Correlation of computed tomography findings and lung function in children and adolescents with cystic fibrosis
Andrew Fretzayas· Ioanna Loukou· Maria Moustaki · Konstantinos Douros
Abstract Background The timely and appropriate monitoring of pulmonary status is of utmost importance for patients with cystic fibrosis (CF).Computed tomography (CT) has been used in clinical and research settings for tracking lung involvement in CF patients.However, as CT delivers a considerable amount of radiation, its sequential use in CF patients remains a concern.The application of CT, therefore, should take into account its potential risks.This review aims to understand whether and to what extent the CT findings correlate with the findings from other monitoring tools in CF lung disease.Data sources PubMed was searched for articles about the correlation of chest CT findings with spirometric indices and with lung clearance index in children and adolescents with CF.The most relevant articles were reviewed and are presented herein.Results Most studies have shown that forced expiratory volume in the first second (FEV 1) and other spirometric indices correlate moderately with CT structural lung damage.However, at the individual level, there were patients with FEV 1within the normal range and abnormal CT and vice versa.Furthermore, longitudinal studies have indicated that the deterioration of structural lung damage does not occur in parallel with the progression of lung function.Lung clearance index is a better predictor of CT findings.Conclusions In general, the existing studies do not support the use of lung function tests as surrogates of chest CT.
Keywords Computed tomography · Computed tomography score · Cystic fibrosis · Lung clearance index · Lung function · Spirometry
Introduction
Cystic fibrosis (CF) is a multi-organ genetic disorder, and the major cause of its substantial morbidity and mortality is the progressive lung disease.For this reason, the timely and appropriate monitoring of pulmonary status is mandatory for CF patients.Lung function tests, such as spirometry, in combination with clinical symptoms assessment, are the major tools for the evaluation of CF lung disease.Plain chest radiograph has also been traditionally applied for the detection of pulmonary structural damage in CF.In the 1990s, highresolution computed tomography (HRCT) started to be used for the depiction and monitoring of structural abnormalities, initially in adults and subsequently in children with CF [1, 2].Since then, CT has increasingly been used in clinical and research settings for tracking lung involvement in CF patients owing to the high spatial resolution of this imaging technique.However, because CT delivers a considerable amount of radiation, its sequential use conveys a risk of radiationinduced mortality that is not negligible, especially if we take into account that the survival of CF patients has been increasing [3].It is conceivable that the application of CT should outweigh its potential risks.Consequently, it is important to understand how and to what extent the CT findings correlate with that of other monitoring tools and if CT could be replaced, to some extent, with other risk-free methods.
This narrative review aims to present the correlation of CT findings with spirometric indices of lung function and with lung clearance index in children and adolescents with CF.
Data sources
PubMed was searched for articles on the correlation of chest CT findings with spirometric indices and with lung clearance index in children and adolescents with CF.The literature was searched with PubMed engine from January 1980 since May 2020.Details of our search strategy are summarized in Fig.1.All articles pertinent to the relationship between chest CT findings and lung function parameters were reviewed and are presented herein.
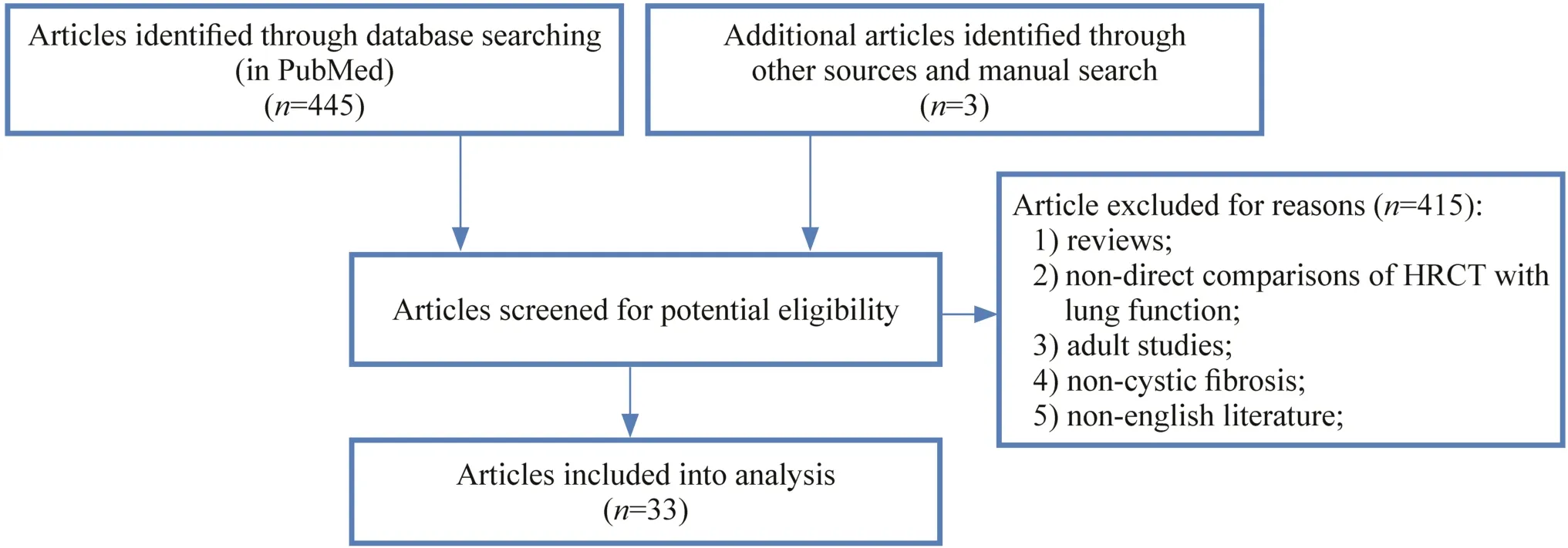
Fig.1 Details of search and selection strategy
CT findings in CF lung disease
The main CT-identified structural lung abnormalities that are observed in the CF are airway wall thickening, mucus plugging, and bronchiectasis.Opacities, such as consolidations and atelectasis, may also be visualized especially during pulmonary exacerbation.Furthermore, bullae, cysts, and air trapping can also be observed sometimes [4, 5].Various scores have been developed to quantify the disease severity and track its progression.The first reported score was developed by Bhalla et al.in 1991 and was based on the evaluation of the degree of bronchiectasis, peribronchial thickening, mucus plugging, sacculations or abscesses, air trapping/emphysema/mosaic perfusion, and collapse/consolidation [6].The score calculation relies on the presence, severity, and extent of the aforementioned abnormalities.Some modifications of this score were published later, namely those of Helbich et al.and Santamaria et al.[7, 8].In 2004, Brody et al.developed a new score that has been widely used since then; it was based on the estimation of extent and severity of bronchiectasis, mucous plugging, peribronchial thickening, parenchymal opacities, and air trapping [9].
All the previously mentioned scores were evaluated in a study of children with CF and were found to have good reliability and reproducibility and to be correlated with each other.However, the scores were not evaluated for their accuracy in classifying the severity of the disease, because an assessment of accuracy was not in the purpose of the study [10].
Recently, three other scores appeared in the literature that aimed at evaluating specific CF populations.The Australian Respiratory Early Surveillance Team (AREST) introduced a score that recorded the presence and extent of bronchiectasis, infl ammatory nodules, bronchial wall thickening, and air trapping in three CT slices on inspiration and expiration, in infants with CF [11].The prevalence of bronchiectasis was 22%, and it increased significantly with advancing age.The Perth-Rotterdam Annotated Grid Morphometric Analysis for CF (PRAGMA-CF) was developed primarily for the estimation of the structural damages of early CF lung disease.The method uses ten CT slices to assess the severity of bronchiectasis, mucous plugging, and other airway abnormalities on inspiratory scans and air trapping on expiratory scans [12].Their score was sensitive and reproducible, and they found a volume lung proportion of structural lung disease ranging from 0 to 10.53%, even in young children and infants (though in the latter group, only a smaller proportion of the lungs was affected).Loeve et al.developed another score specifically aiming at patients with advanced lung disease.The incorporated parameters were infection/infl ammation (bronchiectasis, airway wall thickening, mucous, and consolidations), air trapping/hypoperfusion, bulla/cysts, and normal hyperperfused tissue [4].They found a wide disease spectrum ranging from mainly infection/infl ammation to predominantly air trapping/hypoperfusion.
It should also be mentioned that volumetric acquisition of CT scans can improve the accuracy of CT scores, which are mainly useful for longitudinal follow-up.Furthermore, the matched comparison of inspiratory/expiratory scans allows the precise evaluation of air trapping [13].
Correlation of CT structural abnormalities with spirometric parameters
Several studies have been conducted to investigate the association of CT scores with spirometric parameters.The majority, though not all, of these studies exhibited a signifi-cant correlation between CT score (irrespective of the type of score) and forced expiratory volume in the first second (FEV1) [8, 10, 14- 17].Bhalla et al.who had introduced the first CT score, did not find any correlation between FEV1or forced vital capacity (FVC) and the relevant CT score [6].They commented that the absence of correlation might be attributed to the small sample size (14 patients).Nevertheless, they observed a significant association between the percentage of FEV 1 /FVC ratio and the CT score.Helbich et al.found that the overall CT score correlated significantly with FEV1, whereas its correlation with specific CT findings was weaker [8].Similarly, Demirkazik et al.found that the Bhalla score was significantly correlated with CT findings; this correlation was stronger than the respective correlation between FEV1and the Swachmann-Kulczycki score, which is a scoring system for the overall assessment of the disease including clinical and radiographic points [18].
When the association between pulmonary function and specific radiological findings was explored, the results were controversial.More specifically, Oikonomou et al.used a multivariate model, and showed that the severity of bronchial wall thickening and the extent of atelectasis/consolidation (but not the extent or severity of bronchiectasis) were independently associated with FEV1[17].In contrast to the previous observation, the combination of mosaic perfusion and extent of bronchiectasis explained 58% of FEV1variability in a study conducted by Dakin et al.[16].Conversely, no correlation was noticed between FEV1or FVC and any specific CT finding by Santamaria et al.who, however, did not include mosaic perfusion in the individual components of CT score as Dakin et al.did [7, 16].
In 2004, the five available CT scores were compared in relation to spirometric parameters [10].It was shown that all of these scores were correlated with FEV 1 , FVC, forced expiratory fl ow at 25-75% of FVC (FEF25-75), and FEV1/FVC ratio.The strongest correlations were observed between FEF25-75and FEV1; CT score predicted about 80% and 70% of the variability of FEF25-75and FEV1, respectively.Similar but somewhat weaker partial correlations, ranging from -0.36 for FEF25-75to - 0.46 for FEV1, were found in another study conducted in children with CF [9].Regarding the specific CT findings, only air trapping was found to be associated with both FEF25-75and FEV1.In the 37 out of 60 children with normal pulmonary function tests (above 85% of the predicted values), no significant correlation was found.In the other 23 patients that had at least one abnormal spirometric value, the partial correlations of the air-trapping score with FEV1and FEF25-75were significant.It should be noted that in this study, 14% of participating children had bronchiectasis in > 4 lobes; however, despite this result, the children's spirometric parameters were within the normal range.The latter finding indicates that at the individual level, normal spirometric indices do not preclude the presence of bronchiectasis of substantial extent.In a relatively recent study, it was also found that air trapping on volumetric expiratory chest CT scans correlated significantly with the majority of pulmonary function measures [19].
It is noteworthy, that in a longitudinal study of de Jong et al., the cross-sectional data collected at the beginning of the study revealed a moderate but significant relationship between FEV 1 and CT score [20].However, when after two years, the change of CT scoring and the change of FEV1were compared, no correlation was found.What the investigators observed was that although CT scores had deteriorated significantly (especially the scores for bronchiectasis and mucus plugging), the pulmonary function indices remained stable or even improved.Similar observations were made later by de Jong et al.In a group of 92 patients with CF who had CT scans 3 years apart [21].Specifically, the authors found that bronchiectasis had worsened in 74%, while FEV1had worsened in 58% of the patients; bronchiectasis had deteriorated in 29% of patients whose FEV 1 had remained unchanged or had improved.More recently, findings revealed that CT scores can be used as a better predictor than FEV1the progression of lung disease in the next 2-10 years [22].This observation, however, was not supported by Cademartiri et al.who showed that the high variation in CT scores did not allow the prediction of future pulmonary function test results or the progression of structural abnormalities in the subsequent CT findings [23].Using the PRAGMA-CF method, Svedberg et al.showed that the extent of structural lung disease (SLD) at the age of 7 years correlated significantly with the subsequent progression of SLD; FEV1was only weakly correlated with the progression of FEV 1 decline after the age of 13 years [24].The authors also found a weak association between the rate of decline of FEV1after the age of 7 years and the progression of bronchiectasis.In a recent study from Australia, the CF-CT score of a CT scan obtained at 5-6 years of age was found to be a predictor of the subsequent decline of FEV1z score and could explain 40% of the variation of FEV1 z score 5 years later [25].Among the sub-scores, mucus plugging and air trapping were better predictors of subsequent FEV1decline.The latter observation is important, because both of these findings are potentially reversible with the use of aggressive treatment.
A recent longitudinal study using a volumetric CT scan also showed that quantitative air trapping and mucus plugging increase at 1 and 2 year intervals [26].It is noteworthy that, in this study, the observed decline of FEV1at 3 months was only transient and was resolved by 2 years.
Therefore, it is evident from the aforementioned results that there is wide variation in the reported correlations between FEV1and other spirometric indices with chest structural damage.This can be explained partly by the broad range of FEV1values, being either normal or abnormal, that were included in the samples of the studies reviewed.Concerning the individual cases, it is obvious that discordance between CT scan findings and pulmonary function tests occurs frequently; many patients with normal FEV1and significant structural damages in the CT have been described.It is assumed that because the FEV1is calculated as the percentage of the predicted or as a z score on the basis of large population samples, values within normal range do not necessarily refl ect normality for a specific individual given that his/her potential may be higher than the conventionally defined normal range of values.However, this explanation is not wholly convincing.Jong et al.showed a deterioration of CT scores with stable or improved pulmonary function tests or improved CT scores with deteriorating lung function tests [21].It is also a matter of debate as to whether forced expiratory fl ow at 75% of the FVC (FEF75) or FEF25-75could probably correlate better with early structural damage occurring in the small airways, as it was suggested by Tiddens, given that the variability of these parameters is considerable [27, 28].In general, it is acknowledged that FEF 25-75 adds little information for clinical decision-making over what is provided by FEV1, FVC, and FEV1/FVC ratio [29].
Overall the above evidence suggests that FEV1or any other spirometric index cannot be considered as a surrogate for CT findings in children with CF.
The correlation of CT structural abnormalities with lung clearance index
Although spirometry is the main pulmonary function test for monitoring CF lung disease, it needs the cooperation of the examined subjects and, therefore, is usually applicable in children older than 6 years of age [30].During the last decade, multiple washout methods have been used-especially in children younger than 6 years old-taking advantage of the fact that cooperation is not necessary [31, 32].The main parameter derived from this technique is lung clearance index (LCI), which is an indicator of uneven ventilation distribution [31].The first study that compared the sensitivities of LCI and spirometry on the prediction of CT structural abnormalities showed that the sensitivity of LCI ranged from 85 to 94% for the detection of bronchiectasis, air trapping, and total CT score, whereas the respective sensitivities of FEV1 and FEF75ranged from 19 to 26% and 62-75%, respectively [33].Ellemunter et al.subsequently evaluated the relevant LCI sensitivity in patients with CF and normal FEV1(> 80% predicted) and found comparable results, with the sensitivity and specificity of LCI being 88% and 63%, respectively [34].Fuchs et al.evaluated the progression of FEV1, LCI, and CT scores performed 3 years apart in children and adolescents with an initial annual average of FEV1> 80% [35].They found a significant correlation of Bhalla score with LCI but not with FEV1.Furthermore, the initial LCI value was correlated with the Bhalla score of the CT performed 3 years later, whereas FEV1was not.
In a recent study that was performed in children and adolescents with CF and did not include spirometry, Yammine et al.found a significant correlation between LCI and the extent of bronchiectasis in volumetric CT scan [36].A weaker but significant correlation of LCI with mucous plugging also was observed.However, other authors that compared LCI with chest CT in infants with CF did not find any significant relationship between LCI values and the presence of bronchiectasis or air trapping (using volumetric CT scan).Their only significant finding was that LCI was moderately correlated with the extent of air trapping [37].Ramsey et al.evaluated the relationship of LCI values with structural damage in chest volumetric CT across the entire age spectrum from infancy to adolescence [38].The authors observed that the positive predictive value of LCI for bronchiectasis in infancy was only 18%, whereas in preschool and school-aged children, the positive predictive value was more than 80%.
It seems, therefore, that in CF patients, the LCI values obtained using chest CT are correlated much better than FEV1with the lung structural damage.This result is more evident when FEV1lies within the normal range of values.In infancy, however, the LCI is a rather insensitive predictor at least as far as it regards the presence of bronchiectasis.LCI remains mainly a research tool and cannot substitute for the CT scan, especially in infancy.More longitudinal studies are needed to understand better the relationship of LCI with CT scores and the association of progression of LCI with the respective progression of CT findings.
CT and radiation risk
Serial chest CT in subjects with CF is debatable due to the increased exposure to ionizing radiation.During the past 30 years, the mean annual effective radiation dose has increased from 0.39 mSV to 1.67 mSV per person per year [39].A patient with CF aged 17 years have been exposed to the radiation of a chest CT scan nine times if a protocol of biennial chest CT scans is followed.This is equivalent to a radiation dose of 20 mGY in total and conveys a cancer mortality risk of 0.2% [40].This risk is low, but as the life expectancy of CF patients increases the risk becomes a non-negligible issue [3].Thus, the benefits from chest CT scans should always outweigh the potential risk.There are no universal recommendations for the optimal frequency of chest CT acquisition in CF patients.Many CF centers adopt the biennial chest CT scan.In our institution, an initial chest CT scan is obtained at the age of 5-6 years; thereafter, a scan usually is obtained every 7-8 years.CT scans are performed earlier only if clinically indicated.
Conclusions
The above-mentioned studies indicate that lung function tests, namely spirometry and LCI, should be considered as imperfect surrogates of either the presence or the severity of chest structural lung damage.Furthermore, CT scan findings predict more accurately the progression of CF lung disease in the long term.This is not, however, an adequate reason for performing chest CT imaging in children with CF on a routine basis owing to the health risks associated with radiation exposure.On the other hand, CT imaging is often necessary for the appropriate tailoring of treatment.The optimal intervals of chest CT reiteration in patients with CF have not been yet determined.In the near future, standardization of chest MRI imaging, either non-contrast-enhanced MRI or hyperpolarized gas MRI, is expected to provide a substitute for CT in monitoring structural lung damage progression in CF patients.
Author contributionsDr.Loukou and Dr.Moustaki wrote the initial draft.Prof Fretzayas and Assoc.Prof Douros critically revised the manuscript.All authors approved the final version of the manuscript.
FundingNo financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Compliance with ethical standards
Ethical approvalEthical approval non-applicable.
Conflict of interestNo confl ict of interest to be declared.
 World Journal of Pediatrics2021年3期
World Journal of Pediatrics2021年3期
- World Journal of Pediatrics的其它文章
- COVID-19 ocular findings in children: a case series
- Associations between measures of pediatric human resources and the under-five mortality rate: a nationwide study in China in 2014
- Genetic etiologies associated with infantile hydrocephalus in a Chinese infantile cohort
- Hedgehog signaling pathway gene variant influences bronchopulmonary dysplasia in extremely low birth weight infants
- Causes of severe neonatal hyperbilirubinemia: a multicenter study of three regions in China
- Maternal mental health and well-being during the COVID-19 pandemic in Beijing, China
