Therapeutic efficacy observation of acupuncture plus medicine for laryngopharyngeal reflux due to liver-qi stagnation and spleen deficiency
Zhao Jing (赵静), Wang Yi (王轶), Yang Cui-rong (杨翠蓉), Lou Qing (娄青)
First Affiliated Hospital of Chengdu Medical College, Chengdu 610500, China
Abstract Objective: To observe the clinical efficacy of acupuncture plus medicine in treating laryngopharyngeal reflux due to liverqi stagnation and spleen deficiency.
Keywords: Acupuncture Therapy; Acupuncture Medication Combined; Laryngopharyngeal Reflux; Liver-qi Stagnation and Spleen Deficiency; Esophageal Motility Disorders; Randomized Controlled Trial
Laryngopharyngeal reflux (LPR) is a common otolaryngology disease caused by reflux stimulation of gastric contents and damage to the throat mucosa,which is characterized by foreign body sensation in throat, hoarseness and chronic cough[1-2]. The incidence is high, and about 10% of the outpatients in the department of otolaryngology have throat reflux[3]. At present, the preferred medicine internationally recognized is proton pump inhibitors, which can be used as the diagnostic treatment of LPR. However, long-term use of proton pump inhibitors can lead to the loss of vitamin C, inhibit the bioavailability of vitamin B12,reduce the absorption of hemoglobin iron in the diet,and increase the risk of osteoporotic fractures[4-6]. In this study, we used acupuncture plus medicine to treat patients with LPR due to liver-qi stagnation and spleen deficiency, and compared with patients treated only by medication.
1 Clinical Materials
1.1 Diagnostic criteria
The diagnostic criteria in Western medicine in this study referred the Experts Consensus on Diagnosis and Treatment of Laryngopharyngeal Reflux Disease (2015)[7],and considered the 24-hour laryngopharyngeal esophageal pH monitoring as the gold standard for the diagnosis of LPR. It could be diagnosed if the acid reflux events in 24 h ≥3 times, or the total time of the laryngopharyngeal pH value less than 4 ≥1%, or the 24-hour laryngopharyngeal reflux area index >6.3.
According to theGuiding Principles for Clinical Study of New Chinese Medicines[8], criteria for traditional Chinese medicine (TCM) syndrome differentiation of liver-qi stagnation and spleen deficiency in this study were established. Primary manifestations: foreign body sensation in the throat or acid regurgitation, emotional anxiety or depression, anorexia, tiredness and weakness.Secondary manifestations: hypochondriac distending pain, distension and oppression in the stomach, bitter taste in the mouth and dry throat, a pale tongue with thin and white coating, string-like pulse.
1.2 Inclusion criteria
Those who met both diagnostic criteria in Western medicine and syndrome differentiation of TCM; aged 20-60 years; agreed to participate in this trial and signed informed consents.
1.3 Exclusion criteria
Those with malignant tumors of the digestive tract;women during pregnancy or breastfeeding; who had cachexia; those with severe heart, lung, liver or kidney diseases; those who were allergic to the medications in the trial.
1.4 Dropout criteria
Those who dropped out or had other therapies; those presenting with severe adverse reactions; those with incomplete data.
1.5 Statistical methods
All data were statistically analyzed by the SPSS version 20.0 statistical software. Counting data were processed by Chi-square test. Measurement data in normal distribution and having homogeneous variance were expressed as mean ± standard deviation (±s), and analyzed byt-test. If data did not meet normal distribution or haven’t homogeneous variance, nonparametric test was applied.P<0.05 was considered to indicate a statistically significant difference.
1.6 General data
A total of 70 patients with LPR were enrolled from the Clinic of the First Affiliated Hospital of Chengdu Medical College, between January 2017 and December 2018. The patients were randomly divided into a control group and an observation group by the random number table method, with 35 cases in each group. During the treatment, 3 patients in the control group dropped out due to traffic reasons, and 2 cases in the observation group dropped out due to work reasons. There were no statistically significant differences in the general data between the two groups (allP>0.05), indicating that the two groups were comparable (Table 1).
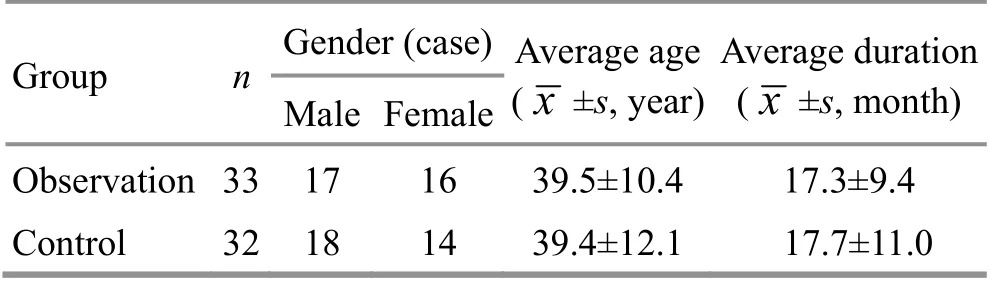
Table 1. Comparison of general data between the two groups
2 Treatment Methods
2.1 Control group
The control group was treated with conventional treatment, oral omeprazole enteric-coated capsules[State Food and Drug Administration (SFDA) Approval No.H20056577, Youcare Pharmaceutical Group Co., Ltd.,China], 20 mg/time, twice a day, 4 weeks in total.
2.2 Observation group
The observation group received acupuncture plus medicine, and the medication was the same as in the control group.
Acupoints: Tiantu (CV 22), Shangwan (CV 13), Zusanli(ST 36), Sanyinjiao (SP 6) and Taichong (LR 3).
Methods:After routine disinfection, Tiantu (CV 22)was perpendicularly punctured by 0.2 cun in depth with an acupuncture needle of 40 mm in length, then the tip of the needle was turned downwards and punctured by about 1 cun in depth along the posterior wall of sternum.Shangwan (CV 13), Zusanli (ST 36) and Sanyinjiao (SP 6)were perpendicularly punctured by about 1 cun in depth with acupuncture needles of 40 mm in length. Taichong(LR 3) was perpendicularly punctured by about 0.5 cun in depth with an acupuncture needle of 25 mm in length.Even reinforcing-reducing manipulation was applied, and the needles were retained for 30 min. The treatment was performed once every other day, for 4 weeks in total.
3 Observation of Curative Efficacy
3.1 Observation items
3.1.1 Reflux symptom index (RSI)
RSI was used to evaluate the severity of LPR before and after treatment. The RSI score ranged from 0 to 45 points. The higher the score, the more severe the symptoms[9].
3.1.2 Reflux finding score (RFS)
Before and after treatment, the patients were examined by laryngoscopy, and RFS scale was scored.The RFS scale included the evaluation of 8 physical signs such as false vocal cord groove, disappearance of ventricle of larynx, erythema and congestion, and vocal cord edema. The RFS score ranged from 0 to 26 points.The higher the score, the more severe the findings of laryngoscopy[10].
3.1.3 Esophageal motility index
Before and after treatment, the solid-state highresolution pressure measurement system was used to measure the lower esophageal sphincter pressure (LESP)and upper esophageal sphincter pressure (UESP).
3.1.4 Salivary pepsin level
Before and after treatment, 1-2 mL of throat saliva coughed out by patients was taken, and the salivary pepsin level was measured by enzyme-linked immunosorbent assay.
3.2 Criteria of curative efficacy
According to the Experts Consensus on Diagnosis and Treatment of Laryngopharyngeal Reflux Disease (2015)[7],the curative efficacy was evaluated.
Markedly effective: The symptoms basically disappeared. RSI ≤13 points.
Effective: The symptoms were significantly improved.RSI decreased, but was still over 13 points.
Invalid: The symptoms had no improvement, and the RSI score had no decrease.
3.3 Results
3.3.1 Comparison of therapeutic efficacy
The effective rate was 93.9% in the observation group,and 75.0% in the control group. The effective rate of the observation group was higher than that of the control group (P<0.05), (Table 2).

Table 2. Comparison of therapeutic efficacy between the two groups (case)
3.3.2 Comparison of RSI score
Before treatment, there was no significant difference in the RSI score between the two groups (P>0.05). After treatment, the RSI scores in both groups decreased (bothP<0.05), and the RSI score in the observation group was lower than that in the control group (P<0.05), (Table 3).
3.3.3 Comparison of RFS score
Before treatment, there was no significant difference in the RFS score between the two groups (P>0.05). After treatment, the RFS scores in both groups decreased(bothP<0.05), and the RFS score in the observation group was lower than that in the control group (P<0.05),(Table 4).
3.3.4 Comparison of esophageal motility index
Before treatment, there were no significant differences in LESP and UESP between the two groups(bothP>0.05). After treatment, the LESP and UESP in the observation group significantly increased (bothP>0.05),and were higher than those in the control group (bothP<0.05), (Table 5).
3.3.5 Comparison of salivary pepsin level
Before treatment, there was no significant difference in salivary pepsin level between the two groups (P>0.05).After treatment, the salivary pepsin levels in both groups decreased (bothP<0.05), and the salivary pepsin level in the observation group was lower than that in the control group (P<0.05), (Table 6).
Table 3. Comparison of RSI score between the two groups(±s, point)

Table 3. Comparison of RSI score between the two groups(±s, point)
Note: Compared with the same group before treatment, 1) P<0.05;compared with the control group after treatment, 2) P<0.05
Group n Observation 33 Control 32 Before treatment After treatment22.39±5.29 12.33±4.051)2)21.41±5.28 16.03±4.481)
Table 4. Comparison of RFS score between the two groups(±s, point)

Table 4. Comparison of RFS score between the two groups(±s, point)
Note: Compared with the same group before treatment, 1) P<0.05;compared with the control group after treatment, 2) P<0.05
Group n Before treatment After treatment Observation 33 14.33±2.79 8.67±2.041)2)Control 32 15.03±2.53 11.00±1.881)
Table 5. Comparison of esophageal motility index between the two groups (±s, mmHg)

Table 5. Comparison of esophageal motility index between the two groups (±s, mmHg)
Note: 1 mmHg=0.133 kPa; BT=Before treatment; AT=After treatment; compared with the same group before treatment, 1)P<0.05; compared with the control group after treatment, 2) P<0.05
Group n Time LESP UESP Observation 33 BT 17.94±3.65 54.94±15.61 AT 23.37±5.441)2) 63.80±15.871)2)Control 32 BT 18.09±4.45 50.34±14.02 AT 18.35±3.87 54.15±13.72
Table 6. Comparison of salivary pepsin level between the two groups (±s, μg/L)

Table 6. Comparison of salivary pepsin level between the two groups (±s, μg/L)
Note: Compared with the same group before treatment, 1) P<0.05;compared with the control group after treatment, 2) P<0.05
Group n Before treatment After treatment Observation 33 122.51±44.43 67.99±28.281)2)Control 32 116.40±39.22 91.05±37.421)
4 Discussion
In TCM, LPR falls under the category of Hou Bi (throat impediment), Hou Yin (hoarseness) and Mei He Qi(globus hystericus). The location of LPR is in the throat and esophagus, and it is closely related to liver, spleen and stomach. Liver-qi stagnation and spleen deficiency is the key pathogenesis of this disease. The liver governs conveyance and dispersion, regulating qi movement and mood. If the liver loses its function of conveyance and dispersion, the qi movement will be blocked, which will affect the transportation and transformation of the spleen and stomach, and the ascending-descending function of qi movement. The essence transformed by spleen and stomach therefore cannot nourish the throat,and the reversed flow of qi impregnates the throat with turbid qi, which leads to the occurrence of this disease[11-12]. Therefore, TCM treatment emphasizes soothing the liver and fortifying the spleen, descending the reverse qi for harmonizing the stomach.
In this study, Tiantu (CV 22), Shangwan (CV 13), Zusanli(ST 36), Sanyinjiao (SP 6) and Taichong (LR 3) were selected as the main points. Tiantu (CV 22) is near the throat, with the effects of regulating qi and descending the reverse qi, clearing throat and relieving cough.Acupuncturing Tiantu (CV 22) can inhibit throat reflux by affecting the function of the upper esophageal sphincter[13]. Shangwan (CV 13) has effects of regulating the spleen and stomach, dispersing the stagnated liverqi and descending the reverse qi. It is close to the upper gastric aperture cardia and can regulate esophageal peristalsis[14]. Zusanli (ST 36) is the He-Sea point of the Stomach Meridian, and can invigorate the spleen for harmonizing the stomach, unblock meridians and activate collaterals, and regulate the ascendingdescending of the qi movement. Sanyinjiao (SP 6) is the crossing point of the Spleen Meridian, Liver Meridian and Kidney Meridian, with effects of invigorating the spleen and dispersing the stagnated liver-qi, benefiting the kidney and nourishing yin. Taichong (LR 3) is the Yuan-Primary point of the Liver Meridian, with effects of dispersing stagnated liver qi for relieving depression, and activating qi for lowering the reverse qi. Acupuncturing the above acupoints could disperse the stagnated liverqi for descending the reverse qi flow, invigorate the spleen and benefit the throat.
In this study, the effective rate of the observation group was higher than that of the control group. After treatment, the RSI and RFS scores in both groups decreased significantly, and the scores in the observation group were significantly lower than those in the control group. RSI reflects the severity of LPR symptoms, and RFS represents the severity of throat signs. The results indicated that acupuncture plus medicine had a certain effect of improving both clinical symptoms and signs in patients with LPR, and the efficacy was superior to that of pharmacological treatment alone.
In this study, we objectively monitored esophageal motility indicators such as LESP and UESP. The reflux of stomach contents to the throat needs to pass through four barriers, the lower esophageal sphincter,esophageal clearance ability, upper esophageal sphincter,and the anti-acid capability of the throat mucosa[15]. The values of LESP and UESP reflect the anti-reflux barrier function of lower esophageal sphincter and upper esophageal sphincter. When the lower esophageal sphincter is loose and with low pressure, the gastric contents are easily refluxed into the esophagus. When the upper esophageal sphincter is loose or its pressure drops, the esophageal reflux is easy to flow back to the throat, resulting in laryngopharyngeal inflammation[16-17].Results in this study showed that the values of LESP and UESP in the control group had no significant changes after treatment, while the values in the observation group had significant increase and were higher than those in the control group. It suggested that acupuncture significantly improves esophageal motility, which might be related to the remarkable effect of acupuncture plus medicine in LPR treatment.
In this study, the salivary pepsin level was also measured. Pepsin is an indispensable proteolytic enzyme in the digestive system, and it is also the main injury factor of LPR. With the reflux event, pepsin enters the throat. Activated pepsin will make the intracellular mitochondrion swollen, the mitochondrial crista become shallow, and the mitochondrial matrix widened, and finally the mucosal cells of the throat are damaged[18-19].Meanwhile, pepsin also promotes the rupture of mitochondrial respiratory chain, resulting in increased production of reactive oxygen species in the mitochondrion, putting the throat mucosa in a state of oxidative stress, causing and aggravating the inflammatory response of the throat mucosa, and damaging the throat epithelium[20-21]. Results in this study showed that the salivary pepsin levels in both groups decreased after treatment, and the salivary pepsin level in the observation group was lower than that in the control group. It suggested that acupuncture plus medicine could significantly reduce the salivary pepsin level, which might be related to its remarkable effect.
In summary, acupuncture plus medicine can produce significant efficacy for LPR due to liver-qi stagnation and spleen deficiency. It can improve the symptoms and signs,and regulate esophageal motility and salivary pepsin level. It is worth clinical promotion.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
This work was supported by Project of Hunan Province Administration of Traditional Chinese Medicine (湖南省中医药科研计划项目, No. 2019138).
Statement of Informed Consent
Informed consent was obtained from all individual participants.
Received: 30 March 2020/Accepted: 9 July 2020
 Journal of Acupuncture and Tuina Science2021年3期
Journal of Acupuncture and Tuina Science2021年3期
- Journal of Acupuncture and Tuina Science的其它文章
- Efficacy of acupuncture in treating chronic non-specific low back pain
- Clinical efficacy observation on pediatric massage for chronic cough in children
- Clinical study of warm needling moxibustion plus intra-articular injection of sodium hyaluronate for chondromalacia patellae
- Effects of acupuncture plus spinal manipulations on physical functioning and biochemical indicators in patients with ankylosing spondylitis
- Effect of mild moxibustion on cancer-related fatigue,serum ghrelin and adiponectin in patients undergoing chemotherapy after colorectal cancer surgery
- Clinical efficacy observation of acupoint threadembedding in treating obese patients with food addiction
