Clinical study of warm needling moxibustion plus intra-articular injection of sodium hyaluronate for chondromalacia patellae
Liu Xiao-hui (刘晓慧), Ye Ya-yun (叶亚云)
Lishui People’s Hospital, Zhejiang Province, Lishui 323000, China
Abstract Objective: To observe the therapeutic efficacy of warm needling moxibustion plus intra-articular injection of sodium hyaluronate in treating chondromalacia patellae and its effect on inflammatory factors in knee joint fluid.
Keywords: Acupuncture Therapy; Warm Needling Therapy; Injections, Intra-articular; Hyaluronic Acid; Chondromalacia Patellae; Osteoarthritis, Knee; Inflammatory Cytokines
Chondromalacia patellae (CP) is a type of osteoarthropathy pathologically characterized by swelling, weakness or fragmentation of the patellar cartilage along with subchondral bone exposure,proliferation or osteosclerosis, mainly manifesting as anterior knee pain, knee joint swelling and limited range of motion[1]. The incidence of CP is approximately 36.2%in China reportedly, but higher in women and athletes performing lots of knee joint activities[2]. At the advanced stage, osteonecrosis and cystic lesions or extensive osteophyte around the cartilage may occur, resulting in intense pain and significantly affecting joint function[3].Currently, early-stage CP is majorly treated with conservative methods such as intra-articular injection of sodium hyaluronate. Surgical treatment is adopted when conservative treatments didn’t achieve a satisfactory result, including sagittal patellar osteotomy and lateral patellar retinaculum release[4].
Acupuncture-moxibustion treatment has been quite popular in treatment of osteoarthropathy like knee osteoarthritis and capsulitis of the shoulder, since it’s found effective in reducing pain and improving joint function[5-6]. In this study, we treated CP with warm needling moxibustion plus intra-articular injection of sodium hyaluronate and observed its efficacy and inflammatory factors in knee joint fluid including nuclear factor-κB (NF-κB), tumor necrosis factor (TNF)-α and interleukin (IL)-1β. The report is given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
The diagnostic criteria for CP were made based on theClinical Guidelines on Diagnosis and Treatment:Orthopedics[7]: usually had a history of trauma or strain;younger people are more likely to be affected; pain in the knee joint was the major complaint with friction sound produced beneath the patella when flexing and extending the affected knee, or presenting ‘leg weakness’or ‘pseudo-interlocking’ signs; physical examination found pain in knee extension against resistance test,positive result in patella grind test and infrapatellar fat pad tenderness; magnetic resonance imaging (MRI)showed altered patellar cartilage surface or abnormal signals in patellar cartilage.
1.2 Inclusion criteria
Conformed to the above diagnostic criteria for CP;ages between 18-60 years old; not taking any medications or other treatments in the previous week;unilateral CP; willing to participate in the study.
1.3 Exclusion criteria
Coupled with meniscus injury, ligament injury, bone tumor or bone tuberculosis; bilaterally affected;pregnant women or women during lactation; unable to stick with the treatment.
1.4 Dropout criteria
Those showed severe adverse reactions; those who quitted on their own; those took other medications or treatments without permission.
1.5 Statistical methods
Data analysis was performed using SPSS version 21.0 software. Measurement data with normal distribution and homogeneity of variance were expressed as mean ±standard deviation (±s), and checked using paired samplest-test in intra-group comparisons or independent samplest-test in between-group comparisons. Measurement data not conforming to normal distribution or homogeneity of variance were examined by non-parametric test. Numeric data were processed by Chi-square test and ordinal data by rank sum test. Statistical significance was recognized whenP<0.05.
1.6 General data
Sixty-eight CP patients who visited Lishui People’s Hospital, Zhejiang Province between August 2016 and September 2018 were selected and allocated to a control group and an observation group using the random number table method, with 34 cases in each group.There were no dropout cases during treatment in either group. Between-group comparison of the data of gender,age and disease duration showed no significant difference (allP>0.05), suggesting the comparability(Table 1).
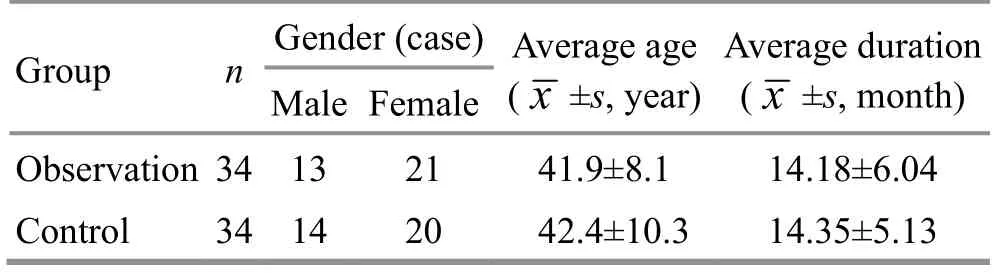
Table 1. Comparison of general data
2 Treatment Methods
2.1 Control group
The control group received intra-articular injection of sodium hyaluronate.
Operation: Sodium hyaluronate injection [State Food and Drug Administration (SFDA) Approval No.H20051837, Shanghai Haohai Biological Technology Co.,Ltd., China] was adopted. The patient took a supine position with two legs extended. After standard sterilization, the medial center spot of the patella was punctured by 15-20° between the needle and body surface. A hollow sensation suggested that the tip of the needle had reached inside the articular cavity and 2 mL sodium hyaluronate injection was injected. If there was effusion, it needed to be eliminated completely ahead.The topical was covered by sterile dressings after injection. Then, passively flexed and extended the knee for 3-5 times to evenly distribute the injection inside the articular cavity. The treatment was performed once a week, for 5 weeks in total.
2.2 Observation group
The observation group was given additional warm needling moxibustion treatment.
Acupoints: Xuehai (SP 10), Liangqiu (ST 34), Dubi(ST 35) and Neixiyan (EX-LE 4) on the affected side, and bilateral Sanyinjiao (SP 6) and Taichong (LR 3).
Operation: The patient took a supine position with the knees flexed by 90° and fully exposing topical skin. Hwato brand sterile acupuncture needles of 0.25 mm in diameter and 40 mm in length (Suzhou Medical Appliance Factory, China) were used. After routine sterilization, with nail-pressing method, Xuehai (SP 10)and Liangqiu (ST 34) were punctured perpendicularly for 0.8-1.0 cun; Dubi (ST 35) was punctured obliquely towards the medial side (inside the articular cavity) for 0.5-1.0 cun; Neixiyan (EX-LE 4) was punctured towards the articular cavity as well for 0.5-1.0 cun; and Sanyinjiao(SP 6) and Taichong (LR 3) were punctured perpendicularly for 0.5-0.8 cun. When needling qi was obtained, even reinforcing-reducing manipulation was performed and the needles were retained for 30 min.During needle-retaining, each needle handle was stuck into one segment of moxa stick of 15 mm long and 10 mm in diameter, for warm needling moxibustion. Put a piece of cardboard between the moxa and skin to prevent from burns. The moxa was ignited from the bottom and the needles were removed when the moxa was completely burnt out. Warm needling moxibustion treatment was performed once a day, 5 times a week, for 5 weeks in total.
3 Observation of Therapeutic Efficacy
3.1 Outcome measures
3.1.1 Western Ontario and McMaster Universities osteoarthritis index (WOMAC)
The two groups were scored using WOMAC before and after treatment. WOMAC observes three domains including pain, stiffness and daily activities using 24 items. A higher WOMAC score means more serious CP symptoms[8].
3.1.2 Time cost for climbing up and down one staircase and pain intensity
Before and after treatment, the patients were asked to make their best effort to climb up and down one staircase within their endurance of pain. The cost of time was recorded and the immediate pain intensity was evaluated using visual analog scale (VAS).
3.1.3 MRI grading
All the patients were checked using MRI to determine the grade of CP and objectively evaluate the severity.Grade Ⅰ: changes in signal intensity of the articular cartilage; grade Ⅱ: abnormal signals suggesting swelling in the articular cartilage; grade Ⅲ: irregular and thinner cartilage; grade Ⅳ: cartilage defects,subchondral osteosclerosis or cystic degeneration[9-10].
3.1.4 Levels of NF-κB, TNF-α and IL-1β in knee joint fluid
Knee joint fluid was extracted before and after treatment to determine the levels of NF-κB, TNF-α and IL-1β using enzyme-linked immunosorbant assay.
3.2 Criteria for efficacy evaluation
The efficacy evaluation criteria referred theCriteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine[11].
Clinical recovery: Knee pain was basally gone, without obvious discomfort during movement and patella grind test turned negative.
Improved: There was mild pain during climbing up and down stairs and semi-squatting, while patella grind test showed weak positive.
Invalid: Symptoms didn’t show notable improvements or even became worse.
3.3 Results
3.3.1 Comparison of therapeutic efficacy
The total effective rate was 94.1% in the observation group versus 70.6% in the control group, and the between-group difference was statistically significant(P<0.05). The details are shown in Table 2.
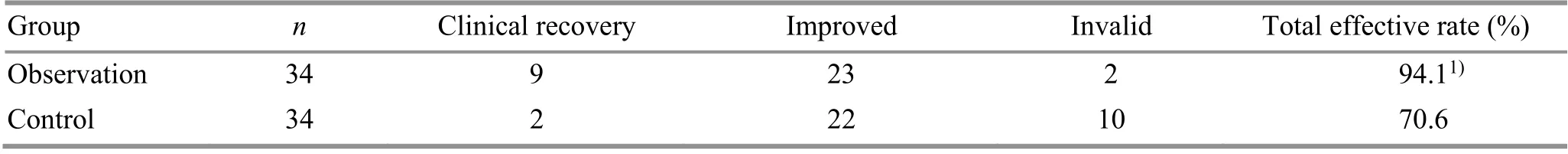
Table 2. Comparison of clinical efficacy between the two groups (case)
3.3.2 Comparison of WOMAC score
Before treatment, there were no significant betweengroup differences in the scores of pain, stiffness and daily activities and WOMAC general score (allP>0.05). After treatment, the scores of pain, stiffness and daily activities and WOMAC general score decreased significantly (allP<0.05), and were lower in the observation group than in the control group (allP<0.05),(Table 3).
3.3.3 Comparison of the time cost for climbing up and down one staircase and VAS score
Prior to treatment, there were no significant differences in the time cost for climbing up and down one staircase and VAS score between the two groups(bothP>0.05). After treatment, the time cost for climbing up and down one staircase and VAS score dropped significantly in both groups (allP<0.05) and were shorter or lower in the observation group than in the control group (bothP<0.05), (Table 4).
3.3.4 Comparison of MRI grading
There was no significant difference in MRI grading between the two groups before treatment (P>0.05).After treatment, there was no significant change in MRI grading in the control group (P>0.05), while notable improvement was found in the observation group(P<0.05) and the observation group was superior to the control group (P<0.05), (Table 5).
3.3.5 Comparison of the levels of NF-κB, TNF-α and IL-1β in knee joint fluid
Prior to treatment, there were no significant differences in the levels of NF-κB, TNF-α and IL-1β between the two groups (allP>0.05). After treatment,the levels of NF-κB and IL-1β declined significantly in the control group (bothP<0.05); the levels of NF-κB, TNF-α and IL-1β all dropped significantly in the observation group (allP<0.05), and were lower than those in the control group (allP<0.05), (Table 6).
Table 3. Comparison of the WOMAC score (±s, point)
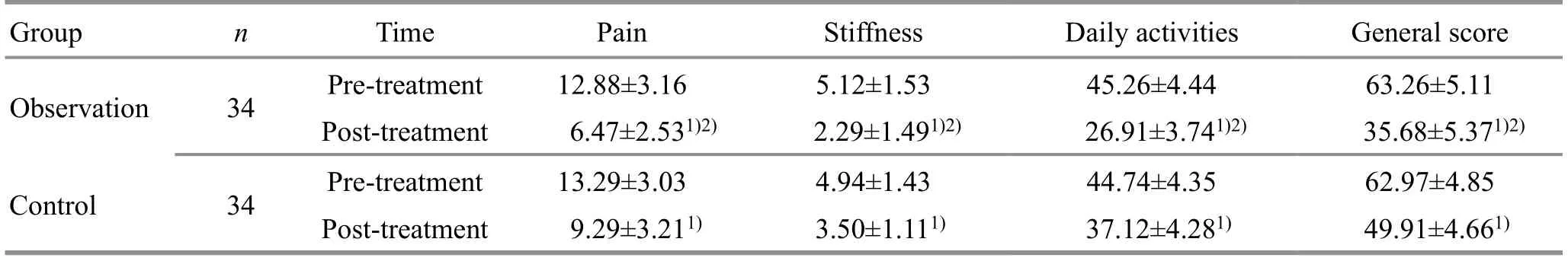
Table 3. Comparison of the WOMAC score (±s, point)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
Group n Time Pain Stiffness Observation 34 Pre-treatment 12.88±3.16 5.12±1.53 Post-treatment 6.47±2.531)2) 2.29±1.491)2) Control 34 Pre-treatment 13.29±3.03 4.94±1.43 Post-treatment 9.29±3.211) 3.50±1.111) Daily activities General score 45.26±4.44 63.26±5.11 26.91±3.741)2) 35.68±5.371)2)44.74±4.35 62.97±4.85 37.12±4.281) 49.91±4.661)
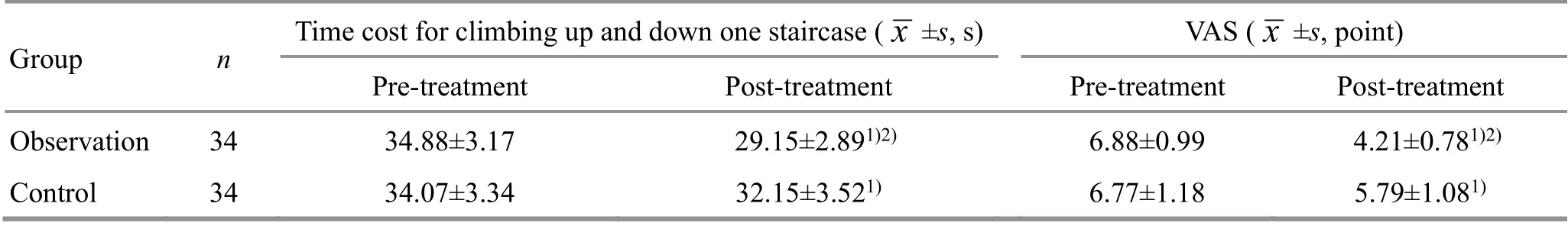
Table 4. Comparison of the time cost for climbing up and down one staircase and VAS score
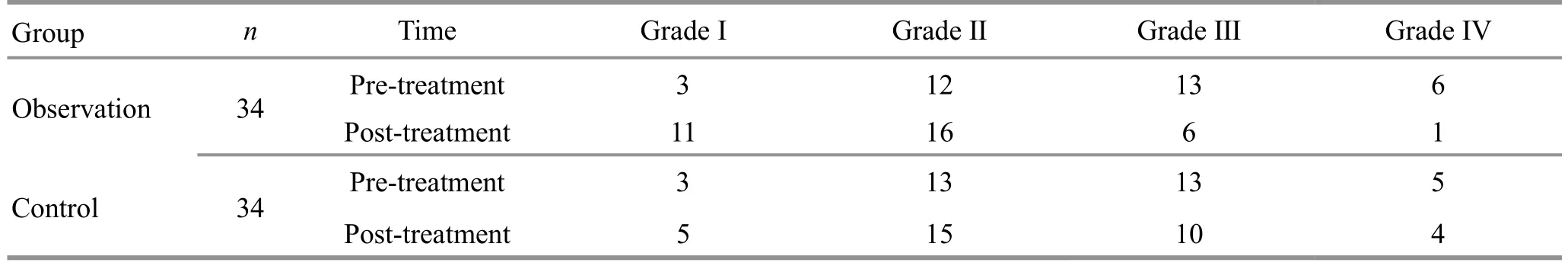
Table 5. Comparison of MRI grading (case)
Table 6. Comparison of the levels of NF-κB, TNF-α and IL-1β in knee joint fluid (±s)
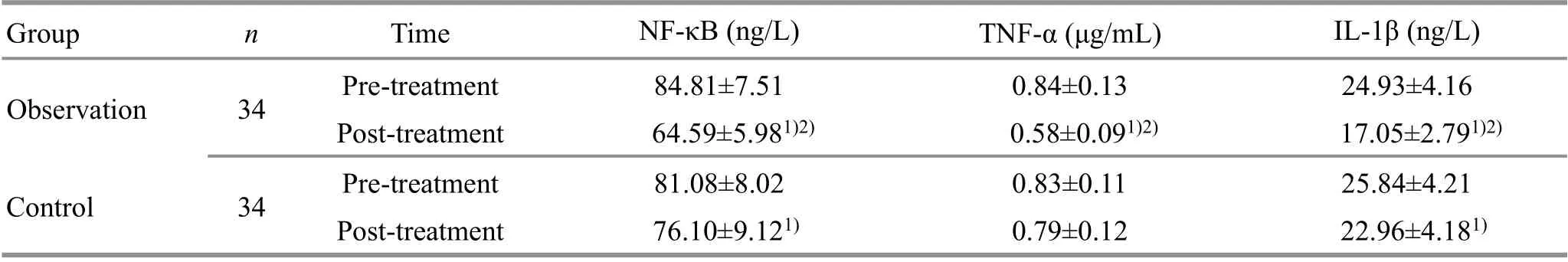
Table 6. Comparison of the levels of NF-κB, TNF-α and IL-1β in knee joint fluid (±s)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
Group n Time NF-κB (ng/L) TNF-α (μg/mL) IL-1β (ng/L)Observation 34 Pre-treatment 84.81±7.51 0.84±0.13 24.93±4.16 Post-treatment 64.59±5.981)2) 0.58±0.091)2) 17.05±2.791)2)Control 34 Pre-treatment 81.08±8.02 0.83±0.11 25.84±4.21 Post-treatment 76.10±9.121) 0.79±0.12 22.96±4.181)
4 Discussion
CP is a common disease in orthopedics, with the degenerative patella cartilage as its main pathological change. The cause of CP is not yet clear, but may be related to trauma, patella instability, increased intraosseous pressure of the patella, cartilage dissolution,autoimmunity, and cartilage dystrophy[12]. Pain is the main symptom of CP, mostly due to secondary synovitis,increased intraosseous pressure, and lowered pain threshold[13]. Intra-articular injection of sodium hyaluronate is one of the most commonly used methods in the treatment of CP. It can directly supplement the synovial mucopolysaccharide substance, improve cartilage damage and prevent further damage to the cartilage matrix. Also, it can inhibit the chemotaxis of leukocytes to limit the spread of inflammation and the production of pain substances. Moreover, it can lubricate the joints and prevent adhesion[14].
There is no proper term for CP in the traditional Chinese medicine classics. According to its clinical symptoms, it can be classified into categories such as ‘Biimpediment’ and ‘tendon injuries’. In a deficient state,the kidney can’t play its role well in governing bones, and the liver can’t nourish tendons. Deficient liver and kidney resulting in malnourishment of tendons and bones should be the pathogenic root in CP. The invasion of wind,cold and dampness is the important external cause of this disease. Deficiency of liver and kidney and insufficient healthy qi, together with the invasion of wind,cold and dampness, result in a fight between the healthy qi and pathogenic evils, leading to blocked meridians and qi-blood coagulation, manifested as achy and numb joints as well as motor dysfunction; qi-blood stagnation and abnormal fluid distribution also contribute to the malnourishment of tendons and bones, leading to Biimpediment over time[15]. It can be seen that the main pathogenic factor should be stagnation of qi and blood.Thus, regulating and activating qi-blood flow should be taken as the main treatment principle.
As a combination of acupuncture and moxibustion,warm needling moxibustion can warm and unblock meridians and promote the circulation of qi and blood. It is suitable for the syndrome of stagnant meridians such as arthralgia. In this study, Xuehai (SP 10), Liangqiu(ST 34), Dubi (ST 35), Neixiyan (EX-LE 4), Sanyinjiao (SP 6)and Taichong (LR 3) were selected to receive warm needling moxibustion. Among these points, Xuehai(SP 10) acts to activate blood flow to resolve stasis and cultivate and supplement blood, so that it is good at treating blood diseases; Liangqiu (ST 34), Dubi (ST 35),Neixiyan (EX-LE 4) and Xuehai (SP 10) were topical acupoints selected to regulate and dredge the qi-blood flow and meridians in the knee joint; Sanyinjiao (SP 6) is the crossing point of Spleen, Liver and Kidney Meridians,working to regulate qi-blood function; Taichong (LR 3),the Yuan-Primary and Shu-Stream point of the Liver Meridian, works to dredge the liver to activate qi circulation and activate blood flow to resolve stasis,producing definite efficacy for knee pain especially because ‘the Shu-Stream points are good at treating the sense of heaviness and joint pain’. These acupoints together can produce a joint effect to regulate and unblock meridians, activate qi-blood flow and resolve stasis, and finally cease the pain.
MRI is the first choice for the diagnosis of CP[16], as it can accurately reflect the disease condition and objectively indicate the extent of the disease. It can be used to track the efficacy after treatment[17]. In this study,patients were examined by MRI before and after treatment to determine the CP grading.
This study also monitored the levels of inflammatory cytokines in knee joint fluid before and after treatment,including NF-κB, TNF-α and IL-1β. These inflammatory cytokines can cause or exacerbate inflammation of the synovial membrane in the knee joint, resulting in inflammatory pain; increased levels of inflammatory factors change the osmotic pressure of the synovial membrane, allowing more plasma enzymes to enter the synovial fluid from the plasma, accelerating cartilage dissolution and inhibiting cartilage repair; abnormal secretion of inflammatory factors in synovial fluid can increase the content of chondroitin sulfate in the cartilage and dissolve the cartilage matrix, leading to a decrease in cartilage elasticity, affecting its elastic deformation function and normal nutrient acquisition,prone to articular cartilage damage, and ultimately resulting in patellar cartilage degeneration[18]. When abnormally activated under the action of stimulating factors such as oxidative stress and cytokines, NF-κB can trigger abnormal inflammation and immune damage,up-regulate the expression of inflammatory mediators and cytokines, and participate in the pathogenesis of osteoarthritis[19]. TNF-α plays an important role in immune response and inflammatory system. It can inhibit the synthesis of cartilage collagen and proteoglycan, promote the release of prostaglandins,and trigger chondrocyte degradation. IL-1β is a crucial cytokine in the destruction of articular cartilage and its level is positively correlated with the degree of cartilage damage[20]. So, inflammatory cytokines such as NF-κB,TNF-α and IL-1β play an important role in the development of CP. Reducing inflammatory cytokines in knee joint fluid is significant in the treatment of CP.
This study showed that the effective rate was higher in the observation group than in the control group (P<0.05);after treatment, the pain, stiffness, daily activities and WOMAC total scores decreased significantly in both groups (allP<0.05), and were lower in the observation group (allP<0.05); the time taken to go up and down a staircase and the VAS score also dropped significantly in the two groups (allP<0.05), and were shorter or lower in the observation group than in the control group (bothP<0.05). The results demonstrate that warm needling moxibustion combined with sodium hyaluronate is effective in the treatment of CP, and this treatment method can significantly relieve the clinical symptoms.After treatment, the MRI grading of the control group was not statistically different from that before treatment(P>0.05), while the MRI grading of the observation group was significantly improved (P<0.05) and was better than that of the control group (P<0.05). It is suggested that warm needling moxibustion plus sodium hyaluronate can improve the patellar cartilage lesions. After treatment, the levels of NF-κB and IL-1β in knee joint fluid in the control group decreased significantly (bothP<0.05), while the levels of NF-κB, TNF-α and IL-1β all decreased significantly in the observation group (allP<0.05) and were lower than those in the control group(allP<0.05). This shows that warm needling moxibustion can notably reduce the levels of NF-κB, TNF-α and IL-1β in knee joint fluid of CP patients, which may be related to the mechanism of warm needling moxibustion plus sodium hyaluronate in the treatment of CP.
In summary, warm needling moxibustion plus intraarticular injection of sodium hyaluronate can produce definite efficacy in the treatment of CP. It can alleviate the clinical symptoms, improve the patellar cartilage lesions, and reduce the levels of NF-κB, TNF-α and IL-1β in knee joint fluid. Therefore, it is worthy of clinical practice and promotion.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
There was no project-fund supporting for this study.
Statement of Informed Consent
Informed consent was obtained from all individual participants.
Received: 30 March 2020/Accepted: 30 July 2020
 Journal of Acupuncture and Tuina Science2021年3期
Journal of Acupuncture and Tuina Science2021年3期
- Journal of Acupuncture and Tuina Science的其它文章
- Efficacy of acupuncture in treating chronic non-specific low back pain
- Therapeutic efficacy observation of acupuncture plus medicine for laryngopharyngeal reflux due to liver-qi stagnation and spleen deficiency
- Clinical efficacy observation on pediatric massage for chronic cough in children
- Effects of acupuncture plus spinal manipulations on physical functioning and biochemical indicators in patients with ankylosing spondylitis
- Effect of mild moxibustion on cancer-related fatigue,serum ghrelin and adiponectin in patients undergoing chemotherapy after colorectal cancer surgery
- Clinical efficacy observation of acupoint threadembedding in treating obese patients with food addiction
