candidates and follow-up methods for this treatment alternative.
 World Journal of Meta-Analysis2021年4期
World Journal of Meta-Analysis2021年4期
- World Journal of Meta-Analysis的其它文章
- Trends in iron deficiency anemia research 2001-2020: A bibliometric analysis
- Systematic review and Meta-analysis of efficacy and safety of dienogest in treatment of endometriosis
- Systematic review with meta-analysis of the epidemiological evidence in Europe, Israel, America and Australasia on smoking and COVID-19
- Troponin I biomarker as a strong prognostic factor for predicting COVID-19 mortality: A systematic review
- Fate of root shell after pontic/socket shield techniques, is it better to extract the whole tooth?
