Auricular acupoint application combined with Fujing prescription treatment for patients with premature ovarian failure
Wen-Ming Cao,Xiao-Ying Meng,Li-Li Yu,Kui-Mei Zhang,Shu-Ling Zhang,Xiu-Rong Wang*
1Shandong Changle People's Hospital,Weifang 262400,China.
Abstract
Keywords:Fujing prescription,Auricular acupoint application,Premature ovarian failure,Follicle-stimulating hormone levels,Estrogen levels
Background
Premature ovarian failure(POF)is a disease that affects women under 40 due to single or multiple factors such as elevated gonadotropins and decreased estrogen levels[1].In recent years,with the increased pressure,the incidence of premature ovarian failure keeps increasing,which seriously affects people's daily life and health[2].
POF results primarily from depletion of follicles in the ovaries or ovarian damage.The etiology is complex,importantly related to medical,metabolic and immune factors,in addition to infection and genetic factors[3].POF may result from congenital enzyme deficiency. In addition, hormonal abnormalities,follicular insufficiency and depletion,and genetics can also be the factor[4].
There is no concept of premature ovarian failure in traditional Chinese medicine(TCM).It belongs to the category of menstrual diseases and gynecological miscellaneous diseases.It has recorded in Synopsis of Golden Chamber(an ancient book of Chinese medicine written by Zhang Zhongjing born in 150 C.E.–219 C.E.)that cold accumulation,Qi and blood weakness,liver depression and Qi stagnation were the etiology and pathogenesis of premature ovarian failure.On this basis,Causes and Manifestations of All Diseases(an ancient book of Chinese medicine written by Chao Yuanfang in 610 C.E.)further emphasized the pathogenic effect of fatigue,lack of blood and Qi.
Most scholars believed that POF was caused by Qi and blood deficiency.Review of Gynaecology by Chen Su-An(an ancient book of Chinese medicine written by Chen Suan)specially emphasized the occurrence of menstrual disorder and amenorrhea caused by kidney deficiency,blood deficiency,phlegm stagnation and other reasons.Combination of TCM and western medicine has been proved effectively in the POF treatment[6].In this article,Fujing prescription,made of 14 Chinese herbal medicines,were used to treat POF combined by stimulating three auricular acupoints(Shenmen(TF 4),Ovary(TF 2),and Endocrine(TF 6)).The effects were discussed to provide guidance for further clinical application.
Data and methods
Informations and Methods
The 100 patients were randomly divided into the control and treatment group.
Enrollment criteria.(1) All participants were diagnosed with POF by gynecological and ultrasound examination(refer to the ninth edition of Obstetrics and Gynecology.(2)All participants did not receive any hormone therapy in the past 3 months.(3)They were between 26 and 40 years of age.(4)All participants were informed and agreed to this study.(5)Approved by the hospital ethics committee(Shandong Changle People’s Hospital,NO.201803152213).
Exclusive criteria.(1)Patients with severe functional disorders of vital organs such as liver and kidney.(2)Patients with ovarian tumors,pelvic tuberculosis and polycystic ovary syndrome. (3) Patients with gynecological organic lesions and previous ovarian surgery.(4)Patients with cognitive dysfunction,psychiatric disorders and allergic disorders.
Methods
The treatment in control group.Taking phentermine(specification,2-10)(Solvay Group,importdrug registration number:H20100159)for 28 consecutive days with a daily dose of 1 tablet,and a cycle of phentermine was continued on the first day of menstruation if menstruation started.The entire course of treatment is 3 months.
The treatment in treatment group.Takeone tablespoon of Fujing prescription a day for 3 months.The auricular acupoint application can stimulate the Shenmen(TF 4)ovar and incretion.
The treatment for both groups of patients lasted for 3 months.In both groups,all sex hormones and glucocorticoids were prohibited for one month before the blood tests were performed.Patients in the treatment group and the control group were tested for their serum hormone levels on the third day of their menstrual cycles by taking venous blood from their elbows on the morning fasting and using the enzyme-linked immunosorbent assay.
Indicators
Treatment efficacy.Refer to the Diagnostic and Therapeutic Effect Standard of Clinical Disease and Syndrome of Traditional Chinese Medicine[7,8].
Recovery criteria.Monthly cycle and menstrual period are within normal range,the menstrual volume is 30–50 ml,the patient's hormone levels are tested and found to be back to normal,all clinical symptoms disappear,and ultrasound shows that ovulation is normal.
Improvement criteria. menstruation showed intermittent menstrual flow,less menstrual volume,clinical symptoms improved,however,the patient still had flushing,hot flashes and easy sweating,mood swings,less leucorrhoea,vaginal dryness,and low libido symptoms,significantly less than before.Hormone levels were close to normal,and there was no dominant follicle on color ultrasound.
Ineffective indications.no improvement in clinical symptoms, future menstruation, hormone level measurements and ovulation tests are not significantly changed compared to pre-treatment[7].
Total effective rate(%)=(Improvement+Recovery)/Total×100
Symptom scores.The patients were scored before and after one course of treatment.
Estrogen level.Test the serum levels of follicle stimulating hormone, estradiol and luteinizing hormone before and after one course of treatment.
Pre-and post-treatment serum levels of reproductive hormones.5 mL of fasting venous blood was collected from the two groups respectively,and the serum was taken after centrifugation.Automatic biochemical analyzer and radioimmunoassay detected the indicators of follicle stimulating hormone(FSH),luteinizing hormone(LH)and estradiol.
Pre-and post-treatment serum immunity indexes.The immunoglobulin G(IgG),immunoglobulin M(IgM)and immunoglobulin A(IgA)levels are tested with immunoturbidimetric assay using an automatic biochemical analyzer.
Assessment of adverse reactions.Primarily includes the occurrence of conditions such as abdominal distension,nausea and vomiting,irregular bleeding and breast discomfort.
Statistical methods
The t-test was conducted using SPSS 19.0 software.The χ2or Fisher’s exact test was used for the comparison of counting data,and the t-test was used for the comparison of sample means.
Results
General data
From March 2018 to March 2020,100 patients with hypovolemia were selected who attended our outpatient clinic,59 of whom showed significant irritability,vaginal interference,insomnia and night sweats,20 had no significant symptoms,and 21 had a need to have children.The 100 patients were randomly divided into a control group of 50 patients and a treatment group of 50 patients.The age,amenorrhea time,complications and pregnancy history of the two groups were comparable.The age,amenorrhea time,complications and pregnancy history of the two groups were comparable.There was no significant difference in the basic data between the two groups(P>0.05).The study was reviewed and approved by the Ethics Committee at the same time.
Comparison of clinicaloutcomes between two groups of patients
In the control group,14 cases were cured,24 cases improved and 12 cases ineffective,with a total effective rate of 76%.In the treatment group,23 cases were cured,19 cases improved and 8 cases ineffective.The total effective rate was 84%.Treatment group was significantly more effective than the control group,and the difference was comparable(P<0.05),see Table 1.
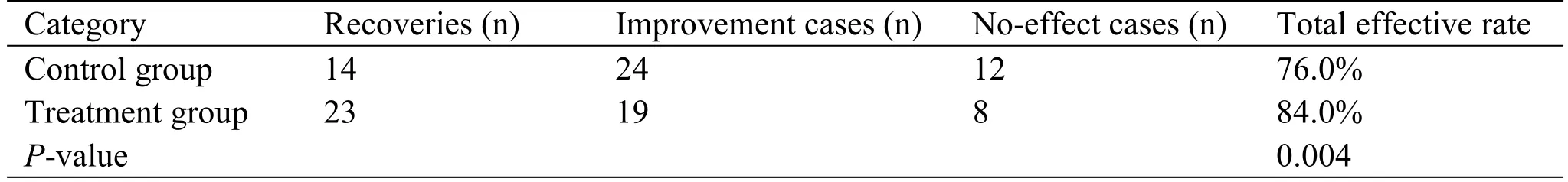
Table 1 Comparison of clinical treatment results between two groups of patients(n,%)
Comparison of TCM evidence points between two groups of patients according to pre-treatment
Before treatment,the TCM syndrome score was 14.13±3.21 in the control group and 12.87±3.52 in the treatment group.There was no significant difference between the two groups before treatment(P>0.05).After treatment,the TCM syndrome score of the control group was 8.75±4.25,and that of the treatment group was 5.23±4.26 after treatment.The TCM syndrome score of the treatment group was significantly lower than that of the control group(P<0.05),as shown in Table 2.
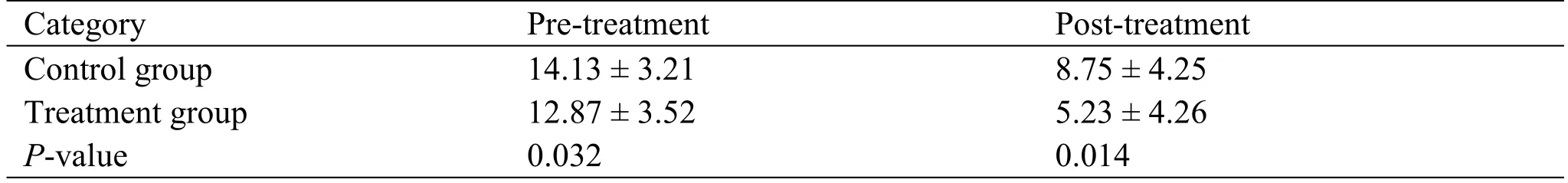
Table 2 TCM syndrome score between two groups of patients according to pre-treatment(n,(mean±SD))
Comparisons of serum follicle-stimulating hormone,estradiol and luteinizing hormone levels in two groups of patients according to pre-treatment
The P-values of follicle stimulating hormone,estradiol and luteinizing hormone in the control group and the observation group were all more than 0.05 before treatment,and there was no statistical significance.In the control group,FSH was 77.15±3.82 IU/l before treatment,while that was 55.17±3.66 IU/l after treatment.In the treatment group,the FSH was 68.12±12.01 IU/l and 26.28±5.97 IU/l,respectively before and after treatment.In the control group,LH was 44.13±5.48 IU/l before treatment and was 38.895.65 IU/l after treatment.In the treatment group,LH was 45.72±3.61 IU/l,before treatment and LH was 28.44±6.21 IU/l after treatment.The treatment methods of the two groups,the FSH and LH of the control group and the treatment group decreased significantly after treatment.The treatment methods of the two groups were effective for premature ovarian failure,but the effect of the treatment group was more obvious.
The level of estradiol in the two groups increased significantly,but the change of the index in the treatment group was more obvious(P<0.05),which was statistically significant,as shown in Table 3.
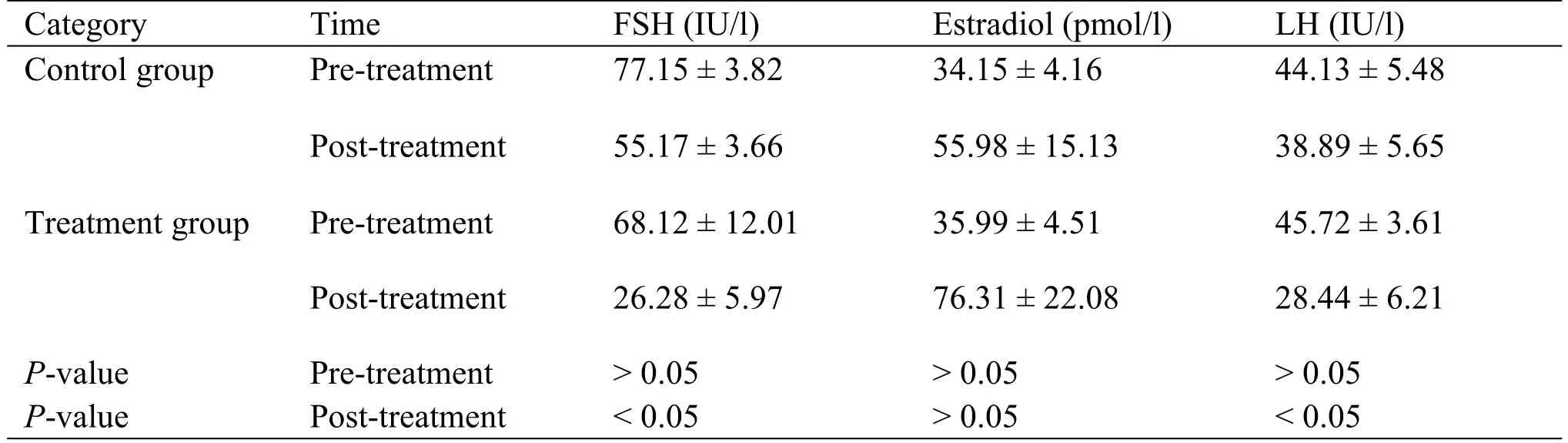
Table 3 The levels of serum FSH,estradiol and LH of the two groups pre-treatment(mean±SD)
Comparison of serum immune parameters between the two groups
The IgG of the control group was 8.7±2.3 g/L and 12.1±4.2 g/L before and after treatment,respectively.The IgG of the treatment group was 8.7±3.1 g/L before treatment and 16.3±4.2 g/L after treatment.
In the control group,the IgM before and after treatment was 1.6 g/L and 1.7 g/L respectively,and the IgM was 1.7 g/kg/L after treatment.In the treatment group,the IgM was 1.7±0.2 g/L before treatment and 2.4±0.5 g/L after treatment,which was statistically significant.
In the control group,IgA was 1.2±0.1 g/L before treatment and 1.4±0.3 g/L after treatment,IgA was 1.4 g/L after treatment.In the treatment group,the IgA was 1.2±0.2 g/L before treatment and 1.9±0.2 g/L after treatment,which was statistically significant.
No significant difference(P>0.05)was found between the basic data of the two groups.
IgG,IgM and IgA indexes are higher in the study group compared with thecontrolgroup in the post-treatment(P<0.05),as shown in Table 4.
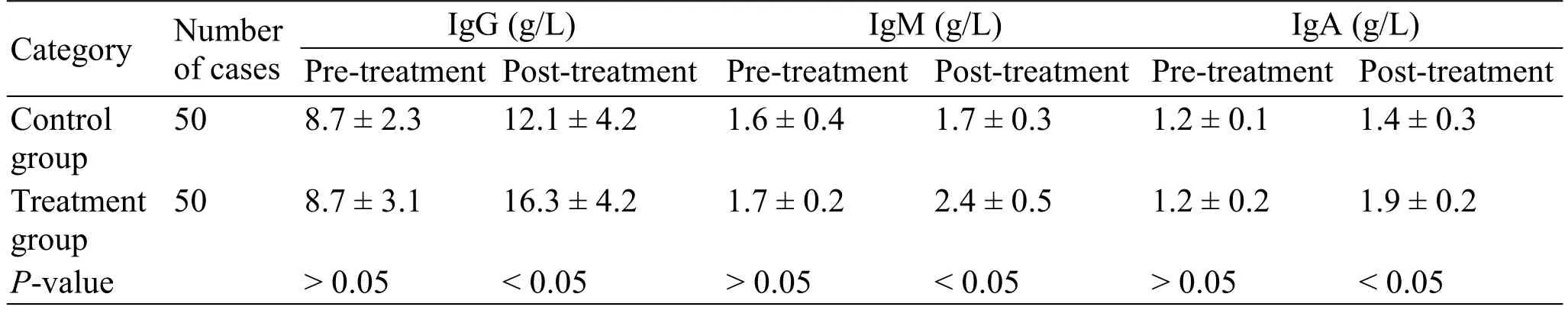
Table 4 Immunoglobulin before and after treatment
Comparison of adverse effects between the two groups
In the control group,there were six cases of abdominal distension,three cases of nausea and vomiting,two cases of irregular bleeding and two cases of breast discomfort,with a total incidence of 26%.In the treatment group,there were four cases of abdominal distension,two cases of nausea and vomiting,two cases of irregular bleeding and one case of breast discomfort,with atotalincidence of 18%.No significant difference(P>0.05)was found between the basic data of the two groups,and this research was reviewed and approved by the ethics committee.The treatment group showed a lower incidence of adverse events compared to the control group(P<0.05),as shown in Table 5.
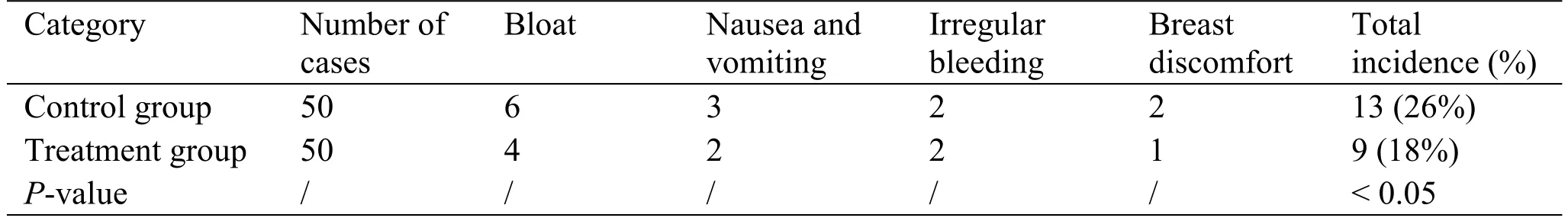
Table 5 Comparison of adverse events in the two groups(cases(n))
Discussion
POF is a disease that affects women under 40 due to single or multiple factors such as elevated gonadotropins and decreased estrogen levels.Most patients present with menstrual disorders,amenorrhea,and infertility[9].About 50% of patients have scanty or irregular uterine bleeding,and 50% of patients have abrupt amenorrhea. Some patients only have symptoms of estrogen deficiency,such as hot flashes,night sweats,irritability and painful intercourse;a minority ofpatients may presentwith primary amenorrhea [10]. The symptoms of estrogen deficiency occur in more than 3/4 of patients,but they are uncommon in patients with primary amenorrhea.In addition,long-term use of estrogen may increase the risk of endometrial cancer,breast cancer and other malignant diseases.
TCM can improve the therapeutic effect,shorten the course of the disease,reduce the recurrence rate,and reduce the side effects of Western drugs[11].Most of the medicinal ingredients in the Fujing prescription can strengthen the liverand kidney.Together with auricular acupoint application,it stimulates the three auricular acupoints:the Shenmen(TF 4),the ovaries and the endocrine acupoints.
The auricular points are the acupuncture points distributed on the auricle,also known as the reaction and stimulation points[12].The Sanmen is located in the triangular fossa,slightly above the upper and lower angular division of the auricle chakra(Figure 1).The ovary acupoint is located at the middle of the inner side of auricle,with the function ofregulating menstruation and nourishing blood,strengthening the spleen and brightening the eyes,strengthening the kidney essence.The endocrine acupoint is located in the front of the ear nail cavity,and is an important acupoint for endocrine and reproductive system diseases,with the functions of regulating the meridians and nourishing blood,benefiting kidney Qi,clearing the meridians,expelling rheumatism,relieving pain,astringing the essence,clearing the aperture,relieving the liver and Qi,and clearing heat and resolving phlegm.The combination of the three points has the effect of regulating the meridians and nourishing blood,and relieving the liver and nourishing the kidneys.According to modern research,stimulation of the above three auricular points can adjust the hypothalamic-pituitary-ovarian self-function,restore the normal physiological state of reproductive endocrine,activating the brain's dopamine system,enabling the ovarian self-function, restoring reproductive endocrine function,and thereby achieving a physiologically dynamic balance[13].
According to the pharmacological research,the combination ofFujing prescription and auricular acupoint can adjust the hypothalamic-pituitary-ovarian axis,activate the original ovarian follicle,facilitate uterine development,improve follicle quality,make follicle development more mature.
During this study,the effective rate was 76% and 84%,respectively in the control group and the treatment group;After treatment,the TCM score was significantly lower, a significant decreases in follicle-stimulating hormone and luteinizing hormone,and a significant increase in estradiol levels were proved.The indexes of IgG,IgM and IgA are higher in the treatment group with a lower adverse reactions rate[14].The analysis shows that the homemade Fujing prescription and auricular acupoint application can significantly improve patients’clinicalsymptoms,reduce the level of follicle stimulating hormone and increase the level of oestrogen compared with the treatment with single western medicine femoston[15].
Conclusion
In conclusion,Fujing prescription combined with auricular acupoint application has obvious clinical therapeutic effects and high treatment efficiency in the treatment of patients with POF,leading to the improvement of hormone levels and clinical symptoms.It deserves further promotion and application in clinical practice.