Efficacy of afatinib in a patient with rare EGFR (G724S/R776H)mutations and amplification in lung adenocarcinoma: A case report
Shu-Yan He, Qing-Feng Lin, Jie Chen, Gui-Ping Yu, Jun-Ling Zhang, Dong Shen
Shu-Yan He, Qing-Feng Lin, Jie Chen, Dong Shen, Department of Medical Oncology, The Jiangyin Clinical College of Xuzhou Medical University, Jiangyin 214400, Jiangsu Province,China
Gui-Ping Yu, Department of Cardiothoracic Surgery, The Affiliated Jiangyin Hospital of Southeast University, Jiangyin 214400, Jiangsu Province, China
Jun-Ling Zhang, Medical Department, 3D Medicines Inc., Shanghai 201114, China
Abstract BACKGROUND The most common EGFR mutations are in-frame deletions in exon 19 and point mutations in exon 21. Cases with classical EGFR mutations show a good response to EGFR tyrosine kinase inhibitors (TKIs), the standard first-line treatment. With the development of next generation sequencing, some uncommon genomic mutations have been detected. However, the effect of TKIs on such uncommon EGFR mutations remains unclear.CASE SUMMARY Here, we report a case of rare EGFR co-mutation in non-small cell lung cancer and the efficacy of afatinib on this EGFR co-mutation. A 64-year-old woman was diagnosed with thoracolumbar and bilateral local rib bone metastases, bilateral pulmonary nodules, and pericardial and left pleural effusion. The pathological diagnosis was lung adenocarcinoma. To seek potential therapeutic regimens, rare co-mutation comprising rare EGFR G724S/R776H mutations and amplification were identified. The patient experienced a significant clinical response with a progression-free survival of 17 mo.CONCLUSION A case of non-small cell lung cancer with rare EGFR G724S/R776H mutations and EGFR amplification responds well to TKI treatment.
Key Words: EGFR G724S and R776H; Afatinib; Non-small cell lung cancer; Case report
INTRODUCTION
Non-small cell lung cancer (NSCLC) is the leading cause of cancer death, especially in developing countries such as China[1]. A recent study shows that in 2015 there were about 733000 newly diagnosed cases of NSCLC in China, with approximately 610000 Chinese patients dying from the disease[2]. NSCLC accounts for the majority (75%) of clinical lung cancer cases. Adenocarcinoma is the most common histological type of NSCLC and can be subdivided into different clinically relevant molecular subtypes according to the type of driver gene mutation.
EGFRwas the first identified targetable oncogenic driver discovered in NSCLC[3].Approximately 40% of Asian patients with newly diagnosed metastatic NSCLC harbor a somatic mutation in theEGFRgene[4]. The most commonEGFRmutations are inframe deletions in exon 19 and point mutations in exon 21. However, rare mutations were found in nearly 10%-15% ofEGFR-positive NSCLC cases[5,6]. Although it has been reported that afatinib is effective against rareEGFRmutations, there are significant differences in progression-free survival (PFS) and overall survival (OS) among patients with different rareEGFRmutations[7]. Here, we describe a rare case ofEGFR G724S/R776Hmutations andEGFRamplification in an NSCLC patient responding to afatinib.
CASE PRESENTATION
Chief complaints
A 64-year-old nonsmoking woman visited our hospital on April 26, 2019 for further treatment because she could not tolerate the side effects of previous chemotherapy for lung adenocarcinoma, including myelosuppression and cardiac and renal insufficiency.
History of present illness
Chest computed tomography (CT) showed bone metastases in the thoracolumbar spine and bilateral local ribs, nodules in both lungs, and pericardial and left pleural effusion.
History of past illness
On September 10, 2014, the patient went to a local hospital because of sudden glossolalia with right lower limb numbness, and was diagnosed with stage IIIA lung adenocarcinoma, and then she underwent resection of the upper lobe on September 24, 2014 (Figure 1A). The patient received pemetrexed combined with carboplatin for four cycles of chemotherapy. In November 2015, the disease progressed. The patient was given paclitaxel plus cisplatin combined with bevacizumab for six cycles from November 11, 2015 to March 11, 2016. From April 1, 2016 to April 26, 2019, the patient received pemetrexed combined with bevacizumab, and his condition remained stable(Figure 1B). After the last cycle of treatment with pemetrexed plus bevacizumab, chest CT showed bone metastases in the thoracolumbar spine and bilateral local ribs,nodules in both lungs, and pericardial and left pleural effusion (Figure 1C).

Figure 1 Diagnosis and treatment of the patient’s disease. A: Treatment of lung adenocarcinoma using different regimens; B: Imaging diagnosis during pemetrexed plus bevacizumab treatment; C: Imaging diagnosis before afatinib therapy; D: Pathological diagnosis.
Laboratory examinations
The previous pathological diagnosis was lung adenocarcinoma (Figure 1D).
Imaging examinations
After the last cycle of treatment with pemetrexed plus bevacizumab, CT showed bone metastases in the thoracolumbar spine and bilateral local ribs, nodules in both lungs,and pericardial and left pleural effusion (Figure 1C).
FINAL DIAGNOSIS
Because the patient could not tolerate the side effects of chemotherapy, potential therapeutic regimens were sought. Her blood was subjected to NGS analysis, and a rareEGFR G724S[mutant allele frequency (MAF): 67.59%] mutation in exon 18 andR776H(MAF: 40.54%) mutation in exon 20 as well as amplification was identified(Figure 2). Therefore, the patient was finally diagnosed with lung adenocarcinoma with rareEGFR G724SandR776Hmutations and amplification.
TREATMENT
Based on the above findings, the patient was administered with afatinib (30 mg qd)combined with bevacizumab and followed regularly.
OUTCOME AND FOLLOW-UP
After 4 mo of treatment, the left pleural effusion and pericardial effusion were significantly reduced and the patient showed SD according to the Response Evaluation Criteria in Solid Tumors, version 1.1 (Figure 3). The MAFs for bothR776HandG724Swere also decreased (R776Hfrom 40.54% to 0.16% andG724Sfrom 67.59% to undetected). During this period, zoledronic acid was irregularly given for anti-bone metastasis therapy. The patient was followed several times, and CT performed on July 10, 2020 showed that the tumor lesion of the right lung remained stable (Figure 3).However, the reexamination on October 25, 2020 revealed disease progression with multiple bone metastases (Figure 4). Imaging studies indicated progressive disease(PD), and the patient's final PFS was 17 mo. There were no obvious adverse reactions during the treatment.
DISCUSSION
In the era of precision medicine,EGFRgenotyping has become the standard practice for NSCLC, but the identification of rare mutations does not necessarily imply clear targeted therapeutic action. Due to the small number and high heterogeneity of patients with rare mutations, the efficacy of EGFR TKIs in patients with rareEGFRmutations remains unclear. However, a large number of clinical studies have shown significant differences in the efficacy of EGFR TKIs in patients with rare mutations inEGFR. Therefore, these patients should be analyzed separately in clinical studies to provide them with more effective individualized treatment.
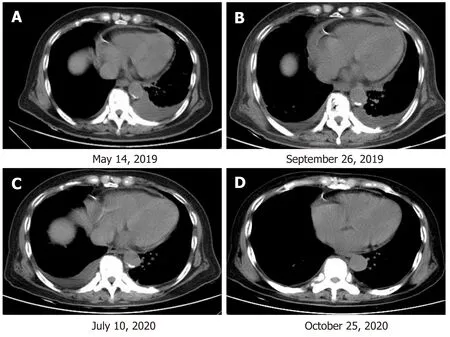
Figure 3 The patient’s clinical course including treatment history and relevant imaging studies. A: At baseline before therapy with afatinib combined with bevacizumab; B: At 4 mo of therapy with afatinib combined with bevacizumab, with an SD response; C: At 14 mo of therapy with afatinib combined with bevacizumab, with an SD response. D: At 17 mo of therapy with afatinib combined with bevacizumab, with a progressive disease response.
As a second-generation EGFR TKI, afatinib is more effective than chemotherapies and first-generation EGFR-TKIs[8,9]. In LUX-Lung 7 and LUX-Lung 8 studies, it was found that patients treated with afatinib as both first-line treatment (compared with gefitinib) and second-line treatment (compared with erlotinib) resulted in a longer PFS or OS[10,11]. However, most patients with rare or complexEGFRmutations had a shorter PFS than patients with exon 19 deletion (16.0 movs9.0 mo; HR, 0.34; 95%CI, 0.13-0.94,P= 0.037)[12]. In addition, it has been reported that patients aged ≥ 65 years with rare mutations have significantly longer PFS than patients aged < 65 years after receiving EGFR TKIs (median PFS: 10.5 movs5.5 mo,P= 0.0320)[13]. Patients with rareEGFRmutations are often excluded from clinical trials. However, these adverse characteristics are frequently encountered in clinical practice, and in particular, rare mutations ofEGFR(two or moreEGFRmutations at the same time) are generally considered a relatively rare event representing a unique and highly heterogeneous subset of NSCLC.
CONCLUSION
In summary, we report a rare case of NSCLC withEGFR G724S/R776Hand amplification, which has never been reported before. The successful use of afatinib in this case may provide a new treatment option for this type ofEGFRco-mutation,especially for patients who decline or are not suitable for chemotherapy. By deepening our understanding of functional and structural differences between rare subtypes ofEGFRvariation, the different responses to EGFR TKIs and overall survival rates of patients with these mutations need to be further studied. This case provides valuable insights for future clinical cancer treatment.

Figure 4 Diagnosis of disease progression in the patient. Whole-body bone scan and organ tomography revealed increased uptake of multiple imaging agents in the skull, spine, ribs on both sides, pelvis composition, and upper left femur, suggesting bone metastasis of the tumor.
 World Journal of Clinical Cases2021年6期
World Journal of Clinical Cases2021年6期
- World Journal of Clinical Cases的其它文章
- Interactive platform for peer review: A proposal to improve the current peer review system
- Animal models of cathartic colon
- New indicators in evaluation of hemolysis, elevated liver enzymes,and low platelet syndrome: A case-control study
- Analysis of hospitalization costs related to fall injuries in elderly patients
- Effect of alprostadil in the treatment of intensive care unit patients with acute renal injury
- Etomidate vs propofol in coronary heart disease patients undergoing major noncardiac surgery: A randomized clinical trial
