Donor defects after lymph vessel transplantation and free vascularized lymph node transfer: A comparison and evaluation of complications
Gunther Felmerer, Dominik Behringer, Nadine Emmerich, Marian Grade, Adam Stepniewski
Gunther Felmerer, Dominik Behringer, Adam Stepniewski, Division of Plastic Surgery, Department for Trauma Surgery, Orthopedics and Plastic Surgery, University Medical Center Goettingen, Goettingen 37075, Lower Saxony, Germany
Nadine Emmerich, Georg-August University Goettingen, University Medical Center Goettingen, Goettingen 37075, Lower Saxony, Germany
Marian Grade, Department of General, Visceral and Pediatric Surgery, University Medical Center Goettingen, Goettingen 37075, Lower Saxony, Germany
Abstract BACKGROUND Secondary lymphedema after surgical interventions is a progressive, chronic disease that is still not completely curable.Over the past years, a multitude of surgical therapy options have been described.AIM To summarize the single-center complications in lymph vessel (LVTx) and free vascularized lymph node transfer (VLNT).METHODS In total, the patient collective consisted of 87 patients who were undergoing treatment for secondary leg lymphedema during the study period from March 2010 to April 2020.The data collection was performed preoperatively during consultations, as well as three weeks, six months and twelve months after surgical treatment.In the event of complications, more detailed follow-up checks were carried out.In total n = 18 robot-assisted omental lymph node transplantations, n = 33 supraclavicular lymph node transplantations and n = 36 Lymph vessel transplantations were analyzed.An exemplary drawing is shown in Figure 1.A graphical representation of patient selection is shown in Figure 2.Robotic harvest was performed with the Da Vinci Xi Robot Systems (Intuitive Surgical, CA, United States).RESULTS In total, 11 male and 76 female patients were operated on.The mean age of the patients at study entry was: omental VLNT: 57.45 ± 8.02 years; supraclavicular VLNT: 49.76 ± 4.16 years and LVTx: 49.75 ± 4.95 years.The average observation time postoperative was: omental VLNT: 18 ± 3.48 mo; supraclavicular VLNT: 14.15 ± 4.9 and LVTx: 14.84 ± 4.46 mo.In our omental VLNT, three patients showed a slight abdominal sensation of tension within the first 12 postoperative days.No other donor side morbidities occurred.No intraoperative conversion to open technique was needed.Our supraclavicular VLNT collective showed 10 lift defect morbidities with one necessary surgical intervention.In our LVTx collective, 12 cases of donor side morbidity were registered.In one case, surgical intervention was necessary.CONCLUSION Concerning donor side morbidity, robot-assisted omental VLNT is clearly superior to supraclavicular lymph node transplantation and LVTx.
Key Words: Lymph surgery; Vascularized lymph node transfer; Lymph vessel transfer; Robot-assisted surgery; Da Vinci Xi; Donor side morbidity
INTRODUCTION
Secondary lymphedema after surgery is a progressive, chronic disease that is still not completely curable.In the literature, a multitude of surgical therapy options have been described over the past years[1-5].
In this thesis, we will discuss a study being undertaken since November 2017 in our clinic according to the established method of robot-assisted lymph node transplantation from the omentum[6].
The autologous supraclavicular lymph node transplantation[7]and the lymph vessel transplantation according to Baumeister[8]will be used as comparative material.
The latter two therapy options have been used internationally since the establishment of microsurgery and for a long time in the main field of plastic surgery at the University Medical Center in Goettingen and have already shown promising results[9-11].The former surgical method, in the form it has been performed in our clinic, represents a novelty and combines the advantages of a minimally invasive intervention using the Da Vinci surgical robot with the already known advantages of lymph node transplantation.Exemplary drawing of the individual donor sides is shown in Figure 1.
Since this is a procedure which requires the opening of the abdominal cavity, any abdominal complications should be worked out in this study.These should be compared with the lifting defect morbidity of the other two procedures.The data collection of the omental patient population was carried out preoperatively at the time of presentation in the consulting room, perioperatively as well as three weeks, six months and twelve months after surgery.
The aim of this study is to examine the complications of robot-assisted lymph node transfer in the treatment of secondary limb lymphedema in comparison to already known procedures in our clinic.
MATERIALS AND METHODS
In this study, data from three different collectives were collected and evaluated.A total of 87 patients undergoing treatment at our clinic between March 2010 and April 2020 were included.The evaluation included data was collected at each appearance during consultation hours, during surgical treatment and during stationary care.
Inclusion criteria for all collectives were, in the case of tumor suffering, a permanent remission and the absence of infections and inflammations.In addition, an adequate conservative therapy over a period of at least half a year should have been carried out beforehand.Some patients were advised to undergo inpatient rehabilitation with Complex Physical Decongestion before surgery.
The procedure for selecting the surgical procedure is shown in Figure 2.
Omental lymph node transplantation robot-assisted
A total of 18 patients could be included in the study section (one man, 17 women).The mean age of the patients at study entry was 57.45 ± 8.02 years (range: 40-75 years), the mean observation period was 18 ± 3.48 mo (range: 12-27 mo).
The main focus of the anamnestic interview was on the causes, the triggers, the latency period, the already performed conservative therapy and the question of erysipelas or other complications.Postoperatively, the anamnestic questioning of gastrointestinal symptoms was essential.Necessary inclusion criterion for the intervention was the removal of the corresponding lymph nodes in the inguinal or axillary region during the initial intervention.Patients with removed pelvic, paraaortic and only sentinel lymph node removal were not included.Lymph vessel transplantation or lymphovenous anastomosis were offered to these patients if surgery was desired and indication was given.
Postoperatively, the patients were called in for consultation at regular intervals to monitor their progress.
An essential prerequisite for performing an autologous lymph node transplant at our clinic is the removal of the inguinal or axillary lymph nodes.Here it is important that the removal of a single lymph node, for example a sentinel lymph node, or a lymph node biopsy does not provide sufficient indication.A transplantation into a non-functional region, such as an elbow or ankle, is not performed at our clinic.Consequently, only transplantations into the axilla or groin are performed.
The robot-assisted abdominal part of the operation is carried out in cooperation with colleagues from the general and visceral surgery department of the hospital.The da Vinci Xi robot system (Intuitive Surgical, CA, United States) is used for omental flap harvest.
Cervical lymph node transplantation
A total of 33 patients could be included in this study section (two men, 31 women).The mean age of the patients at study entry was 49.76 ± 4.16 years (range: 22-77 years), the mean observation period was 14.15 ± 4.9 mo (range: 4-66 mo).
The main focus of the anamnestic interview was on the causes, the triggers, the latency period, the conservative therapy already carried out and the question of erysipelas and other pre- and postoperative complications.As already described, necessary inclusion criterion for the intervention was the removal of the corresponding lymph nodes in the inguinal or axillary region during the initial intervention.Postoperatively, the patients were called in for consultation with the plastic surgery department at regular intervals to monitor their progress.
Lymph vessel transplantation
A total of 36 patients could be included in this study section (eight men, 28 women).The mean age of the patients at study entry was 49.75 ± 4.95 years (range: 15.9-60.7 years), the mean observation period was 14.84 ± 4.46 mo (range: 4-57 mo).
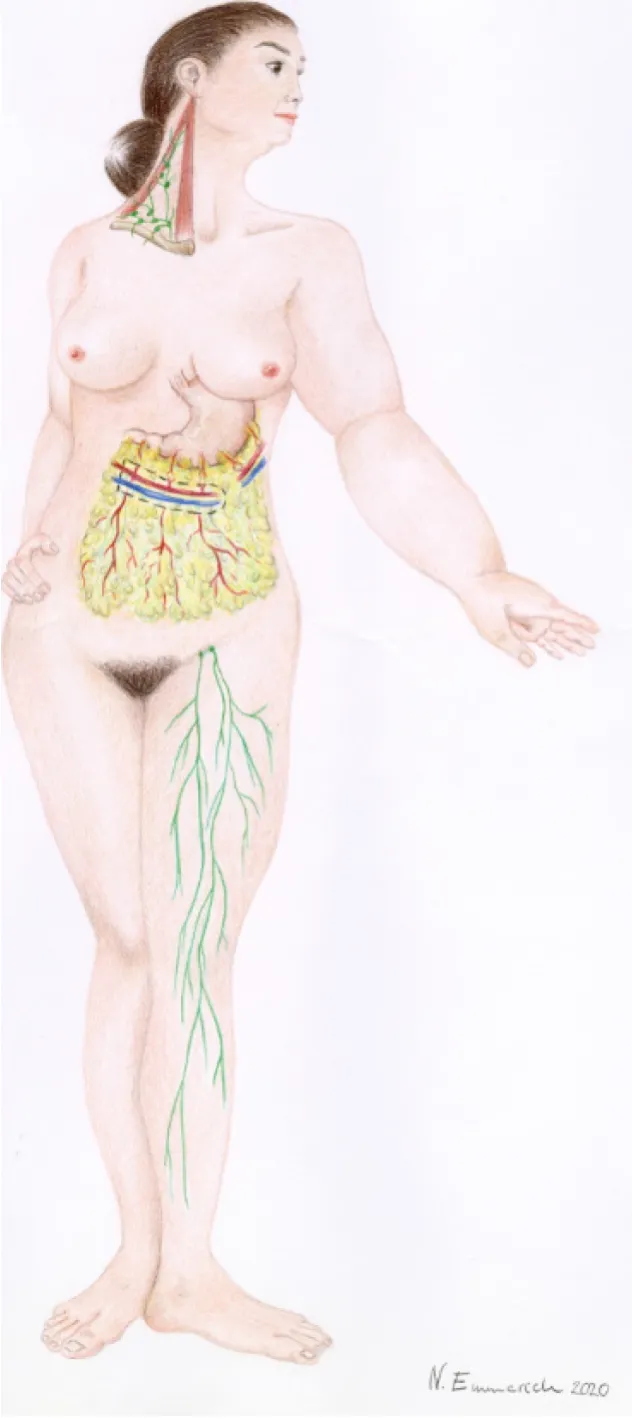
Figure 1 Exemplary drawing of the individual donor sides.
The main focus of the anamnestic interview was, as in the other groups, the causes, the triggers, the latency period and the conservative therapy already carried out and the question of erysipelas or other complications.Necessary inclusion criteria for the procedure was a lack of swelling in the area of the donor region.If the patients reported a corresponding swelling tendency after primary surgery, no lymph vessel transplantation was performed, even if there was no lymphedema in the area of the donor leg when the patient was seen during consultation.If, on the day of the operation, after intraoperative injection of patent blue, a dermal backflow was observed in the area of the donor leg, no lymph vessel transplantation was performed either.In such cases, lymphovenous anastomoses were applied.The patients were informed about this procedure preoperatively.In our lymph vessel group from 2010 to 2018, this occurred once.
Postoperatively, patients were seen during consultation hours of the plastic surgery department at regular intervals for follow-up.
RESULTS
Omental lymph node transplantation robot-assisted

Figure 2 Flowchart showing the selection of the surgical procedure.
A total ofn= 18 patients could be included in the robot-assisted vascularized lymph node transfer (VLNT) study (one man, 17 women).The mean age of the patients at study entry was 57.45 ± 8.02 years (range: 40-75 years), the mean observation period was 18 ± 3.48 mo (range: 12-27 mo).In eight cases the right, in ten cases the left extremity was affected.According to the International Society of Lymphology (ISL) classification, 15 patients were classified as stage II, three patients as stage III.A total of eight leg lymphedema and ten arm lymphedema were operated on.Breast cancer was the most frequent primary diagnosis withn= 10 patients.The second most frequent cause was cervical carcinoma and vulva carcinoma with a frequency ofn= 2 each.With a frequency ofn= 1 each, surgical treatment was performed for a liposarcoma of the thigh, squamous cell carcinoma of the penis, malignant melanoma and a malignant peripheral neuroectodermal tumor.Six patients had received radiochemotherapy after primary surgery.Three patients received pure radiotherapy.Two patients received chemotherapy.All patients underwent lymphonodectomy in primary surgery.The average time from diagnosis to surgery was 91.64 ± 48.98 mo (range: 6-204 mo).Three of the surgical patients reported recurrent erysipelas of the corresponding lymphedematous extremity preoperatively.Two of them had three episodes per year and one patient had an average of four episodes.None of these patients suffered from recurrent erysipelas of the corresponding limb during the postoperative observation period.Three patients reported a slight tension in the abdominal area in the early postoperative phase with rapidly decreasing symptoms in the first 12 d (Table 1).A total of 5/18 patients had already undergone abdominal surgery.Among the procedures performed were two laparoscopic hysterectomies, one laparoscopic ovariectomy, one exploratory laparoscopy, one laparoscopic cholecystectomy and one robot-assisted pelvic lymphonodectomy.None of the surgical patients required an intraoperative change to an open procedure with medial laparotomy.
Cervical lymph node transplantation
A total of 33 patients could be included in the cervical lymph node group (two men, 31 women).The mean age of the patients at study entry was 49.76 ± 4.16 years (range: 22-77 years), the mean observation period was 14.15 ± 4.9 mo (range: 4-66 mo).In 17 cases the left, in 16 cases the right extremity was affected.According to the ISL classification, two patients were classified as stage III, the remaining 31 as stage II.In total, 13 Leg and 20 arm lymphedema were performed.Breast cancer was the most frequent primary diagnosis in the cervical lymph node group withn= 20 patients.The second most frequent cause was vulvar carcinoma and malignant melanoma withn= 3 cases each.n= 2 patients each underwent primary surgery for cervical carcinoma and liposarcoma.Withn= 1 each, a lipoma of the thigh, endometrial carcinoma and lymphedema after inguinal hernia and removal of the inguinal lymph nodes were performed.
Seventeen patients had received radiochemotherapy after primary surgery.Three patients received pure radiotherapy.Two patients received pure chemotherapy.The average time from diagnosis to surgery was 72.87 ± 17.36 mo (range: 6-216 mo).Three patients reported recurrent erysipelas preoperatively.In two of the three patients, no recurrent erysipelas occurred in the follow-up period of one year.
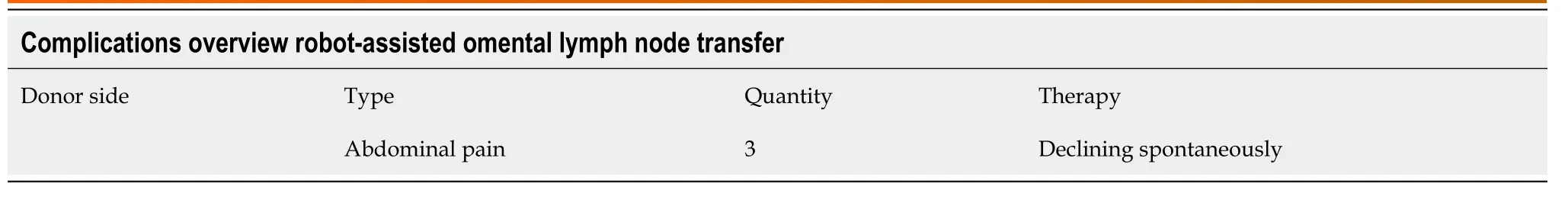
Table 1 Donor side morbidity after robot-assisted omental vascularized lymph node transfer
Only supraclavicular lymph nodes were used as donor nodes in our clinic.A total of 24 right and nine left cervical lymph node packages were removed and used for transplantation.
A total of 10 complications occurred in 33 surgical patients during the inpatient and post-operative treatment.A tabular list of the individual complications as well as their number and therapy is given in Table 2.
In terms of donor side morbidities, three seromas worthy of puncture occurred poststationarily.On one occasion, a wound infection was found, which decreased well under antibiotic therapy.One lymphocele was found, which was punctured in an outpatient treatment.A persistent lymph fistula in the left cervical region had to be surgically revised and closed.In the case of significant cervical soft tissue swelling, one patient developed a temporary Horner's syndrome, which, however, regressed in the inpatient course.In the first follow-up, three weeks after surgery, no symptoms remained.One patient complained postoperatively about a hypertrophic, painful scar in the neck region.With two triamine infiltrations, a significant improvement of the symptoms could be achieved.Another patient complained postoperatively of hyposensitivity in the clavicular region.
Lymph vessel transplantation
A total of 36 patients could be included in the study (eight men, 28 women).The mean age of the patients at study entry was 49.75 ± 4.95 years (range: 15.9-60.7 years), the mean observation period was 14.84 ± 4.46 mo (range: 4-57 mo).In 18 cases, the left extremity was affected, in 15 cases the right extremity.Three patients were affected on both sides.According to the ISL classification five patients were classified as stage III, the remaining 31 as stage II.A total of 22 Legs, 11 arms, two lymphedema in the facial area and one lymphedema in the genital area were operated on.Cervical carcinoma was the most frequent primary diagnosis in the lymph vessel group withn= 13 patients.The second most frequent cause was breast carcinoma withn= 11 cases followed by malignant melanoma withn= 2 affected patients.This was followed by endometrial carcinoma, ovarian carcinoma, squamous cell carcinoma of the lower mouth, prostate carcinoma, leiomyosarcinoma, seminoma, renal cell carcinoma, non-Hodgkin's lymphoma, postinfectious lymphedema and lymphedema after massive acne vulgaris withn= 1 each.
Nineteen patients had received radiochemotherapy after primary surgery.Three patients received pure radiotherapy.One patient received chemotherapy.
The average time from diagnosis to surgery was 51.45 ± 13.05 mo (range: 12-137 mo).
Two patients reported recurrent erysipelas preoperatively.In one of the two patients, no recurrent erysipelas occurred in the follow-up period of one year.
As total of 5 different donor side morbidities occurred.One lymphocele occurred, which closed after five punctures.Two wound dehiscences with wound healing disturbances were seen.Two wound infections occurred, which were treated conservatively with antibiotics.Two lymph fistulas occurred, which stopped spontaneously after increasing albumin levels.In five of the 36 patients, there was an increase in the circumference of the donor leg.All five patients were fitted with appropriate compression stockings.One patient was equipped with compression stockings on the foot with a circular knit.Three patients required knee stockings with a circular knit.The last patient required a complete thigh stocking of compression class I with a flat knit (Table 3).
DISCUSSION
Since the establishment of laparoscopic minimally invasive surgery in everyday clinical practice and, most recently, further development using robot-assisted procedures, there have been significant changes in reconstructive lymph surgery.The robot-assisted lymph node transfer from the omentum was first described in 2016[12].Previously, the same author had performed omental lymph node transplants in a laparoscopic manner with good results in ten patients[13].Particular advantages of the robotic procedure were shown, among others, due to the three-dimensional image quality and the robot-supported preparation, which eliminates the physiological tremor and thus enables very precise and vessel-sparing preparation[12].Due to the fact that abdominal lymph nodes are used for transplantation and the peritoneum is opened, a variety of potential complications arise with these procedures[14-18].
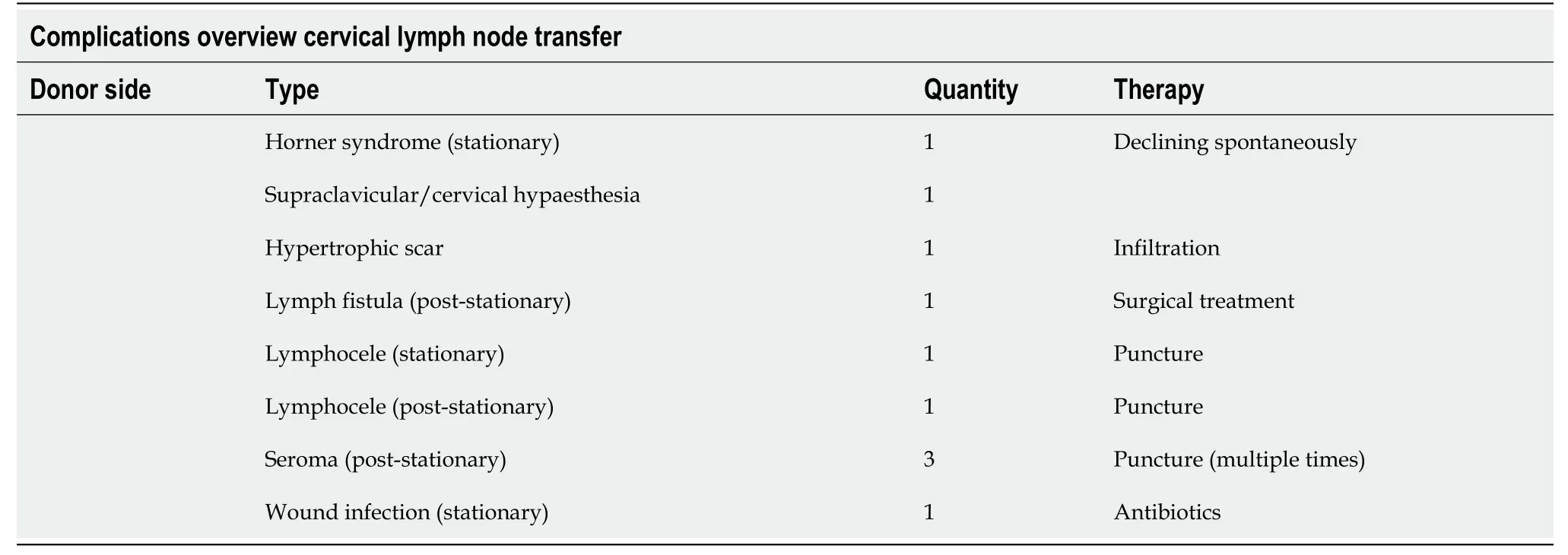
Table 2 Donor side morbidity after cervical vascularized lymph node transfer

Table 3 Donor side morbidity after lymph vessel transplantation
At present, only a few publications on robot-assisted VLNT have been published[12,19].To the best of our knowledge, our study withn= 18 is the largest robotassisted VLNT study published to date.In our patient group, 3/18 patients reported pulling pain in the abdominal and thoracic region within the first days after surgery.In our opinion, this is most likely due to the temporarily created pneumoperitoneum.The complaints had subsided after 12 d.Further complications have not occurred in our patient group so far.With regard to long-term complications such as trocar hernias and adhesions, no reliable assessment can be yet made.
Similar to other authors, we experienced some donor side morbidities after supraclavicular VLNT[20,21].
The unique reversible occurrence of Horner's syndrome in our group of patients illustrates the complex anatomy of the supraclavicular region, which has already been discussed before.In case of spontaneous regeneration, as in our event, it is assumed that the corresponding nerve was overstretched by retractors or inserted hooks during the operation[22].
Although several studies have already shown the general practicability of lymph vessel transplantation, there is little literature available on elevation defect morbidities.In addition to general complications such as wound infections, wound healing disorders and lymph fistula, five iatrogenic lymphedema occurred in the donor leg area.It should be noted that the listing in our study took place when compression garments were prescribed or recommended only once.We highly believe that the actual number of patients requiring compression garments will be much lower in the long run.
CONCLUSION
In summary, robot-assisted omental VLNT is clearly superior to supraclavicular VLNT and LVTx due to the reliably low donor side morbidity.The evaluation of long-term consequences will have to be clarified in future studies.
ARTICLE HIGHLIGHTS
Research background
Secondary lymphedema after surgery is a progressive, chronic disease that is still not completely curable.Over time a multitude of surgical therapy options have been described with its individual complications and side effects.
Research motivation
Due to technical progress in robot-assisted surgery, many advances have been made in this field within the last few years.This has significantly increased the precision and tissue-sparing work during abdominal interventions and made omental flap harvest much easier.Our motivation was to compare the complications of robot-assisted lymph node transfer in the treatment of secondary limb lymphedema.
Research objectives
Since 2010 we use the autologous supraclavicular lymph node transplantation (VLNT)and the lymph vessel transplantation (LVTx) according to Baumeister.Since 2017 we perform robot assisted free VLNT from the omentum.Our motivation was to summarize and point out the single-center complications in LVTx and free VLNT.
Research methods
In this study, data from three different collectives were collected and evaluated.A total of 87 patients undergoing treatment at our clinic were included.In total n = 18 robot-assisted omental lymph node transplantations, n = 33 supraclavicular lymph node transplantations and n = 36 Lymph vessel transplantations were analyzed.The data collection was performed preoperatively during consultations, as well as three weeks, six months and twelve months after surgical treatment.Descriptive statistics were used to analyze the patient data.
Research results
In the omental VLNT, three patients showed a slight abdominal sensation of tension within the first 12 postoperative days.No other donor side morbidities occurred.Our supraclavicular VLNT collective showed 10 lift defect morbidities with one necessary surgical intervention.In our LVTx collective, 12 cases of donor side morbidity were registered.In one case , surgical intervention was necessary.
Research conclusions
Concerning donor side morbidity, robot-assisted omental VLNT is clearly superior to supraclavicular lymph node transplantation and LVTx.
Research perspectives
At present, only a few publications on robot-assisted VLNT have been published.Because of the short time, no reliable assessment concerning long-term complications can be yet made.The evaluation will have to be clarified in future studies.
ACKNOWLEDGEMENTS
The authors would like to thank Mr.Timothy Campbell, MA, PgMP, PMP for correction of language, grammar and punctuation.
 World Journal of Transplantation2021年4期
World Journal of Transplantation2021年4期
- World Journal of Transplantation的其它文章
- Does steroid-free immunosuppression improve the outcome in kidney transplant recipients compared to conventional protocols?
- Perioperative risk factors associated with delayed graft function following deceased donor kidney transplantation: A retrospective,single center study
