Assessment of left-ventricular diastolic function in pediatric intensive-care patients:a review of parameters and indications compared with those for adults
Morgan Recher·Astrid Botte·Jerome Soquet·Jean-Benoit Baudelet·François Godart·Stephane Leteurtre
Abstract Background The incidence of diastolic heart failure has increased over time.The evaluation of left-ventricular diastolic function is complex,ongoing,and remains poorly performed in pediatric intensive-care patients.This study aimed to review the literature and to provide an update on the evaluation of left-ventricular diastolic function in adults and children in intensive care.Data sources We searched data from PubMed/Medline.Thirty-two studies were included.Four pragmatic questions were identified:(1) What is the physiopathology of diastolic dysfunction? (2) Which tools are required to evaluate diastolic function? (3) What are the echocardiographic criteria needed to evaluate diastolic function? (4) When should diastolic function be evaluated in pediatric intensive care?Results Early diastole allows characterization of relaxation,whereas compliance assessments and filling pressures are evaluated during late diastole.The evolution of diastolic function differs between adults and children.Unlike in adults,decreased compliance occurs at the same time as delayed relaxation in children.Diastolic function can be evaluated by Doppler echocardiography.The echocardiographic criteria for ventricular relaxation include the E wave,E/A wave ratio,and isovolumic relaxation time.Ventricular compliance can be assessed by the E/ e’ wave ratio,atrial volume,and Ap wave duration during pulmonary vein flow.In adult intensive-care patients,the E/ e’ ratio can be used as an index of tolerance for volume expansion in septic patients and to adjust the inotropic support.Conclusion Clinical studies would allow some of these parameters to be validated for use in children in intensive care.
Keywords Diastole·Echocardiography·Heart failure·Intensive-care unit·Pediatric
Introduction
Left ventricle (LV) systolic dysfunction is usually accompanied by a variable degree of diastolic dysfunction.Conversely,diastolic dysfunction may exist in conjunction with normal LV systolic function indexes;this is referred to as heart failure with preserved ejection fraction (HFpEF) [1].The diastolic characteristics of the LV have been clearly shown to be involved in cardiac performance [2,3].The incidence of diastolic dysfunction has increased over time(from 38 to 47% within 15 years) [4].Over 15 years,numerous epidemiological,physiopathological,clinical,and prognostic studies have been conducted to understand diastolic heart failure [5,6].However,most studies were performed in adults,with only a few studies focused on the pediatric population [7].
Diastolic function (DF) is a complex process and its evaluation needs to be characterized using multiple parameters.An evaluation of LV DF in adult intensive-care patients has been recently described [8].In children,assessing DF using echocardiography is complex,because most parameters are particularly affected by the patient’s age,heart rate,and type of congenital heart disease.For children in pediatric intensive-care units,the characterization of DF remains challenging [9].However,diastolic dysfunction occurs in several conditions observed in intensive-care patients,and its assessment may provide important information to physicians during the decision-making process.The primary objective of this study was to provide an update on the physiology and evaluation of LV DF in adults and children in intensive-care units.The second objective was to evaluate the usefulness and pragmatism of parameters used to assess DF in pediatric intensive-care patients.
Studies with the following criteria were selected:(1)retrospective and prospective studies,(2) human studies conducted in children and adults hospitalized in intensive care,and (3) studies including measures of LV DF.Newborn infants were excluded from this research.The literature review was completed in December 2018.Relevant electronic databases,including MEDLINE and PubMed,were searched for studies published in either English or French,between 1980 and 2018;the following algorithm was used:“diastolic function”AND (“intensive care”OR ICU OR“pediatric intensive care”OR PICU).Two authors independently screened each article for inclusion.There were no eligibility restrictions based on the study design,country of origin,or single versus multi-institutional admissions.Articles were excluded when only the abstract was available.
Authors screened titles and abstracts for content relevant to diastolic function evaluation using echocardiography in pediatric and adult intensive-care patients as inclusion criteria.A sample size restriction was not applied when screening eligible studies.
A total of 38 studies met the inclusion criteria (Supplementary Fig.1).The publication analysis led to the development of four main questions:(1) What is the physiopathology of diastolic dysfunction? (2) Which tools are required to evaluate DF? (3) What are the echocardiographic criteria needed to evaluate DF? (4) When should DF be evaluated in pediatric intensive-care patients?
What is the physiopathology of diastolic dysfunction?
In adults,diastolic heart failure represents one-third of heart failure cases,and these cases have higher rates of progression than cases of heart failure of systolic origin [10].The prognosis of patients with diastolic heart failure is poor(5-year survival,35 ± 3%) compared with that of patients with altered LV systolic function [11].Diastolic dysfunction is defined by the inability of the ventricle to fill,with normal atrial pressure,during exertion and at rest.It is secondary to the extension of the relaxation phase and decrease in ventricle compliance [12].Several associated conditions are required to meet the diagnostic criteria for HFpEF (Table 1)[13].
DF depends on two overlapping parameters that characterize the intrinsic functions of the LV,namely the post-systolic relaxation and compliance;it can also be influenced by extrinsic factors [12].The systolic and diastolic functions of the LV can be illustrated using pressure—volume curves,as reported by Appleton et al.[14].The changes can be quantified using the slope of the tangent of the pressure—volume curve during diastole (dP/dV) after cardiac catheterization.In patients with diastolic dysfunction,the atrial pressure increases to maintain the gradient of transmitral pressure that allows LV filling.
Traditionally,in adults,relaxation parameters are used to characterize early diastole,whereas the compliance and filling pressure parameters are used to characterize late diastole.A paradigm has been established in adults in which diastolic dysfunction progresses from normal to impaired relaxation,with an intermediate phase of pseudo-normalcy that is characterized by increasing filling pressures.At a late stage,the restricted filling phase appears,with poor ventricular compliance [15].In neonates,the LV remains poorly differentiated,with little compliance,but evolves rapidly during the first year of life to reach specific compliance and contractility characteristics.This lack of compliance induces a shorter filling time and requires a larger duration of atrial systole during ventricular diastole.Masutani et al.demonstrated that children with HFpEF showed decreased relaxation and increased myocardial stiffness [7].Furthermore,Kawaguchi et al.showed that patients with the same characteristics had ventricular and arterial stiffness that contributed to diastolic dysfunction [16].The stretching of ventricular myocardial fibers and the ventricular transmural pressure are triggers for the production of natriuretic peptides [17].Unlike in adults,decreased compliance may occur simultaneously with delayed relaxation in children [18].
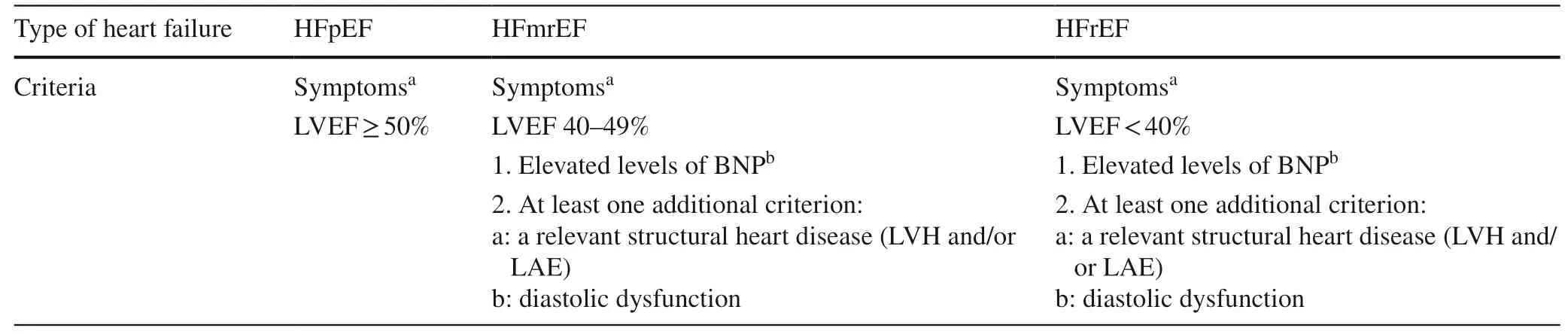
Table 1 Definition of heart failure with preserved (HFpEF),mid-range (HFmrEF),and reduced ejection fraction (HFrEF)
Which tools are required to evaluate diastolic function?
Cardiac catheterization
The standard method used to diagnose diastolic dysfunction is left cardiac catheterization [19].This technique measures the time constant,tau (τ),that represents the LV relaxation delay.When the log of the diastolic pressure is plotted as a time function,τis equal to the inverse of the slope of this linear relationship.LV diastolic dysfunction,on the other hand,is indicated by aτ> 48 ms,a left-ventricular end-diastolic pressure (LVEDP) > 16 mmHg,or an average pulmonary capillary pressure > 12 mmHg.Thus,τis considered to be the best index for evaluating relaxation [20].However,performing a cardiac catheterization in intensivecare patients remains problematic in a daily clinical practice,due to organ failure and hemodynamic instability,as well as transfer issues to the catheterization laboratory.In addition,cardiologists may be unavailable to perform the procedure emergently,and a rapid assessment of diastolic function at the patient’s bedside would allow for the best adjustment of therapeutics.
Doppler echocardiography
Doppler echocardiography is the standard clinical technique used to analyze DF due to its accessibility and excellent temporal resolution [21].The echographic diagnostic approach in the intensive care includes four stages,as reported by Vignon [12].First,attribute respiratory failure to increased pulmonary venous pressure (cardiogenic pulmonary edema) while eliminating chronic pulmonary heart disease.Second,ensure a normal or slightly altered systolic function (left-ventricular ejection fraction(LVEF) ≥ 50%).To assess a normal systolic function,the absence of LV dilation (indexed LV volume < 49 mL/m 2)is required in a normovolemic patient [13,22].Third,eliminate the causes of heart failure with preserved LVEF(valvular,pericardial,or right heart conditions,such as pulmonary hypertension or post-embolic disease) or heart failure with a high flow (cirrhosis,chronic anemia,etc.).Finally,find evidence of LV diastolic dysfunction with increased LV filling pressure.
The evaluation of DF combines several parameters.The diagnosis relies on the overall impression,specific context,and responses to cautious treatment.These parameters,combined with tissue Doppler,Doppler of the pulmonary veins,or the propagation speed of the mitral flow,provide information regarding the filling pressures.TheAmerican Society of Echocardiography Council on Pediatric and Congenital Heart Diseaserecommends expressing cardiovascular structure measurements based on a Z-score,using the Haycock formula for body surface area [23,24].A team at the Boston Children’s Hospital created a“Hospital Z-score system”that is based on data collected from normal children over a 12-year period.The parameters are adjusted according to height,weight,and body mass index,and are regularly updated (https://zscor e.chbos ton.org/) [25].Another website,which is also regularly updated,allows for the interpretation of pediatric results using parameters other than the Doppler Tissue Index (DTI) ( https://www.param eterz.com) [26].However,echocardiographic parameters in children have a wide range of normal values,and extracardiac factors (age,heart rate,respiratory rate,etc.) affect these values [27].
Which echocardiographic criteria are needed to evaluate diastolic function?
A multiparametric approach that includes the mitral flow,flow through the pulmonary veins,tissue Doppler echocardiography,and M-mode color Doppler propagation of mitral flow (Vp) is necessary to evaluate DF (Fig.1).Ventricular relaxation is reflected by theEwave,Awave,E/Awave ratio (Fig.2),and the isovolumic relaxation time(IVRT) (Fig.3).Compliance is assessed using theE/e’wave ratio (Fig.4),atrial volume,and the pulmonary vein flow Ap wave duration (Fig.1).However,other parameters,like the deceleration time and IVRT,are influenced by both relaxation and compliance [15].In children,the severity of diastolic dysfunction is less well diagnosed using these parameters [18].
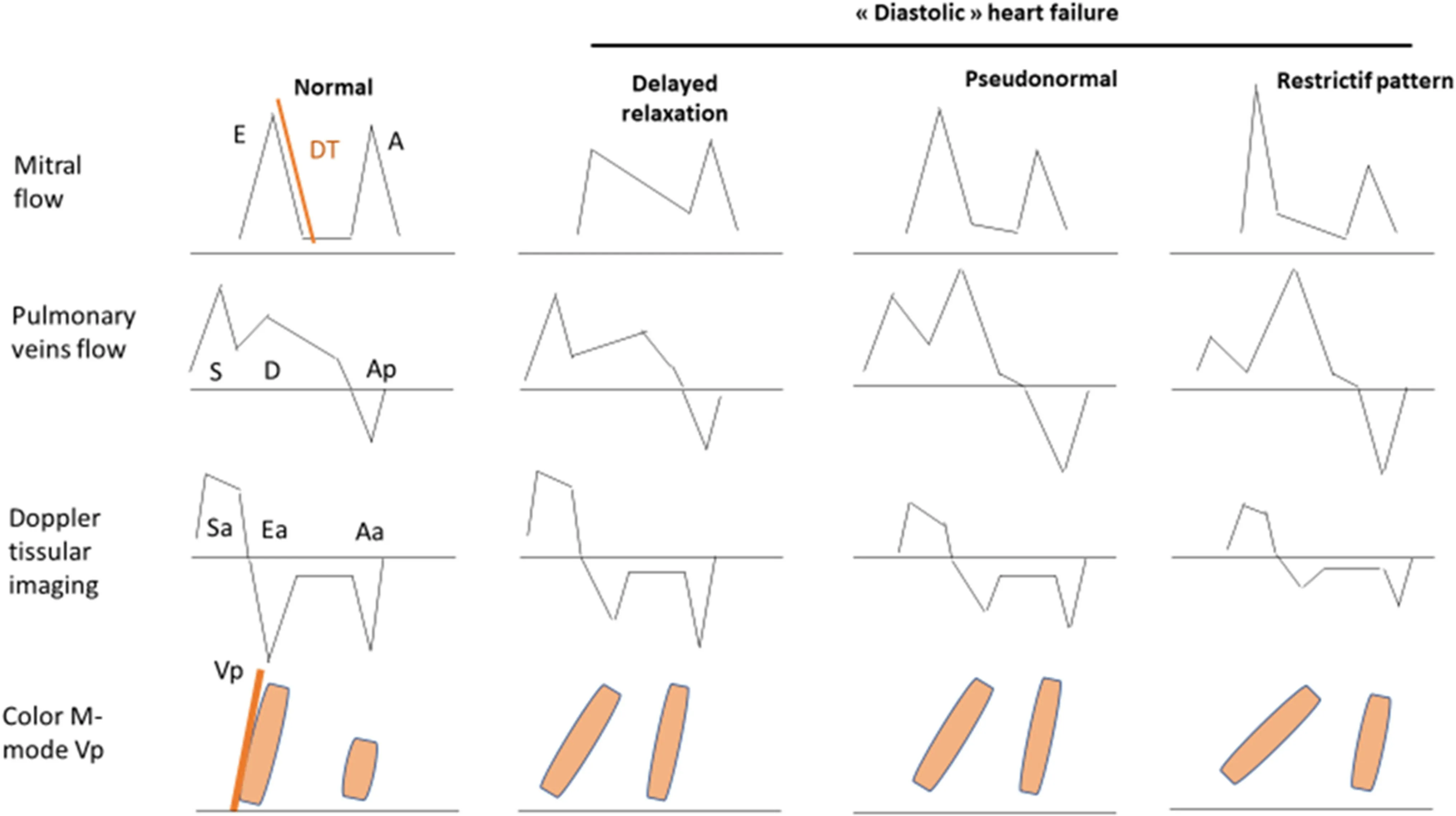
Fig.1 Evaluation of left-ventricular diastolic function using echocardiography
Study of the mitral profile with pulsed Doppler in spectral mode
The study of the mitral profile measures the speeds at which red blood cells move through the vulvar orifice,by an apical four-chamber view.This requires measurement of the following parameters:
The isovolumic relaxation time (IVRT),calculated by the noise of the aortic valve closure and the mitral valve opening.It is measured by pulsed or continuous Doppler or by tissue Doppler as a four-cavity apical section (normal:90 ± 20 ms).
The E-wave peak velocity(E for“early”),which corresponds with fast filling of the LV starting when the pressure of the LV becomes less than that of the LA.
The E-wave deceleration time (DTE),which is between 160 and 240 ms,but can be less in young subjects.It reflects the change in the pressure gradient between LV and LA during fast filling.
The A-wave peak velocityThe auricular contraction produces a second acceleration of the flow entering in the LV.Their ratio,which is normally between 1 and 2,is used.It decreases with age,reaching 1 in one’s sixties.In subjects who are young and active and/or a tachycardia > 100/min,the mitral flux has a pseudo-restrictive profile (E/A> 2) due to very fast relaxation.There is sometimes a fusion of theEandAwaves (tachycardia for example).An anomaly of the relaxation of the LV (decreased relaxation speed) is reflected as a decrease in the amplitude of theEwave.However,the DTE and the otherEandAdiastolic indices are limited by their dependence on load conditions [23].
The mitral flow propagation velocity (Vp)Pulsed Doppler in color mode coupled with time-movement mode allows measurement of the propagation velocity (Vp) of the blood flow that arrives in the LV.This hard-to-measure parameter is less reproducible [23].Care must be taken with its interpretation as it depends on the systolic function.The Vp is normal,before 50 years of age,if > 55 cm/s;after 50 years of age,if > 45 cm/s.A slowing of the Vp of the flow of protodiastolic filling (< 45 cm/s) is indicative of an impairment of relaxation [10,23].
The measurements of the previous parameters (IRTV,E-wave peak velocity,A-wave peak velocity,DTE,and Vp)depend on alignment and sample volume location,and on loading conditions [23].
Profile of the velocity of the mitral annulus,measured in tissue Doppler

Fig.2 Pulsed-wave Doppler imaging of the mitral valve shows peak E wave velocity (E),peak A wave velocity (A),and deceleration time (DT)
Tissue Doppler allowsthe measurement of the displacement velocity of the mitral annulus [23].Tissue Doppler Imaging(TDI) appears to be influenced little by the load conditions and the geometry of the cardiac structures,and it could better reflect relaxation of the LV than the parameters obtained in spectral Doppler [23].The DTI parameters selected by theAmerican SocietyofEchocardiography Pediatric and Congenital Heart Disease Councilare:peakse’ (or Ea)which corresponds with fast filling of the LV starting when the pressure of the LV becomes less than that of the LA,a’ which corresponds with the auricular contraction ands’ for systolic contraction;the isovolumic contraction time(IVCT),the isovolumic relaxation time (IVRT),andE/e’[23].The measurements of these parameters depend on alignment and loading conditions,and are not useful for regional wall motion abnormalities.A normal e’ or Ea wave is > 8 cm/s.Moreover,theE/e’ ratio reflects the ventricular filling pressure;E/e’< 10:normal filling pressure;E/e’between 10 and 15:intermediate pressure;E/e’> 15:high pressure [10].
Although theE/e’ ratio can be used to evaluate the LVEDP in adults,it is less reflective of the filling pressure.Ezon et al.found a weak correlation between the LVEDP and this parameter in patients with dilated cardiomyopathy[28].Moreover,Masutani et al.showed similar findings in a cohort of heterogeneous pediatric patients [29].These studies showed that LVEDP cannot be evaluated using only theE/e’ ratio;rather,a combination of parameters may be more appropriate than relying on a single value.Furthermore,in the setting of systolic dysfunction,this is not much of an issue,because myocardial relaxation and DF are abnormal in this setting,as demonstrated by the reduced septal and laterale’ waves in nearly 90% of patients with systolic dysfunction.
The coupling of the systolic and diastolic functions is a new concept that is becoming well established and recognized.These two phases of the cardiac cycle are closely interrelated,such as according to the Frank—Starling law where enhanced filling increases contractility [30].Courtois et al.showed that ventricular geometry and LV myofiber orientation allow a twisting motion during systole,followed by an untwisting motion during diastole.This late phase creates a pressure gradient inside the LV from the base to the apex,sucking blood from the atrium to the LV [31].This systolic—diastolic coupling is poorly evaluated using the conventional Doppler parameters,except for tissue-Dopplerderived annular velocities (S’) at the septal and lateral LV walls.Friedberg et al.used these parameters in patients with dilated cardiomyopathy to evaluate this coupling and showed a relationship between theS’/e’ ratio and ventricular dysfunction [32].Patients with hypertrophic cardiomyopathy have delayed untwisting with reduced systolicS’ and diastolic myocardiale’ wave velocities [33].

Fig.3 Tissue Doppler echocardiography of the lateral mitral valve shows the e’and a’ waves,the isovolumic contraction time (IVCT),and the isovolumic relaxation time (IVRT)
2D speckle tracking (natural acoustic markers) or 2D strain
This parameter is based on identification of the ventricular walls on several planes representing the deformation of an object relative to its original shape.Since the advent of posttreatment of images,some intensive-care units have taken an interest in studying DF by 2D strain,particularly with septic shock [34,35].
When should DF be evaluated in pediatric intensive-care patients?
In adults,the most robust Doppler parameters for assessing the LV filling pressure are the transmitral velocity profile and the measurement of theE/e’ wave ratio.In a population of cardiac patients (with spontaneous ventilation) with altered LVEFs,anE/Aratio > 2 and an E-wave deceleration time of < 120 ms predicted an elevated pulmonary arterial occlusion pressure (PAOP,which is a reflection of the pulmonary pressures) of > 20 mmHg,with a specificity close to 100% [36].When the mitral profile was different,anE/e’ratio > 15 identified a PAOP > 15 mmHg,with a sensitivity and specificity close to 90% [37].In another study,the same PAOP threshold was predicted by anE/e’ ratio > 10,with a sensitivity of 97% and a specificity of 78% [38].In a population of mechanically ventilated patients in intensive care,anE/Aratio > 2 indicated a PAOP of > 18 mmHg,with a positive predictive value close to 100% [39].When theE/e’ ratio was > 8,it predicted a PAOP of > 18 mmHg,with a sensitivity of 83% and a specificity of 88% [40].However,pediatric studies have not been reported to validate the use of theE/e’ ratio or other parameters for detecting increased PAOP or filling pressures.
Sepsis (Table 2)
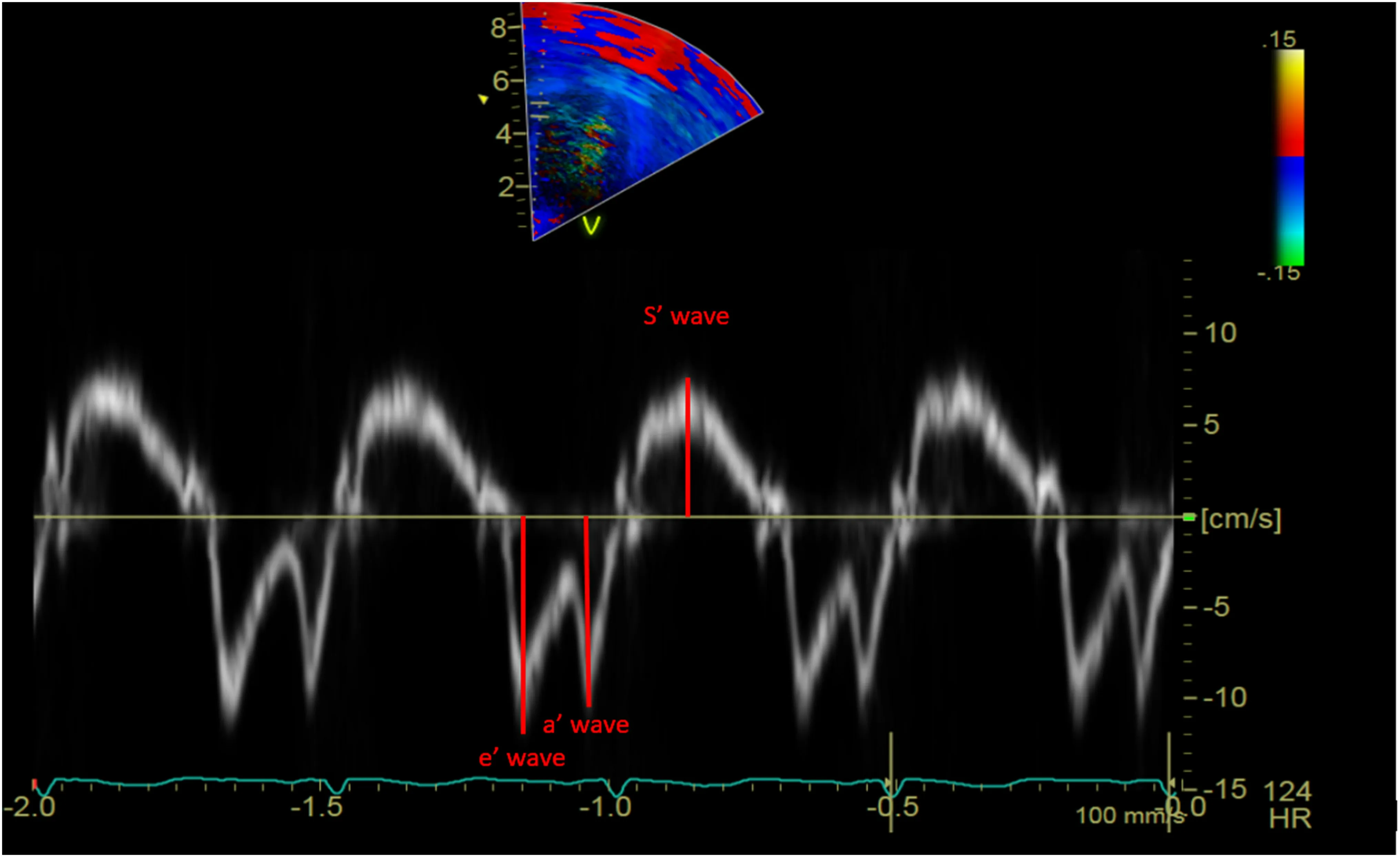
Fig.4 Pulsed-wave tissue Doppler echocardiography of the lateral mitral valve shows the Ea wave (e’),Aa wave (a’),and the systolic wave (S’)
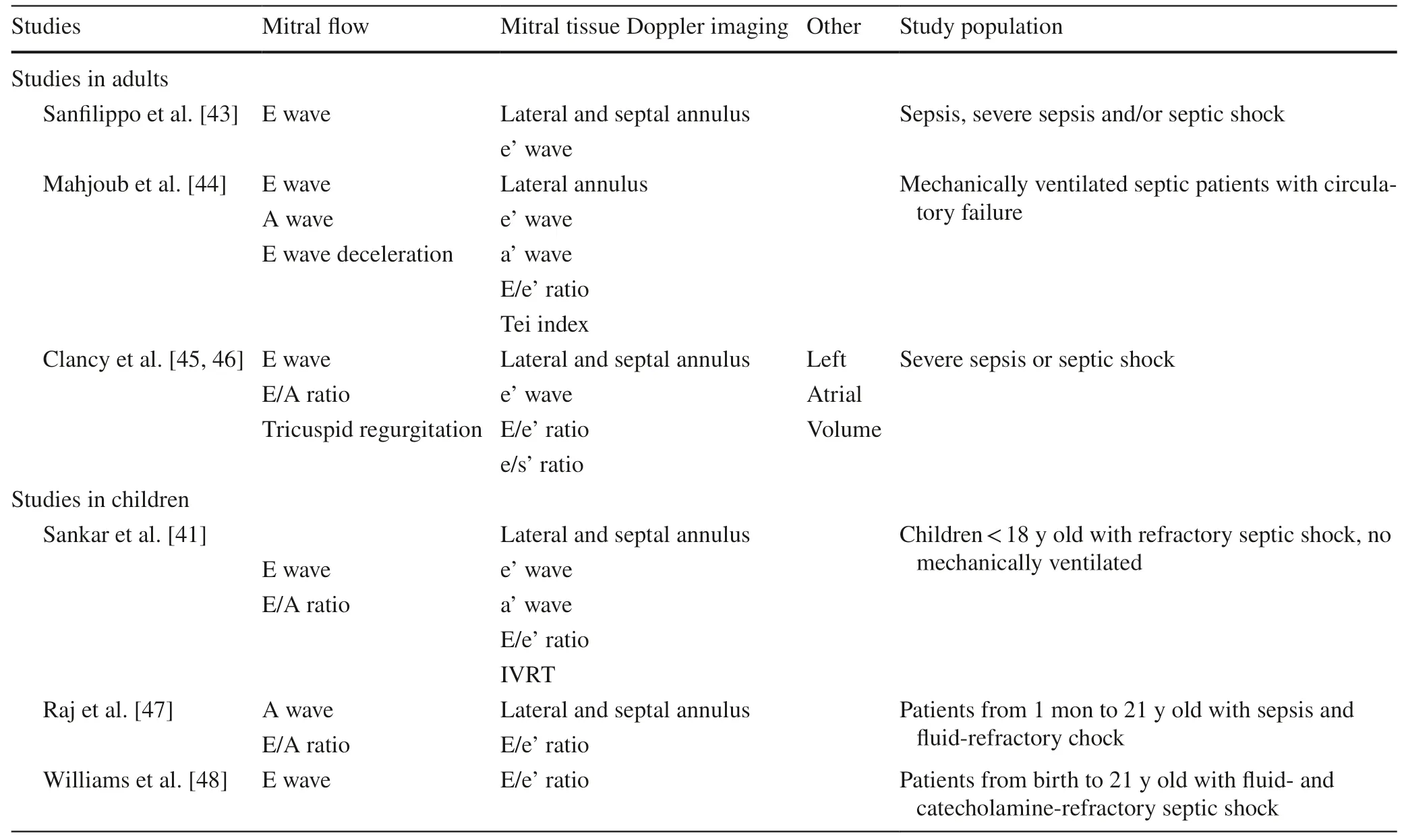
Table 2 Parameters used to assess diastolic function
The prevalence of diastolic heart failure associated with sepsis in the pediatric population was described by Sankar et al.as being comparable to its prevalence among adults[41].In adults,diastolic dysfunction is a good prognostic factor,according to Parker et al.,allowing a better cardiac adaptation to the systolic depression induced by sepsis [42].On the other hand,other studies have recently suggested that diastolic dysfunction is predictive of mortality in adults experiencing septic shock [43].Mahjoub et al.found that in 83 adults with septic shock and diastolic dysfunction,the variation of theE/e’ ratio (∆E/∆e’) was significantly higher in those responding to volume expansion than in nonresponders.This suggests that theE/e’ ratio could be an index of volume expansion tolerance,which is due to the correction of hypovolemia in septic shock,suggesting improved LV relaxation and thereby allowing a better stroke volume and better coronary and myocardial perfusion [44].Clancy et al.suggested that the e’/S’ ratio may be an indicator of worsening intrinsic myocardial relaxation that is relatively load-independent (compared with theE/AandE/e’ ratios) in patients with hyperdynamic circulation [45,46].
Sankar et al.showed that in 56 septic children with spontaneous ventilation and not receiving vasoactive agents within the first 6 hours after admission to pediatric intensive care,41% had diastolic heart failure with a 43% mortality rate;25% had systolic heart failure with a 16% mortality rate [41].In a prospective study involving 30 children with septic shock,Raj et al.demonstrated that 33% of the patients exhibited diastolic heart failure,without a significant correlation between diastolic heart failure and mortality [47].Moreover,in a retrospective study,Williams et al.showed no correlation between LV diastolic dysfunction and mortality,vasoactive-inotrope score,biological parameters (lactates and B-type natriuretic peptide) and the duration of mechanical ventilation [48].
Inotrope adjustment
The use of dobutamine is widespread in pediatric intensivecare patients,despite there being limited published information regarding the consequences of its administration and dosing on DF.In light of its beta-agonist effects that increase myocardial contractility,dobutamine increases the stroke volume and cardiac output.In adults receiving dobutamine infusions,some teams,therefore,have described decreases in filling pressure,LV volume,E/e’ ratio,and isovolumic relaxation time [49].During septic shock,patients are tachycardic;therefore,their diastolic time is shortened,and their LV filling time is reduced.To compensate for this decrease in diastolic time,the LV relaxation phase is accelerated,although the mechanism is altered in patients with sepsis.Morelli et al.,in a randomized trial that included 144 septic patients,observed a decreased need for inotropes and improved myocardial performance in the continuous beta-blocker group compared with the conventional treatment group [50].They did not specifically assess diastolic function by echocardiography;however,they concluded that lowering the heart rate by a beta-blocker allows for a better ventricular filling during diastole,hence,improving stroke volume and thereby improving the efficiency of myocardial work and oxygen consumption [50].Being able to increase diastolic function in septic patients would allow for an optimal management,showing that the evaluation of diastolic function is essential in these patients.However,pediatric studies have not reported the evaluation of diastolic parameters during the administration of cardiac therapeutics.
Evaluation of the potential for weaning from mechanical ventilation
The weaning from mechanical ventilation can be considered as an exercise with an increased respiratory load,cardiac load,and oxygen demand.In adults,increased LV filling pressures,caused by both increased venous return (secondary to the use of spontaneous ventilation) and LV afterload,are likely to result in cardiogenic pulmonary edema,referred to as“weaning PAOP”[51].In 2002,Marcelino et al.showed that the isovolumic relaxation time was predictive of successful weaning from mechanical ventilation[52].Lamia et al.showed that increasedE/A(> 0.95) andE/e’ (> 8.5) ratios are predictive of increases in the left filling pressure (PAOP,> 18 mmHg),with a sensitivity of 82%and a specificity of 91%,in patients who had difficulty being weaned from mechanical ventilation [53].
However,to our knowledge,data have not been published regarding the effect of mechanical ventilation on DF or echocardiographic factors that predict mechanical ventilation weaning failures in pediatric intensive-care patients.Table 3 summarizes the main diseases which might be included in an echocardiographic diastolic dysfunction assessment.
Conclusions
Compared with adults,the evaluation of LV DF is more complex and remains rarely performed in children.Moreover,the lack of knowledge regarding LV DF in children and its aspects that are specific to pediatric cases creates difficulties in the analysis of certain parameters.The evaluation of LV DF should be part of the echocardiographic parameters considered in some situations,such as evaluating responsesto vascular filling in patients with sepsis,evaluating inotrope adjustments,and planning for weaning from mechanical ventilation.
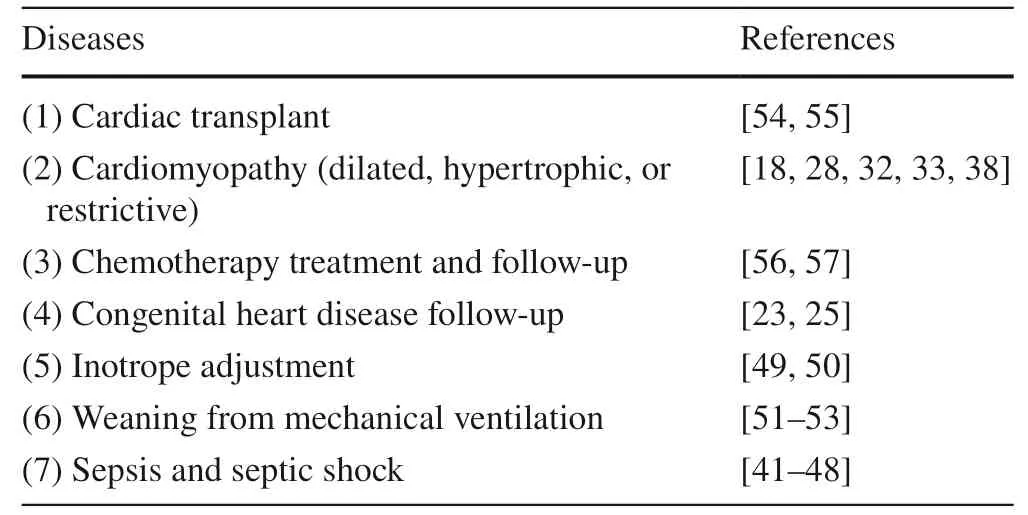
Table 3 Category of pediatric diseases which may require an echocardiographic diastolic dysfunction assessment in pediatric intensive care unit
In children,having more specific algorithms for use in various situations in the pediatric intensive-care unit that take into account clinical,echocardiographic (two-dimensional,DTI),and biological (troponin IC,N-terminal-pro-B-type natriuretic peptide) data would be useful.Additional clinical studies also would allow some of these parameters to be validated in pediatric intensive-care patients and would facilitate the development of a decision algorithm suitable for use in current clinical practice.
Author contributionsDr.MR and Dr.AB conceptualized the study,conducted the initial analyses,drafted the initial manuscript,reviewed,and revised the manuscript;Dr.JS and Dr.JBB reviewed and revised the manuscript;Pr.FG reviewed and revised the manuscript;Prof.SL conceptualized the study,reviewed and revised the manuscript.All authors have approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FundingNo financial or nonfinancial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Compliance with ethical standards
Ethical approvalNot required for this review article.
Conflict of interestThe authors have no conflicts of interest relevant to this article to disclose.
 World Journal of Pediatrics2021年1期
World Journal of Pediatrics2021年1期
- World Journal of Pediatrics的其它文章
- Why COVID-19 is less frequent and severe in children:a narrative review
- Laboratory diagnosis of COVID-19 in secondary care hospitals in India:will standalone serology suffice?
- Winter is coming:care of the febrile children in the time of COVID-19
- Addressing e-cigarette health claims made on social media amidst the COVID-19 pandemic
- Social responsibilities of a pediatric journal:considerations and future directions
- Surrogate markers and predictors of endogenous insulin secretion in children and adolescents with type 1 diabetes
