Nonalcoholic fatty liver disease as a risk factor for cytomegalovirus hepatitis in an immunocompetent patient: A case report
Bashar Khiatah, Laya Nasrollah, Stephen Covington, Deborah Carlson
Bashar Khiatah, Deborah Carlson, Internal Medicine, Community Memorial Hospital, Ventura,CA 93003, United States
Laya Nasrollah, Stephen Covington, Department of Gastroenterology, Community Memorial Hospital, Ventura, CA 93003, United States
Abstract BACKGROUND Almost 80 percent of adults in the United States have had cytomegalovirus (CMV)infection by age 40. The number of symptomatic CMV hepatitis cases has been increasing along with non-alcoholic fatty liver disease (NAFLD) cases in the United States that is estimated to be 25 percent of the population. In this paper,we try to link these two entities together.CASE SUMMARY In this case report, we describe a young female who presented with fever, nausea,and vomiting who was found to have NAFLD and CMV hepatitis that was treated supportively.CONCLUSION In this case report, we describe NAFLD as a risk factor for CMV hepatitis and discuss the possible impact on clinical practice. We believe, it is essential to consider NAFLD and it’s disease mechanisms’ localized immu-nosuppression, as a risk factor of CMV hepatitis and severe coronavirus disease 2019 infection.
Key Words: Non-alcoholic fatty liver disease; Cytomegalovirus hepatitis; Immunocompetent; Female health; Global impact; Hepatology; Case report
INTRODUCTION
Cytomegalovirus (CMV) is a herpesviridae family member that causes a spectrum of human illness that is mostly dependent on the host. Infection in an immunocompetent patient is usually asymptomatic or might present as a mononucleosis syndrome.Occasionally, primary CMV infection can lead to severe organ-specific complications with significant morbidity and mortality[1,2]. CMV hepatitis in immunocompetent patients has been reported frequently in the literature, increasing the awareness of this disease[3]. Reports over the last decade have informed us that non-alcoholic fatty liver disease (NAFLD) is a multisystem disease affecting multiple extrahepatic organs and regulatory pathways, proving that NAFLD's clinical burden is not limited to liverrelated morbidity and mortality[4]. NAFLD is an excessive infiltration of fat in the liver in individuals not consuming or consuming in small amounts of alcohol defined as ≤20 g per day for women and ≤ 30 g per day for men. Diagnosis usually requires the elimination of secondary causes of fatty infiltration of the liver, including hepatitis C virus infection, the use of glucocorticoids, celiac disease, Wilson disease, familial hypobetalipoproteinemia, and autoimmune disorders[5].
CASE PRESENTATION
Chief complaints
Six-day history of fever, night sweats, myalgia, nausea, and vomiting.
History of present illness
A 34-year-old Hispanic female presents to the emergency room (ER) with a six-day history of fever, night sweats, myalgia, nausea, and vomiting. Coronavirus disease 2019 testing was negative, and she was sent home on antiemetics. She developed intermittent abdominal pain in the right upper quadrant of 5/10 intensity, sharp, nonradiating associated with mild headache and lightheadedness that prompted her to return to the ER. She has no sick contacts. She is up to date on her vaccinations,monogamous, practices all social distancing precautions, and is a housewife and a mother of 3 healthy children. She denies having pain with any specific foods,including fatty foods, recent travel, IV drug abuse, alcohol, smoking, and all other symptoms. Her only medications were Ondansetron and Acetaminophen.
History of past illness
Remote history of intermittent asthma.
Personal and family history
Family history is remarkable for diabetes.
Physical examination
On physical exam, her body mass index is 33.1 kg/m²; she has a temperature of 101.2 F and is mildly tender to palpation in the epigastric area. Otherwise, her physical exam is benign.
Laboratory examinations
Laboratory studies are shown in Table 1 and 2.
Imaging examinations
Radiologic studies revealed fatty liver, as shown in Figure 1 and 2, compared to normal liver imaging in 2015.
FINAL DIAGNOSIS
CMV Hepatitis in the setting of NAFLD. She is admitted for observation and found to have CMV hepatitis, as shown in Table 1 and 2.
TREATMENT
Supportive treatment with Ibuprofen 400 mg every 6 h for fever.
OUTCOME AND FOLLOW-UP
She was discharged home and instructed to follow up with both her primary care doctor and the Gastroenterologist. Education was provided on a low-fat diet, exercise,and the importance of weight loss. One week after discharge, she was seen in the primary clinic for follow up. She reported continuous yet less frequent symptoms of fever, myalgias, and night sweats controlled with Acetaminophen, Ibuprofen, and Ondansetron. Her liver enzymes were trending down. Two weeks after discharge, she was symptom-free with normalized liver enzymes.
DISCUSSION
The liver is a unique immune environment containing lymphocytes, monocytes,Kupffer cells, Natural-killers, astrocytes dendritic, and many other immigrant cells associated with the immune system. It is responsible for synthesizing various proteins such as acute-phase proteins, complements, cytokines, chemokines, lipid messengers,and reactive oxygen species. Insulin resistance, oxidative stress, endoplasmic reticulum stress, endotoxins from the intestinal flora, and genetic predispositions are all involved in developing NAFLD, causing an imbalance of the immune system in the liver[4,5]. This imbalance translates as an elevation of Interleukin-6 (IL-6), IL-15, IL-17,IL18, Tumor Necrosis Factor-alpha, Interferon gamma-induced protein 10, and Transforming growth factor beta-3[5]. A recently published study where authors reported NAFLD's significance as a significant risk factor affecting the severity of coronavirus disease 2019 emphasizes the importance of this imbalance[6].
CONCLUSION
Finally, in the United States, with an estimated 25 percent of the population with NAFLD, and almost 80 percent of adults having CMV infection by age 40, it is essential to consider NAFLD and it’s disease mechanisms’ localized immunosuppression, as a risk factor of CMV hepatitis. Further studies and research are required to understand NAFLD as a risk for viral diseases.
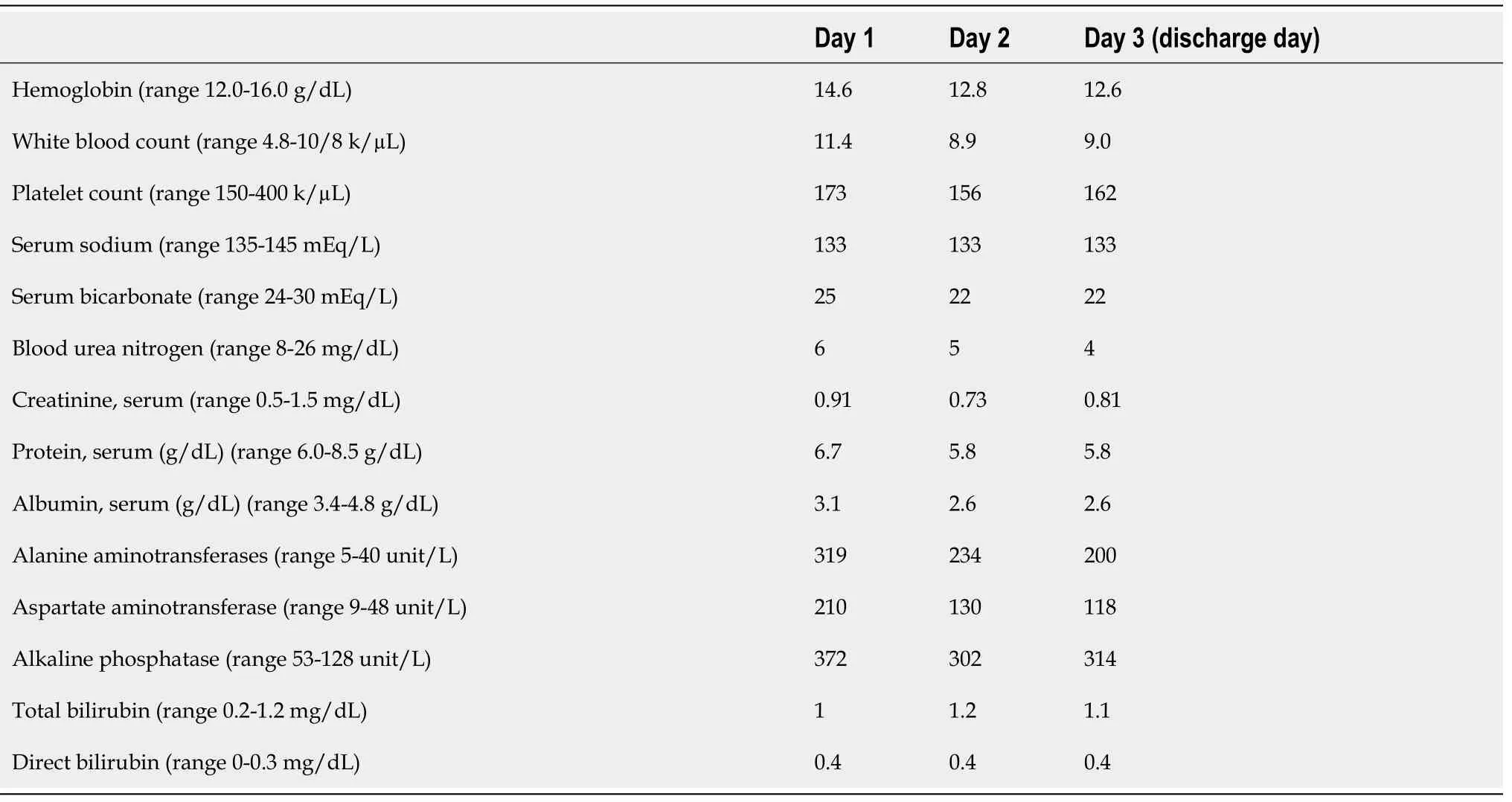
Table 1 Laboratory trend
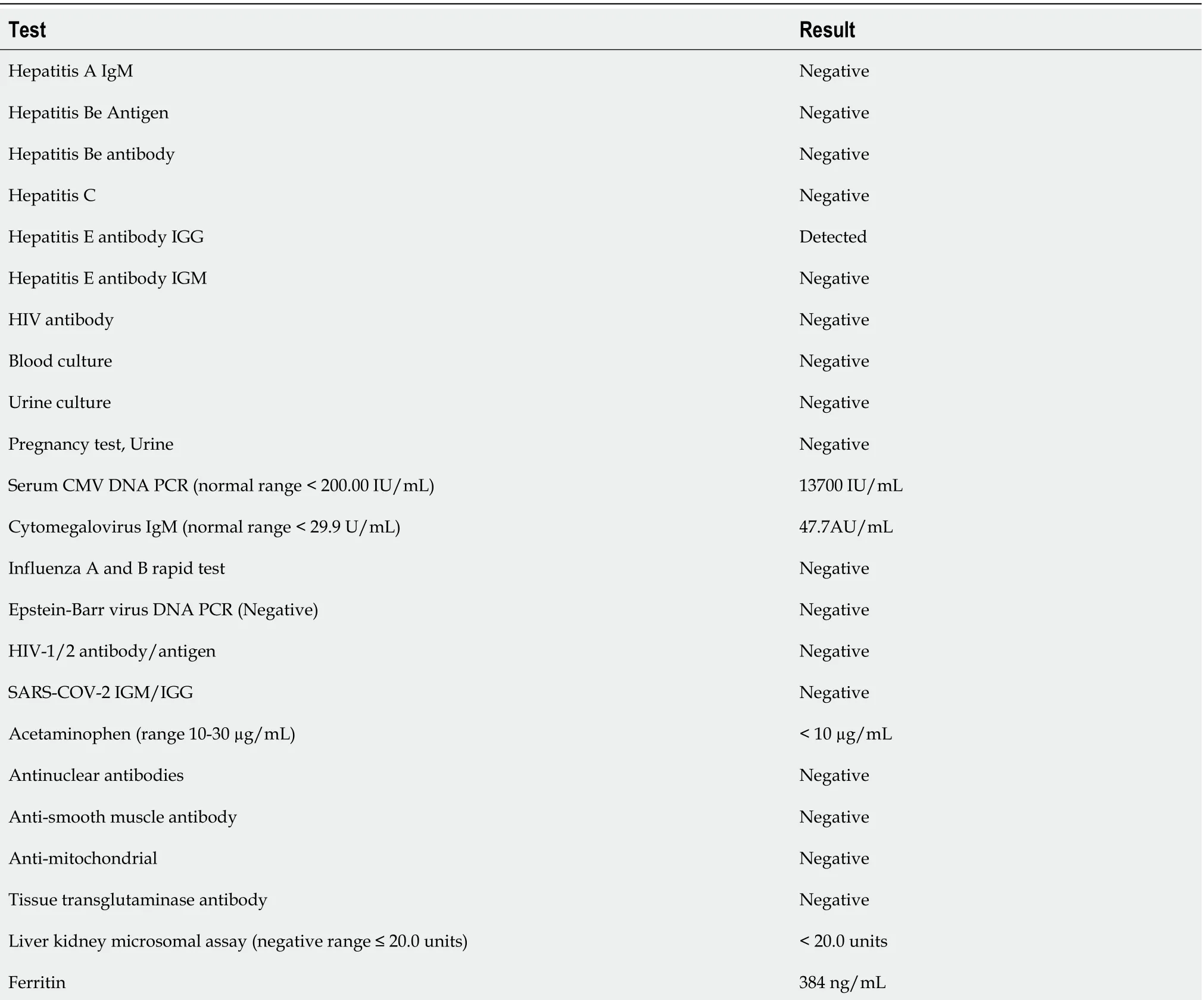
Table 2 Hepatitis workup
CMV: Cytomegalovirus; PCR: Polymerase chain reaction; SARS-COV-2: Severe acute respiratory syndrome coronavirus; IGG: Immunoglobulin G.

Figure 1 Intrahepatic vessels appear unremarkable including the hepatic veins. Increased liver echogenicity with moderately enlarged liver most consistent with fatty infiltration. Mild heterogeneous liver around the gallbladder fossa likely related parenchymal sparing in an otherwise fatty liver.

Figure 2 Magnetic resonance cholangiopancreatography results. Mild hepatosplenomegaly and hepatic steatosis.
 World Journal of Clinical Cases2021年6期
World Journal of Clinical Cases2021年6期
- World Journal of Clinical Cases的其它文章
- Postoperative discal pseudocyst and its similarities to discal cyst: A case report
- Gastrointestinal stromal tumor with multisegmental spinal metastases as first presentation: A case report and review of the literature
- Polidocanol sclerotherapy for multiple gastrointestinal hemangiomas: A case report
- Congenital hepatic fibrosis in a young boy with congenital hypothyroidism: A case report
- Intrahepatic cholangiocarcinoma is more complex than we thought:A case report
- Early reoccurrence of traumatic posterior atlantoaxial dislocation without fracture: A case report
