Phase 1 studies comparing safety,tolerability,pharmacokinetics and pharmacodynamics of HLX01 (a rituximab biosimilar) to reference rituximab in Chinese patients with CD20-positive B-cell lymphoma
Yuankai Shi,Qingyuan Zhang,Xiaohong Han,Yan Qin,Xiaoyan Ke,Hang Su,Li Liu,Jinxiang Fu,Jie Jin,Jifeng Feng,Xiaonan Hong,Xiaohong Zhang0,Depei Wu,Bin Jiang,Xiaodong Dong
1National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital,Chinese Academy of Medical Sciences &Peking Union Medical College,Beijing Key Laboratory of Clinical Study on Anticancer Molecular Targeted Drugs,Beijing 100021,China;2 Harbin Medical University Cancer Hospital,Harbin 150081,China;3Peking University Third Hospital,Beijing 100191,China;4The 307th Hospital of Military Chinese People’s Liberation Army,Beijing 100071,China;5Tangdu Hospital of the Fourth Military Medical University,Xi’an 710038,China;6The Second Affiliated Hospital of Soochow University,Suzhou 215004,China;7The First Affiliated Hospital Zhejiang University College of Medicine,Hangzhou 310006,China;8Jiangsu Cancer Hospital,Nanjing 210009,China;9Fudan University Shanghai Cancer Center,Shanghai 200032,China;10The Second Affiliated Hospital Zhejiang University School of Medicine,Hangzhou 310003,China;11The First Affiliated Hospital of Soochow University,Suzhou 215006,China;12 Peking University People’s Hospital,Beijing 100034,China;13 Shanghai Henlius Biotech,Inc.,Shanghai 200233,China
Abstract Objective:This study aimed to compare the pharmacokinetic,pharmacodynamic and safety profiles of HLX01(a rituximab biosimilar) and reference rituximab sourced from China (MabThera®;rituximab-CN).Methods:Here we report the results of two phase 1 studies.In the phase 1a,open-label,dose-escalation study(NCT03218072,CTR20140400),eligible patients received 250,375 and 500 mg/m2 HLX01 sequentially at 7-day intervals,after confirming no dose-limiting toxicity (DLT).In the phase 1b,double-blind study (NCT02584920,CTR20140764),eligible patients were given a single dose of 375 mg/m2 HLX01 or rituximab-CN.The primary endpoints included safety and tolerability parameters for the phase 1a and the area under the plasma concentrationtime curve from time zero to day 91 (AUC0-91d) for the phase 1b study.Equivalence was concluded if 90%confidence interval (90% CI) for the geometric least squares mean ratio (GLSMR) fell in the pre-specified equivalence criteria (80%-125%).Results:Between June 20,2014 and January 5,2015,12 patients were enrolled in the phase 1a study.The pharmacokinetics of HLX01 showed dose proportionality and accumulation to steady state.HLX01 was well tolerated,with no serious adverse events (AEs),discontinuations or DLTs.Between November 8,2014 and August 13,2015,87 eligible patients were enrolled in the phase 1b study,including 43 who received HLX01 and 44 who were treated with rituximab-CN.The equivalence endpoint was met with GLSMR for AUC0-91d being 89.6%(90% CI:80.4%-99.8%).AEs,anti-drug antibodies,and CD19+and CD20+B lymphocyte counts were similar between the HLX01 and rituximab-CN treatment groups.Conclusions:Treatment with HLX01 was safe and well tolerated in Chinese patients with B-cell lymphoma.HLX01 and rituximab-CN have similar pharmacokinetic,pharmacodynamic and safety profiles.
Keywords:Biosimilar;lymphoma;monoclonal antibody;pharmacokinetics;safety
Introduction
Non-Hodgkin lymphoma (NHL) is the most common adult hematological cancer worldwide,with 85% of cases derived from B lymphocytes (1-3).As the most prevalent form of NHL,diffuse large B-cell lymphoma (DLBCL)accounts for approximately one third of lymphoid malignancies in Western countries and in China (4-6).
Rituximab is a chimeric mouse/human anti-CD20 monoclonal antibody,which has been approved for the treatment of B-cell malignancies for over two decades.CD20 is a valuable therapeutic target in B-cell NHL,since it is expressed as a B-cell-specific cell surface antigen of pre-B and mature B lymphocytes,occurring in more than 90% of B-cell lymphomas (7).
Improved clinical outcomes for patients with B-cell malignancies treated with rituximab have been confirmed in practice,and this treatment option represents a significant advance in the treatment of B-cell NHL,both as monotherapy and in combination with chemotherapy regimens (7-10).Rituximab maintenance therapy also provides survival benefits to patients with follicular lymphoma and mantle cell lymphoma (11,12).
Whilst rituximab provides clear clinical benefit,patients’access to this product is restricted due to its high costs in China (13).HLX01,the first biosimilar product manufactured in China,was approved by the National Medical Products Administration (NMPA) on February 22,2019 (14,15).It was developed in accordance with the NMPA and the World Health Organization similar biotherapeutic product development guidelines.Similarities between HLX01 and reference rituximab in their physicochemical properties and biological activities have previously been demonstrated (16).
An approval of biosimilar products requires demonstration of similar efficacy and safety between biosimilar and reference drug (17).It is necessary to carefully select endpoints to ensure that differences between biosimilar and reference drug are the main focus,while evaluating the impacts of other factors such as tumor burden,previous treatment and underlying clinical conditions.The stepwise approach of biosimilar development and demonstration of similar efficacy and safety requires demonstration of equivalence in pharmacokinetics (PK) and pharmacodynamics (PD) in clinical trials.
Here we report the findings of two phase 1 (1a and 1b)studies of HLX01.Phase 1a study assessed PK,PD,safety and tolerability with escalating and then multiple doses of HLX01.Phase 1b study was a single-dose,multicenter,randomized,double-blind,parallel-controlled study that compared PK,PD,safety and immunogenicity profiles between HLX01 and reference rituximab sourced from China (MabThera®;rituximab-CN).It was the first PK/PD study of reference rituximab in Chinese patients.
Materials and methods
HLX01 and rituximab-CN
Reference rituximab (MabThera®) was purchased from Shanghai Roche Pharmaceuticals Ltd,China.HLX01[(Han-Li-Kang®) Rituximab Injection] was manufactured by Shanghai Henlius Biotech,Inc.,China.
Study design and ethics
Phase 1a study (NCT03218072,CTR20140400) was an open-label,dose-escalation study conducted at two sites in China.Patients were enrolled sequentially into one of three dose-escalating cohorts (250,375 and 500 mg/m2).Following the initial infusion of HLX01,patients were monitored for seven days through the recording of vital signs,laboratory tests and safety indicators.Enrolment into the sequential,dose-escalating cohort was only permitted if the incidence of dose-limiting toxicities (DLTs) during the monitoring period occurred in less than one-third of participants.In the absence of DLTs,patients in each cohort received further three doses of HLX01,administered weekly.The total observation period was 13 weeks from the initial dose.The primary objective of the phase 1a study was to evaluate the safety and tolerability of single and multiple escalating intravenous (IV) doses of HLX01.
The phase 1b study (NCT02584920,CTR20140764)was a randomized,double-blind,parallel-controlled study conducted at 12 sites in China (Supplementary Table S1).Patients were randomized 1:1 to receive a single IV dose of HLX01 (375 mg/m2) or rituximab-CN (375 mg/m2) and were observed for up to 13 weeks (91±3 d).The primary endpoint was the area under the plasma concentration-time curve (AUC) from time zero to day 91 (AUC0-91d).Equivalence was achieved if 90% confidence interval (90%CI) of the geometric least square mean ratio (GLSMR) of AUC0-91dfell in the pre-specified equivalence margins of 80%-125%.Secondary endpoints included AUC from time zero to week 1,2,4 and 8,AUC from time zero to infinity (AUC0-inf) and maximum drug concentration(Cmax).Other objectives were to compare the PD parameters of HLX01 and rituximab-CN,and evaluate the safety and immunogenicity of HLX01 maintenance therapy.
The study was conducted in accordance with the Declaration of Helsinki,and applicable national and local regulations for clinical trials.It received approval from independent ethics committees at each participating center,and written informed consent was obtained from all patients who participated in this study prior to screening.
Patients
Eligible patients were adults aged 18-65 years,with histologically diagnosed CD20+B-cell lymphoma.Patients in phase 1a study had relapsed/refractory B-cell lymphoma requiring consolidation therapy,or chronic lymphocytic leukemia with a peripheral leukocyte count ≤50×109/L.Patients who had achieved complete remission (CR) or unconfirmed CR (CRu) after prior treatment,had peripheral leukocyte counts ≤5×109/L and were considered by the Investigator as likely to benefit from further maintenance treatment,were enrolled in the phase 1b study.Key exclusion criteria for both studies were primary or secondary immunodeficiency,and use of hematopoietic growth factors within one week of enrollment or live vaccines within four weeks of enrollment.The cut-off periods for patients who had received prior rituximab were two years (phase 1a) or four months (phase 1b) before study enrollment.For the phase 1b study,a threshold for residual serum rituximab ≤24 μ g/mL was applied at screening(full inclusion and exclusion criteria are detailed inSupplementary Table S2).
Randomization and masking (phase 1b study)
Randomization was performed by an independent statistician using the PROC PLAN process (SAS software;Version 9.2;SAS Institute Inc.,Cary,NC,USA).Patients were stratified into two subgroups according to the history of rituximab use.Independent personnel were responsible for completing the blind packaging of each vial of study medication with randomization codes. Double-blind masking was achieved by a dispensing nurse,who was involved in the drug administration and preparation of the medication in identical infusion containers.
Safety and tolerability
In both studies,the safety analysis set comprised all patients who received ≥1 dose of study drug.Safety and tolerability were assessed by physical examinations,laboratory measurements and occurrence of adverse events (AEs),serious AEs (SAEs) and adverse drug reactions (ADRs).AEs,including infusion-related reactions (IRRs),were classified using Medical Dictionary for Regulatory Activities Terminology (Version 16.1) and graded according to the National Cancer Institute Common Terminology Criteria for AEs (Version 4.03).All AEs were assessed for their relationship to the study drug;events that were very likely related or possibly related were defined as ADRs.DLT was defined as grade ≥4 hematologic toxicity or grade ≥3 non-hematologic toxicity,excluding IRRs.
PK evaluation
Serum concentrations of HLX01 and rituximab-CN were evaluated by validated enzyme-linked immunosorbent assay.In the phase 1a study,blood samples were collected before and immediately after each HLX01 and rituximab-CN infusion,with further samples collected following the first and fourth doses (at 2,24,72 and 120 h).In addition,samples were taken at 7,14±1,38±2 and 68±3 d after the fourth dose.
The PK analysis population for the phase 1b study comprised patients in the safety analysis set for whom AUC0-91dcould be reliably calculated and who had no major protocol deviations.Blood samples for analysis were collected within 1 h prior to study drug administration,immediately after study drug infusion and at 6,24,72 and 168±1 h.Further samples were collected at 14±1,28±2,56±3 and 91±3 d after study drug administration.The subgroup of patients that had received prior reference rituximab treatment also had samples collected at screening.
PD evaluation
The proportions and absolute counts of circulating lymphocytes were determined by flow cytometry.In the phase 1a study,testing was performed prior to study drug administration and at 72 and 168 h after the first dose of study drug.Other time points were immediately after administration of the fourth dose,and at 38±2 and 68±3 d thereafter.In the phase 1b study,samples were taken prior to study drug administration,and at 5 min,24 h,14±1,56±3 and 91±3 d after study drug infusion.
Immunogenicity evaluation
The presence of anti-drug antibodies (ADAs) was assessed by electrochemiluminescent immunoassay.In the phase 1a study,ADAs were analyzed prior to the first and third doses of HLX01,immediately after the fourth dose,and at 38±2 and 68±3 d thereafter.In the phase 1b study,testing was performed prior to study drug administration and at 14,28±2,56±3 and 91±3 d after study drug infusion.
Efficacy evaluation
No efficacy objective was defined in the phase 1b study because the patients had achieved CR/CRu prior to inclusion.However,the study design included evaluation of efficacy endpoints,CR,and CRu to determine whether the patients’ disease was stable.Fisher’s exact test was used at week 8 post study drug infusion to assess the overall efficacy rate.Computerized tomography (CT) scans were evaluated by the Investigator according to International Working Group 1999 and 2007 to assess treatment efficacy and response.
Statistical analysis
Sample size for the phase 1b study was estimated based on equivalence of primary endpoint of AUC.The smallest sample size was estimated to be 78 (n=39 per group),aiming for the equivalence margins of 80%-125%,with a two one-sided alpha (α) of 0.05,power of 90%,coefficient variation of 0.3 and the AUC ratio (study group:control group) of 1.0.
Statistical analyses were performed using the SAS software (Version 9.2;SAS Institute Inc.,Cary,NC,USA).PK parameters,including AUC from time zero to last sampling time point (AUC0-t),AUC0-infand AUC0-91d,were assessed via non-compartmental analysis using Phoenix WinNonlin®software (Version 6.3;Pharsight Corporation,Mountain View,California,United States).Cmaxconcentrations are reported as actual values.Descriptive statistics are reported for both studies and include mean,standard deviation,median and range(minimum and maximum values).AEs and ADA positivity are reported using frequency and percentages.For the phase 1b study,subgroup analyses were performed for immunogenicity,PK and PD parameters according to prior rituximab use.A sensitivity analysis of PK parameters by ADA status was also performed and the equivalence assessment was conducted in the ADA-negative and the ADA-positive (consecutive) subgroups.Inter-group comparisons of pre-treatment indicators and measurements were analyzed byt-test or Wilcoxon rank sum test,and enumeration data were analyzed by Fisher’s exact test.A P value <0.05 was considered statistically significant.
Results
Patient demographics
Between June 20,2014 and January 5,2015,a total of 12 patients,with relapsed/refractory B-cell lymphoma,were enrolled in the phase 1a study (Figure 1A).All patients received the first single dose and the subsequent four doses of HLX01.Patient baseline characteristics confirmed that all cohorts had a similar distribution of Eastern Cooperative Oncology Group (ECOG) performance status(PS),tumor type and number of prior lines of chemotherapy (Table 1).Most patients were male (66.7%)and the median age was 51.5 (range:31.5-64.3) years.Patients in the 375 mg/m2cohort (n=6;50.0% male) were younger (median age:42.5 years;range:31.5-51.5 years),with lower body weight compared with patients in the 250 mg/m2and 500 mg/m2cohorts (Table 1).
A total of 87 patients were enrolled in the phase 1b study between November 8,2014 and August 13,2015,including 43 patients in the HLX01 group and 44 patients in the rituximab-CN group (Figure 1B).Two patients discontinued prior to study completion;one patient in the HLX01 group withdrew consent and one patient in the rituximab-CN group experienced a treatment-emergent adverse event (TEAE).As one patient was excluded from the rituximab-CN group due to deviation from Good Clinical Practice guidelines,the safety analysis set comprised 86 patients.Of these patients,81 were included in the PK analysis,40 in the HLX01 group,and 41 in the rituximab-CN group.Five patients were excluded from the PK analysis;one had incomplete infusion data due to an IRR,three were ADA-positive prior to administration and one patient had an incomplete sample set due to withdrawn informed consent.Patients in both study groups were similar in terms of demographics and baseline disease characteristics,except that patients in the rituximab-CN arm had a slightly longer median duration of the disease compared with those in the HLX01 arm (1.3 yearsvs.0.9 years) (Table 1).Half of the patients in the safety analysis set had received prior rituximab treatment for B-cell lymphoma.
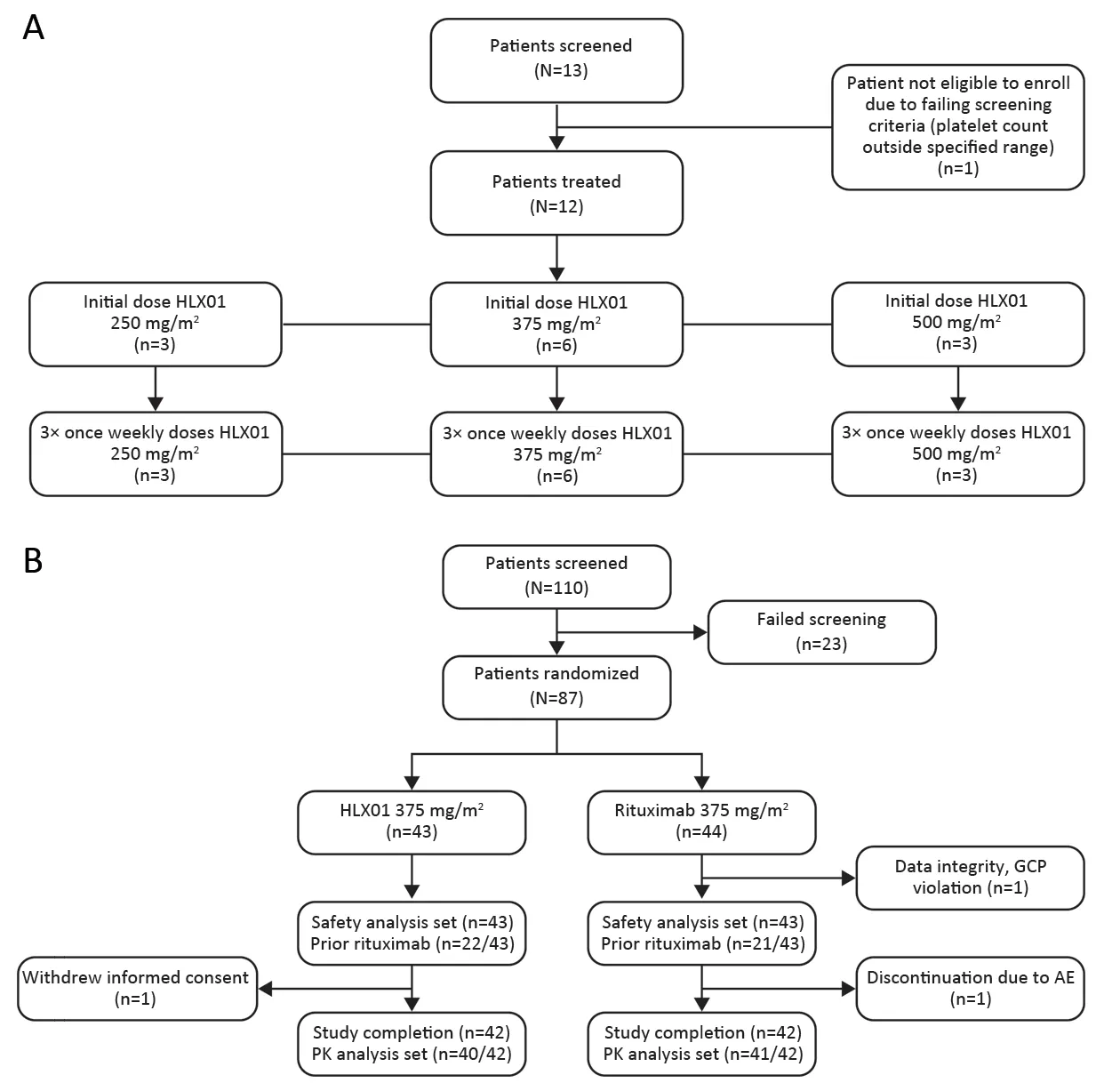
Figure 1 Patient flow diagrams for (A) phase 1a study and (B) phase 1b study.AE,adverse event;GCP,Good Clinical Practice;PK,pharmacokinetics.
PK
The PK characteristics of HLX01 (phase 1a) were assessed after single and multiple doses in each dose cohort(Supplementary Figure S1,Table S3).The AUC0-tand Cmaxshowed linear correlation with increasing administered dose (Supplementary Table S3).The mean terminal half-life(t1/2) after a single dose of HLX01 was 124.5 h across the dose ranges.Therefore,steady state would be anticipated at approximately 498.0-622.5 h.Consistently,the mean Cmaxof HLX01 after multiple doses in each cohort was higher than the mean Cmaxobserved after a single dose,indicating drug accumulation to steady state (data not shown).
In phase 1b study,22 patients in the HLX01 group and 21 patients in the rituximab-CN group had received prior rituximab treatment.The mean exposure to HLX01 and rituximab-CN was 648.7 mg and 624.7 mg in each treatment group (n=43 per treatment group),respectively.PK parameters following single-dose treatment were analyzed using a non-compartmental approach and are shown inSupplementary Table S4.The geometric mean AUC and AUC0-91dwere similar following single doses(375 mg/m2) of HLX01 and rituximab-CN (Figure 2,Table 2).The primary endpoint was met,as the GLSMR of AUC0-91d(HLX01:rituximab-CN;89.6 %) and 90% CI(80.4%-99.8%) fell in the pre-specified equivalence margins of 80%-125% (Table 2).The Cmaxfor HLX01 and rituximab-CN were similar (GLSMR:102.6%;90% CI:95.2%-110.6%).The GLSMR for AUC0-infwas 87.0%(90% CI:77.7%-97.5%) (Table 2),with the upper margin of 90% CI contained within and the lower margin falling outside the pre-specified equivalence margins.The sensitivity analysis of PK parameters by ADA status showed consistent results (Table 2).

Figure S1 Serum concentration-time curves () following (A) single dose and (B) multiple doses of HLX01 (250,375 and 500 mg/m2)(phase 1a study).
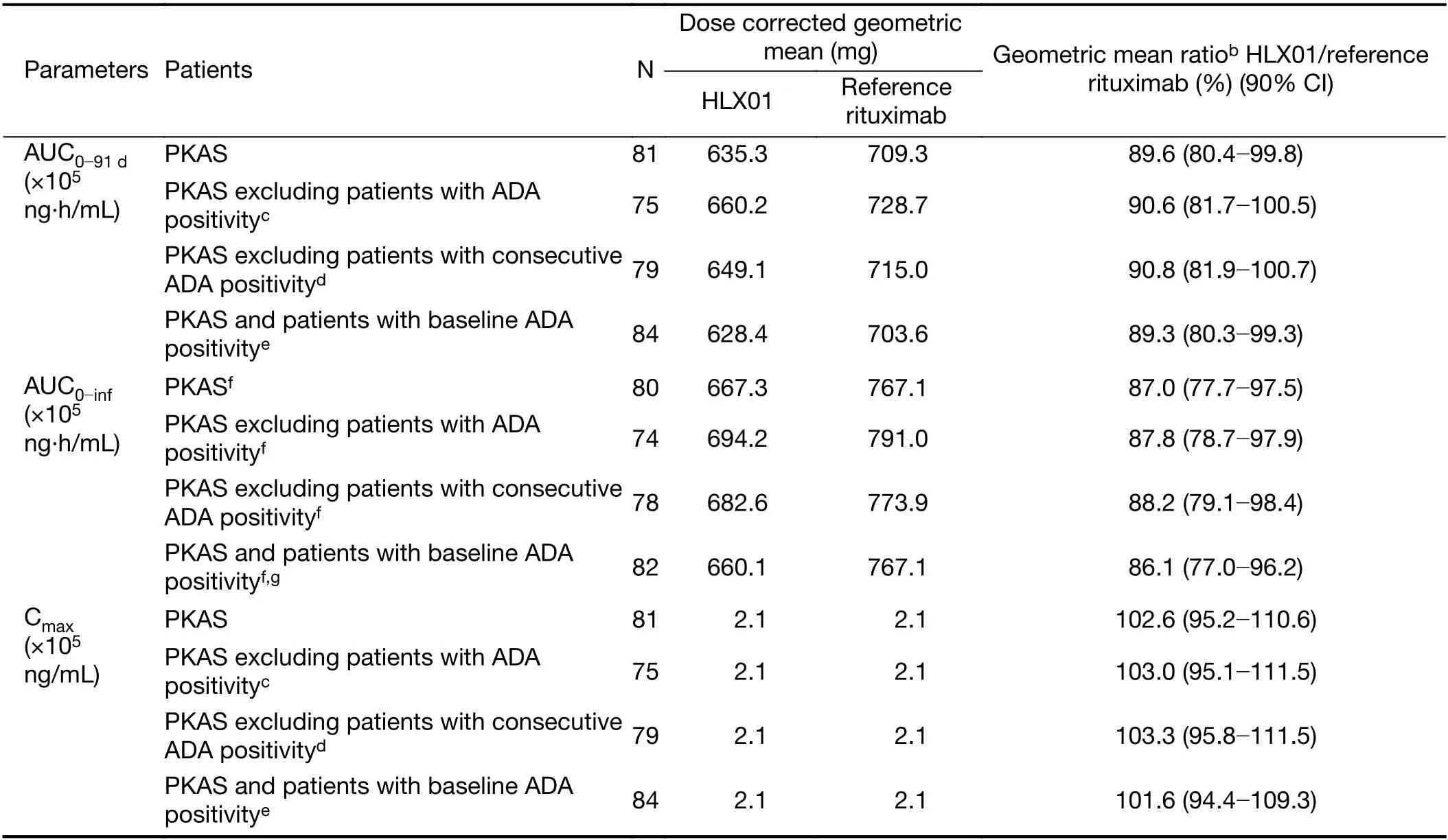
Table 2 Sensitivity analysis and evaluation of equivalence of PK parameters between HLX01 and reference rituximaba (375 mg/m2;phase 1b study)
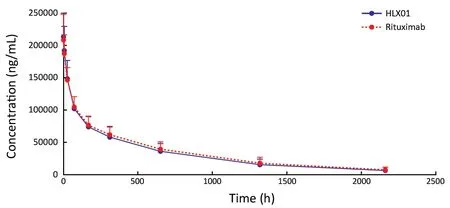
Figure 2 Serum concentration-time curves () following single doses of HLX01 and reference rituximab (phase 1b study).The reference rituximab was sourced from China (MabThera®;rituximab-CN),and 375 mg/m2 of HLX01 or reference rituximab was administered.
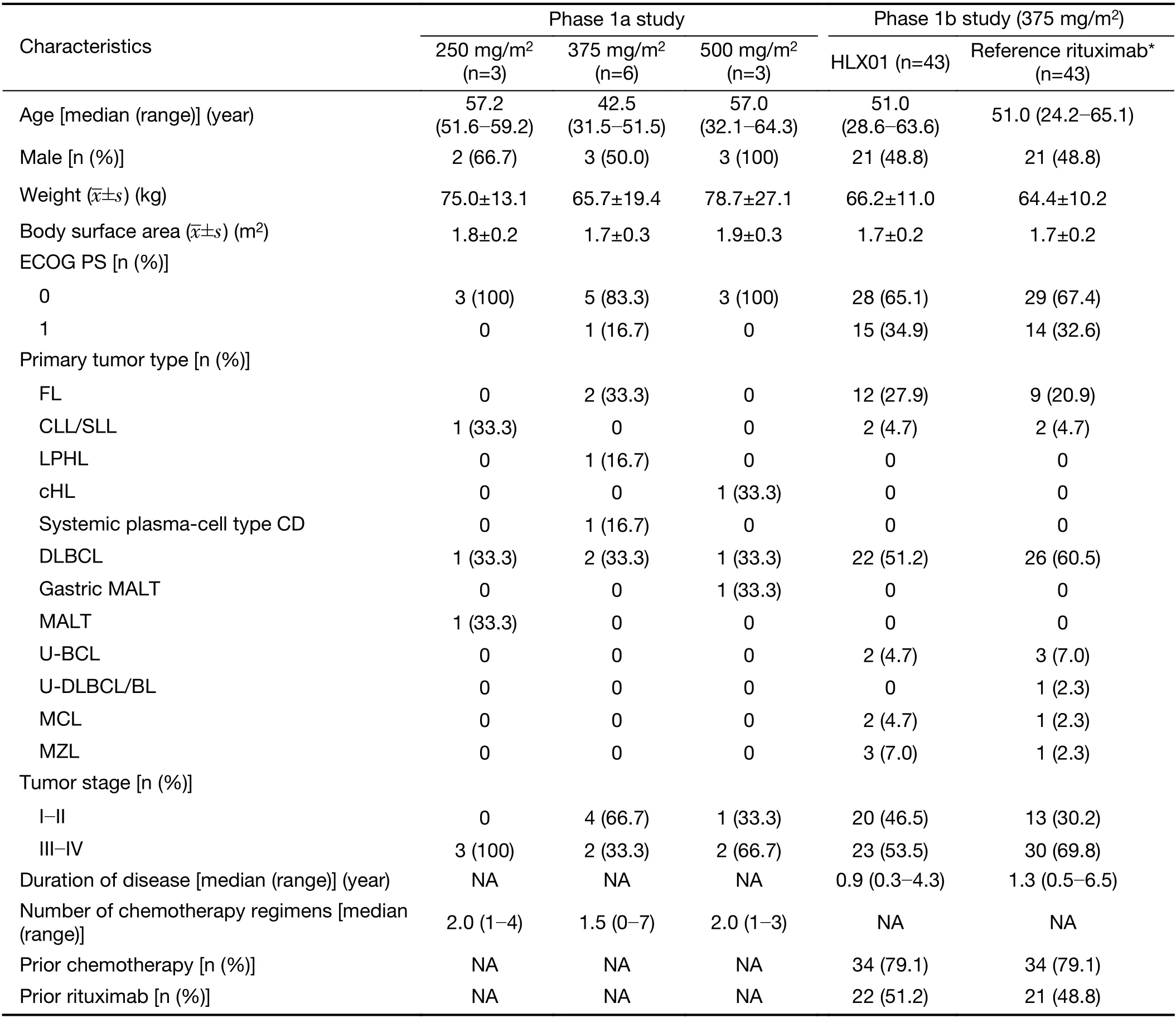
Table 1 Patients’ demographics and baseline characteristics (phase 1a study and phase1b study) in safety analysis set
Safety and tolerability
In the phase 1a study,no deaths,SAEs,AEs leading to treatment discontinuation,or DLTs were observed following single-dose administration of the three tested doses of HLX01.Mean drug exposures in the doseescalation cohorts (250,375 and 500 mg/m2) were 461.0,649.3 and 933.3 mg,respectively,after first infusion.Two patients experienced AEs after receiving single doses of 250 mg/m2HLX01 (Supplementary Table S5).
No deaths or TEAEs leading to treatment discontinuation after multiple-dose administration of HLX01 (250,375 and 500 mg/m2) were observed.One patient reported an SAE (grade 3 anal fistula) in the 500 mg/m2HLX01 cohort,which was considered unrelated to treatment by the Investigator (Supplementary Table S5).In total,35 TEAEs were recorded following administration of multiple doses of HLX01,including fever,chills and upper respiratory infection reported by ten patients (83.3%) in both the single-and multiple-dose periods (Supplementary Table S5) and 19 TEAEs experienced by seven patients(58.3%) that were considered very likely/possibly related to treatment (Supplementary Table S6).Of these 19 TEAEs,most were grade 1 (13 events) or grade 2 (5 events).Only one grade 3 recovering/resolving TEAE (elevated alanine aminotransferase) was considered likely/possibly related to treatment.A few changes in vital signs and physical examination relative to baseline were observed during the study.
In the phase 1b study,only one patient in the rituximab-CN group discontinued the single-dose infusion due to an IRR (a grade 1 scalp itchiness and rash) (Table 3).IRRs were reported in similar proportions of patients in the treatment groups (20.9% per HLX01vs.23.3% per rituximab-CN).No deaths or SAEs were reported following singledose treatment with HLX01 or rituximab-CN.
During the phase 1b study,115 AEs were reported (49 AEs in the HLX01 group and 66 AEs in the rituximab-CN group) (Table 3).Of the 49 AEs reported in the HLX01 group during the study,23 were classified as ADRs(Supplementary Table S7).Of the 66 AEs reported in the rituximab-CN group,34 were considered ADRs(Supplementary Table S7).When looking for clustering among these ADRs,there were multiple events of neutropenia,itchy skin/rashes and respiratory events.Most ADRs were resolved during the study.Most AEs were grade 1-2,with two patients in the rituximab-CN group experiencing grade 3 AEs during the study.No grade 3 AEs were reported in the HLX01 group during the study.There were no grade ≥4 AEs recorded over the observation period.
Immunogenicity
In the phase 1a study,serum samples were tested for the development of anti-HLX01 antibodies up to 90 d post first HLX01 infusion.One patient tested positive for ADA during the screening assessment and,therefore,did not enter the study.All other samples were ADA-negative.
In the phase 1b study,at baseline,two patients tested positive for anti-HLX01 antibodies (neither had prior rituximab use) and one patient tested positive for antirituximab antibodies.Two HLX01-treated patients and four rituximab-CN-treated patients tested positive for ADAs at ≥1 time points.There were no significant differences between treatment groups in ADA positivity.Of the five ADA-positive patients treated with rituximab-CN,two had used rituximab previously.
PD
In the phase 1a study,CD19+and CD20+B lymphocyte counts were reduced 72 h after the HLX01 infusion and remained at these lower levels at subsequent time points.CD4+and CD8+T cell counts (median) were replenished by day 90.
In the phase 1b study,depletion of CD19+and CD20+B lymphocyte counts occurred within 5 min of study drug administration and was maintained throughout the study to a similar extent for both HLX01 and rituximab-CN groups(intergroup difference at all time points:P>0.05) (Table 4).Similarly,within 5 min of study drug administration,the CD4+and CD8+T cell counts decreased from baseline in both groups,and returned to close to baseline values within 24 h and remained stable over the study duration(Supplementary Table S8).Inter-group comparison supported similarity between HLX01 and rituximab-CN,as P-values were >0.05,except for the 24-h CD4+cell count (P=0.04).
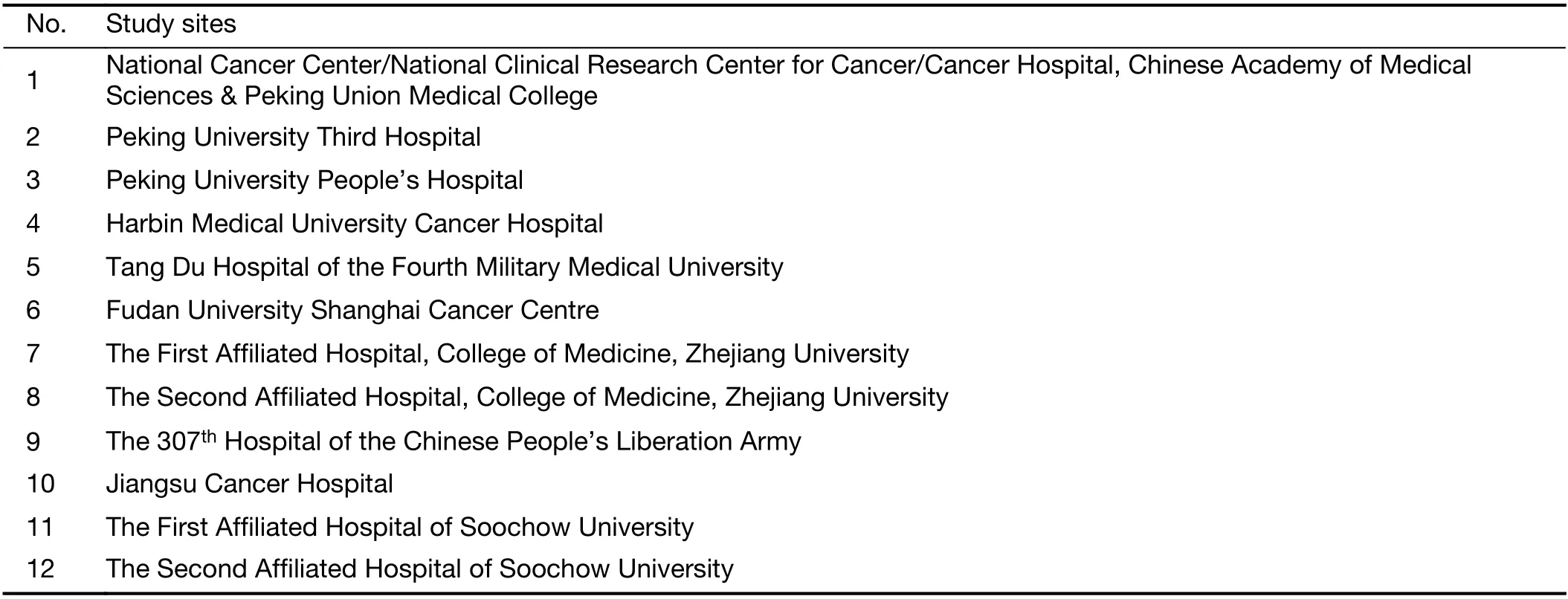
Table S1 Phase 1b study sites

Table S2 Inclusion and exclusion criteria of phase 1a study and phase 1b study

Table 3 TEAEs following single administration of HLX01 or reference rituximaba (phase 1b study)
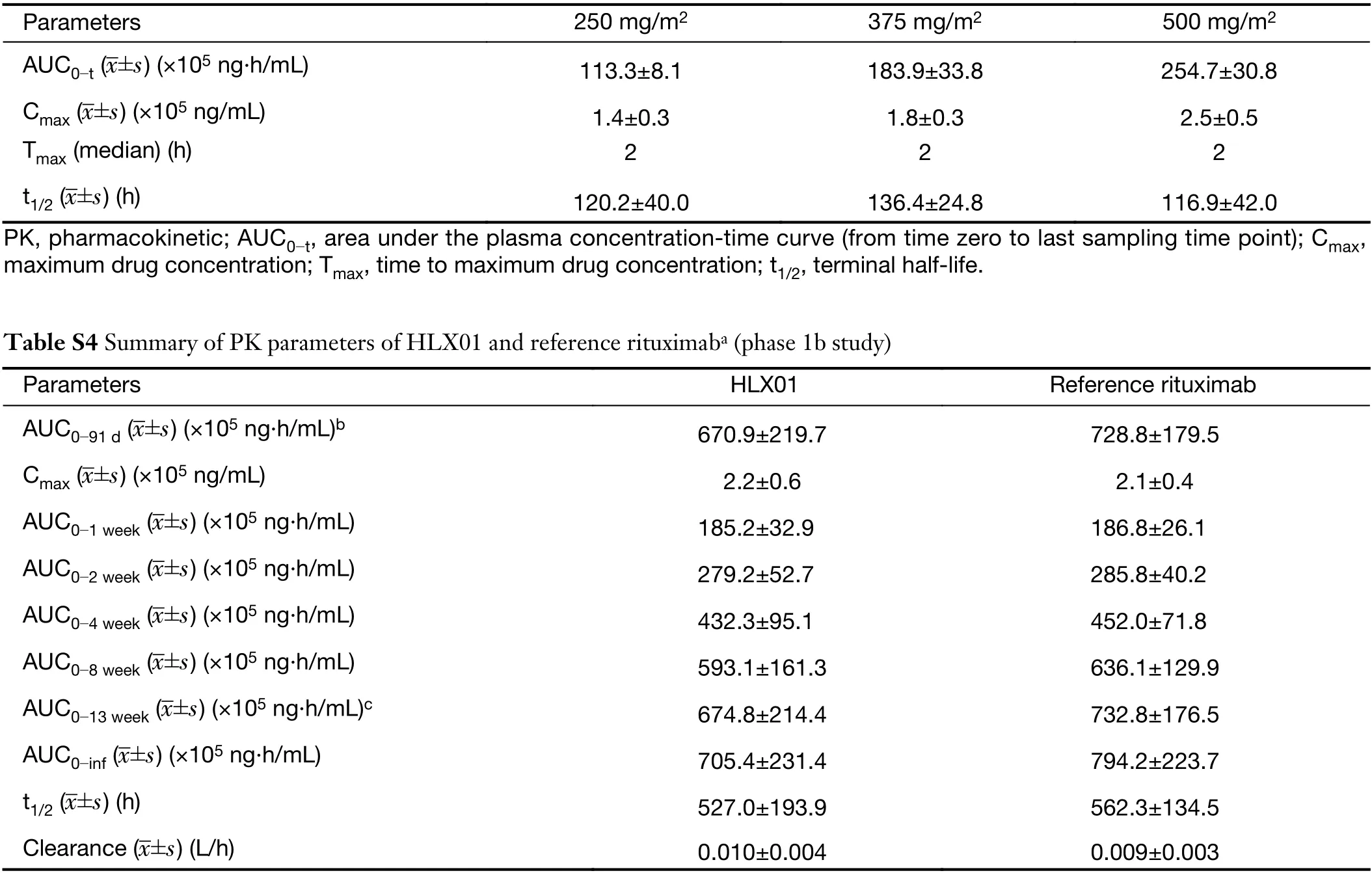
Table S3 Summary of PK parameters after single infusion of HLX01 (phase 1a study)
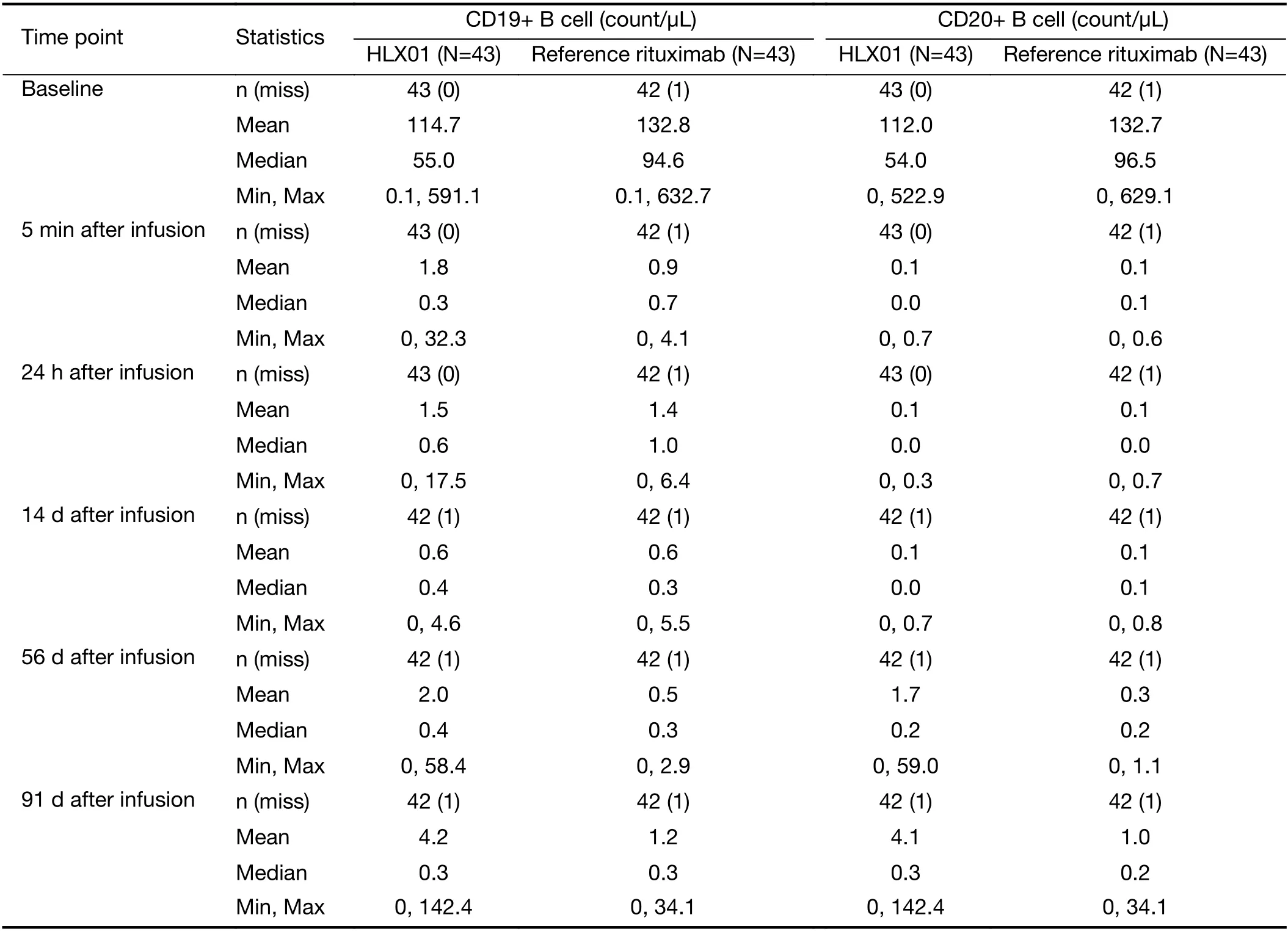
Table 4 Mean changes in peripheral CD19+and CD20+B lymphocyte following HLX01 and reference rituximab administration (phase 1b study)
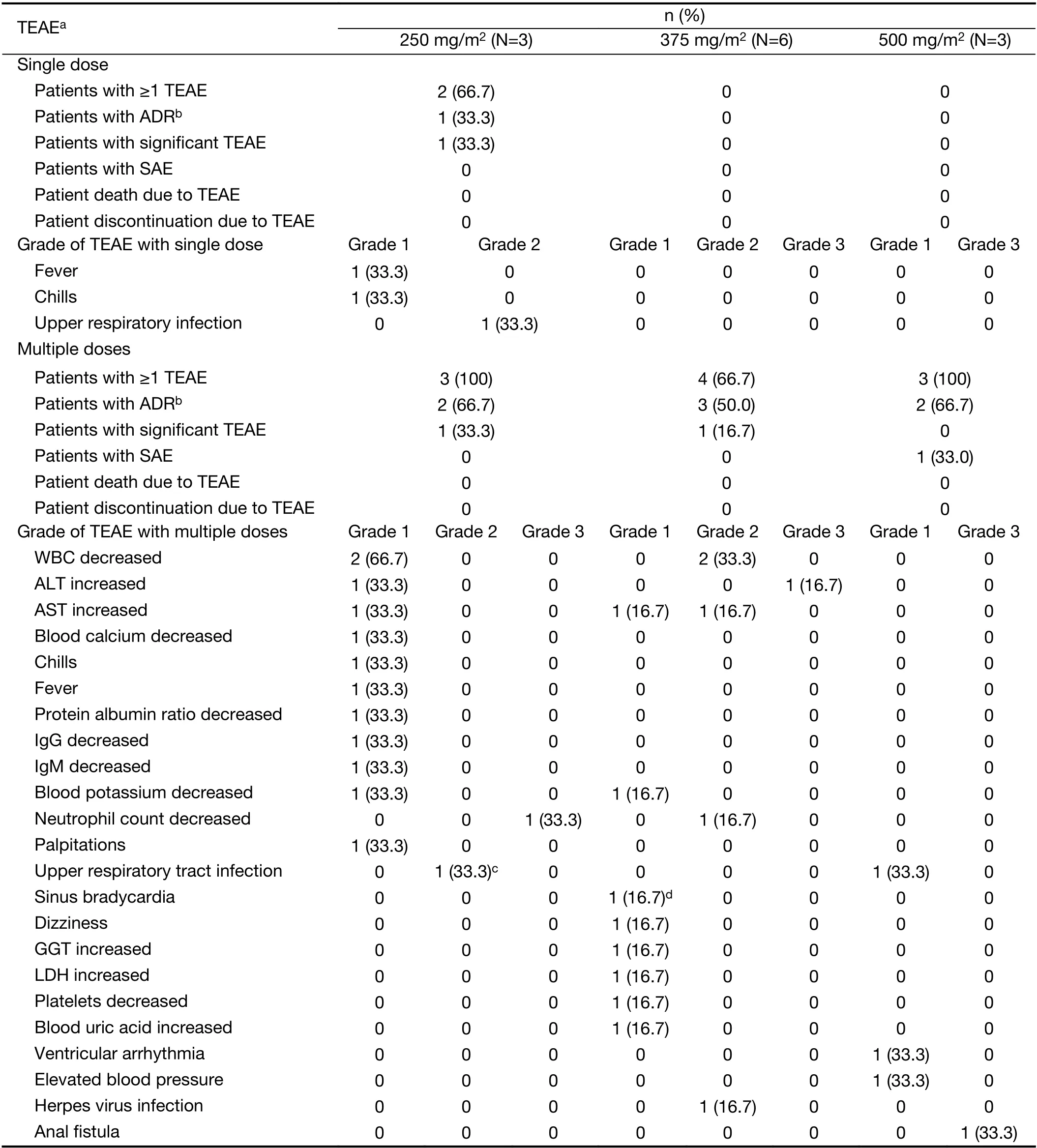
Table S5 TEAEs following single and multiple administrations of HLX01 (phase 1a study)
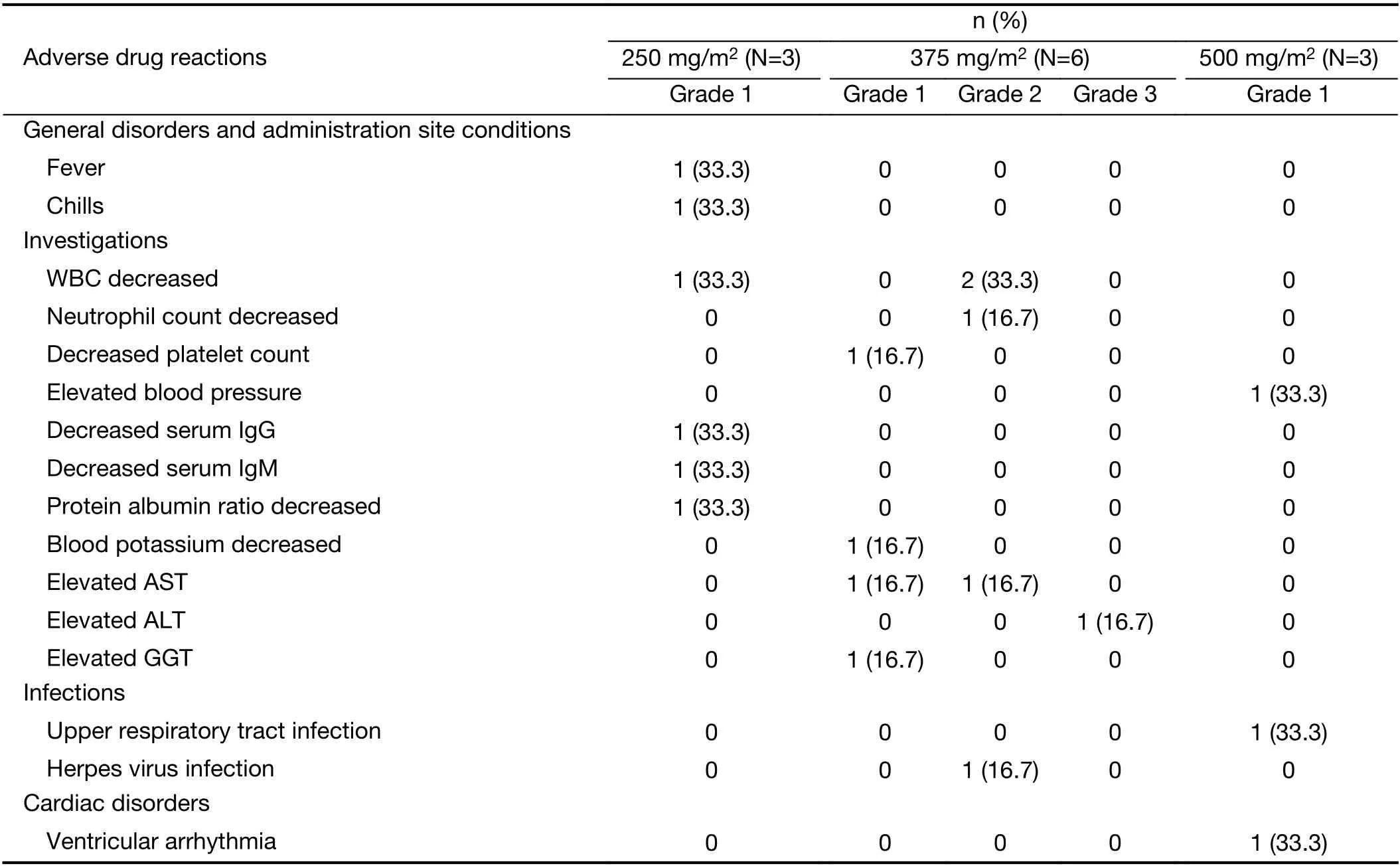
Table S6 Adverse drug reactions following multiple administrations of HLX01 (phase 1a study)
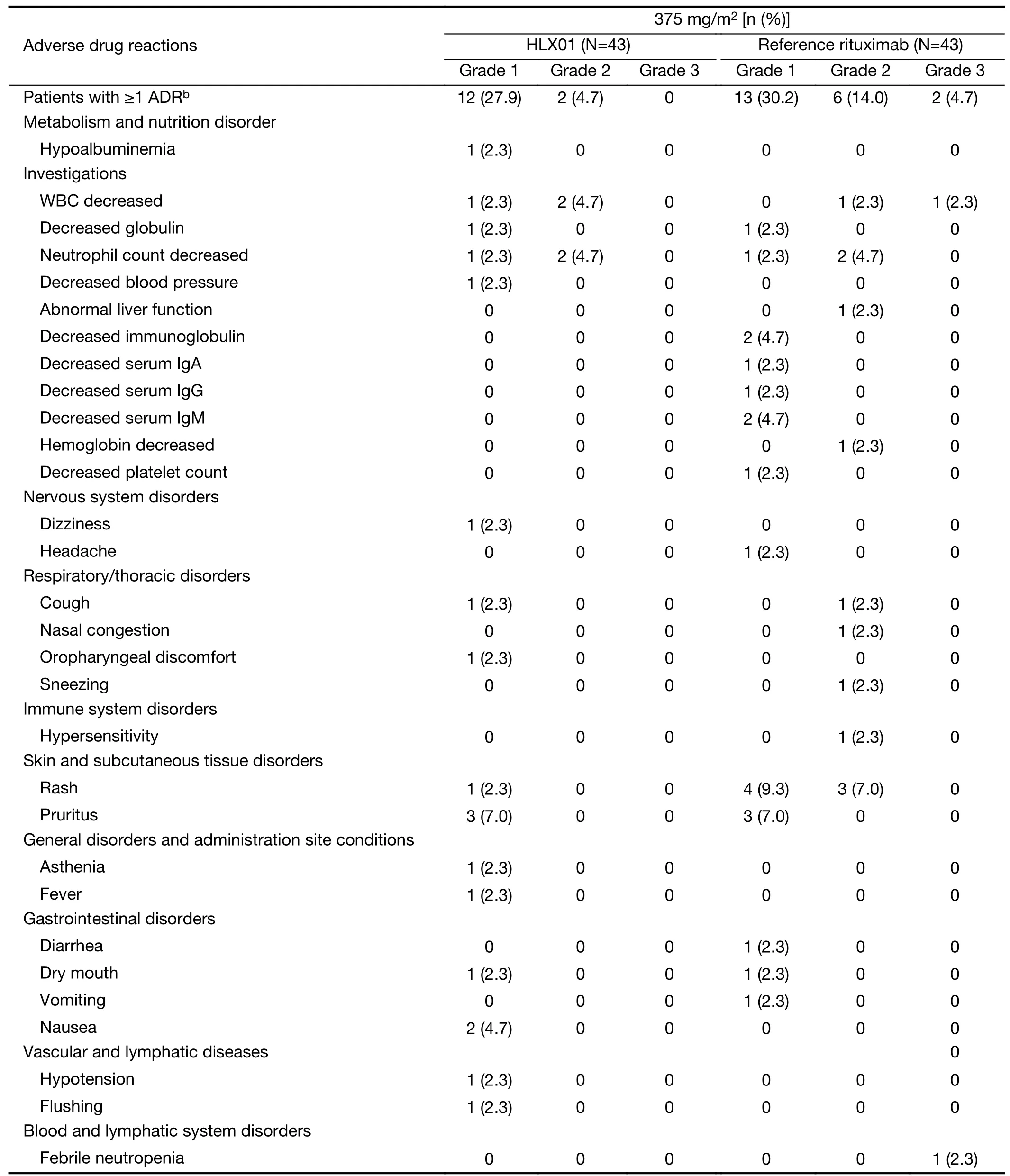
Table S7 Adverse drug reactions following of HLX01 or reference rituximaba (phase 1b study)
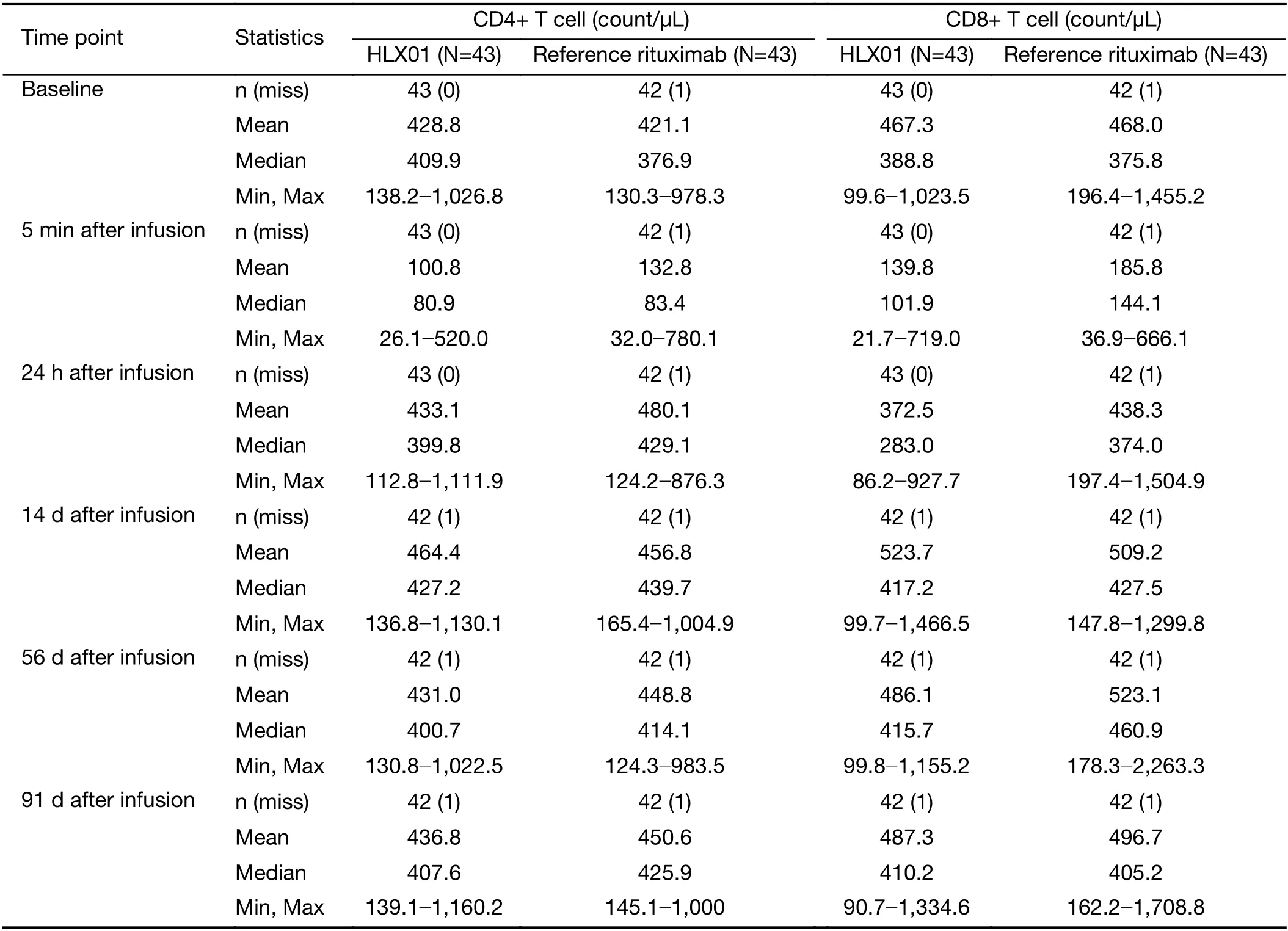
Table S8 Mean changes of circulating CD4+and CD8+T cell pre-and post-treatment (phase 1b study)
Efficacy
All patients enrolled in the phase 1b study who had achieved CR or CRu were evaluable for disease progression following a single dose of HLX01 or rituximab-CN treatment.As of eight weeks after study drug infusion (the final assessment point),the percentage of evaluable patients who remained at CR or CRu was similar in both groups(97.7% in HLX01 group,95.3% in rituximab-CN group,P=1.00).
Discussion
Biologics are complex therapeutic products,requiringcareful manufacturing to ensure homogeneity.Developing biosimilar biologics requires rigorous evaluations to confirm structural and functional similarity to originator products.Controlled clinical trials,using commercially available reference products,are therefore invaluable for confirmation of equivalence of proposed biosimilars and reference products in terms of PK,PD,immunogenicity,safety and efficacy.
HLX01 is the first biosimilar product approved by the NMPA in China.The application for approval was supported by the evidence demonstrating similarity between HLX01 and reference rituximab in terms of their physicochemical properties,biological activities,PK,clinical efficacy and safety (16,18).In the absence of Chinaspecific guidelines prior to 2015,the early clinical development program for HLX01 followed the principles and requirements of the European Medicines Agency(EMA) and the US Food and Drug Administration (FDA)regulatory guidelines for developing and evaluating biosimilar products.The NMPA guidelines that have since been developed are largely consistent with those from the EMA and FDA,and have been adhered to in this study(14,17,19).AUC0-trather than AUC0-infwas chosen as the primary endpoint in the phase 1b study,as it was calculated from actual measured values and was highly recommended by the regulatory authority in China at the time.AUC0-infwas set as a key secondary endpoint in this study.
This initial phase 1a study demonstrated the safety and tolerability of HLX01 in 12 patients.There were no DLTs,and escalating doses of HLX01 were safe and well tolerated,including the recommended therapeutic dose for rituximab (375 mg/m2).PK profiles of escalating doses of HLX01 displayed an expected linear increase and,in agreement with the early phase PK data for referencerituximab and other anti-CD20 monoclonal antibodies,study drug accumulation was observed upon multiple-dose treatment to steady state (20,21).Population PK of the phase 1b study and the data from a phase 3 clinical study(data not shown),have confirmed that age,weight and gender do not have a significant impact on the PK of HLX01.Therefore,the observed differences between baseline characteristics of different groups in the phase 1a study are not anticipated to impact the outcomes.These outcomes provided scientific basis and dose suggestion for patients with NHL in phase 1b study.
The phase 1b study was a comparative PK and safety study of HLX01 and rituximab-CN.The primary(AUC0-91d) and secondary (Cmax) endpoints met the equivalence criteria and demonstrated PK equivalence of HLX01 and rituximab-CN,although the lower 90% CI margin of GLSMR for AUC0-inf(77.7%) was slightly outside the pre-specified equivalence margins(80%-125%).The sensitivity analysis,stratified by the ADA status,further demonstrated PK equivalence of HLX01 and rituximab-CN.
In both studies,HLX01 was safe and well tolerated.Overall,HLX01-related toxicities were as expected from the observations of prior studies of reference rituximab and rituximab biosimilar products,and no new safety concerns were identified (20-24).Most AEs,including IRRs,hematological toxicities and infections were mild (grade ≤2)and did not affect study completion.Fewer ADRs of fever were reported in this study than in a previous phase 1 reference rituximab trial,and no grade 4 (or above) events were reported in this trial (21).Interestingly,the rate of infections in this phase 1b study was relatively low (11.6%)compared to other rituximab biosimilar studies such as GP2013 (21.5%) (25) and PF-05280586 (31.1%) (26),possibly related to the status of enrolled patients.The rates of infections in the HLX01 and rituximab-CN groups were comparable,supporting the conclusion of similarity between the two drugs in terms of safety.
Immunogenicity to biologics may result in reduced treatment efficacy or AEs (27).While ADA development has been previously reported following rituximab therapy(23),all patients in phase 1a study tested negative for ADA over the study duration.Consistent with previous studies(24,27),the incidence of ADA was low and similar in the HLX01 and rituximab-CN groups in the phase 1b trial.
Furthermore,the PD profiles of HLX01 and rituximab-CN were similar with respect to counts of CD19+,CD20+B lymphocytes,and CD4+and CD8+T-cells.There was no difference between the two groups in disease progression at week 8 (final assessment point).
Conclusions
Resultsof the phase 1a and phase 1b studies demonstrate similar PK,PD,safety and immunogenicity profiles between HLX01 and rituximab-CN.HLX01 was safe and well tolerated in Chinese patients with B-cell lymphoma.
Acknowledgements
This study was funded by Shanghai Henlius Biotech,Inc.,Science and Technology Commission of Shanghai Municipality (No.14431908500),and China National Major Project for New Drug Innovation (No.2012ZX09303012).
Footnote
Conflicts of Interest:Xiaodong Dong is an employee of Henlius.Other authors have no conflicts of interest to declare.
 Chinese Journal of Cancer Research2021年3期
Chinese Journal of Cancer Research2021年3期
- Chinese Journal of Cancer Research的其它文章
- Current evidence and challenges of systematic therapies for adult recurrent glioblastoma:Results from clinical trials
- Single-cell DNA methylome analysis of circulating tumor cells
- Prognostic value of a modified Immunoscore in patients with stage I-III resectable colon cancer
- Profiling of hepatocellular carcinoma neoantigens reveals immune microenvironment and clonal evolution related patterns
- A male-ABCD algorithm for hepatocellular carcinoma risk prediction in HBsAg carriers
- Pain threshold,anxiety and other factors affect intensity of postoperative pain in gastric cancer patients:A prospective cohort study
