Visual quality after implantation of trifocal intraocular lenses in highly myopic eyes with different axial lengths
Hui Liu, Fang-Fang Li, Hai-Jun Xia, Jin Zhou,3
1Department of Ophthalmology, Chengdu Aier Eye Hospital, Chengdu 610041, Sichuan Province, China
2Department of Ophthalmology, Chongqing Aier Eye Hospital, Chongqing 400020, China
3Department of Ophthalmology, Aier School of Ophthalmology, Central South University, Changsha 410012, Hunan Province, China
Abstract
INTRODUCTION
High myopia is considered as the risk factor for cataract formation, which is evident in that cataract develops at a relatively younger age in highly myopic individuals[1-3]. For these patients, implantation of multifocal intraocular lenses (IOLs) is expected to relieve them from using spectacles or contact lenses with satisfactory visual outcomes. Previous studies have shown that implantation of bifocal IOLs is a practical option that can be used to achieve good uncorrected distance and near visual acuity in eyes with long axial lengths (ALs)[4-5]. Moreover, satisfactory visual performances at different distances have been shown after trifocal IOL implantation in highly myopic eyes, even with low IOL powers[6]. However, when multifocal IOLs are implanted in patients’ eyes, they may report several types of adverse visual effect, including decreased contrast sensitivity and the perception of glare or halos[7-9]. Thus, it is worthwhile to evaluate the in vivo optical and visual outcomes of highly myopic eyes implanted with multifocal IOLs.
Recent developments in optical quality evaluation have come into clinical use. One example uses the double-pass method, through which the ocular media and retinal reflections provide complete information and accurate estimates of optical quality[10]. The Optical Quality Analysis System (OQAS), based on this double-pass technique, assesses and quantifies all higher-order aberrations (HOA) and intraocular forward and backward scattering as a reliable predictor for retinal image quality after IOLs implantation[11-12]. This system has been successfully applied to measure the optical quality of different types of multifocal IOLs, such as diffractive bifocal IOLs[13], hybrid apodized diffractive-refractive optic zone multifocal IOLs, and refractive rotationally asymmetric multifocal IOLs[14-16].
However, none of the previous studies mentioned the objective optical quality of trifocal IOLs in highly myopic eyes. It is important to provide this information, which will help clinicians to recommend appropriate multifocal IOLs for patients with high myopia. In this study, besides subjective evaluation, the double-pass instrument was used to evaluate objective visual quality after performing trifocal IOL implantation in highly myopic eyes with different ALs.
SUBJECTS AND METHODS
Ethical ApprovalThe study was approved as a retrospective study by the Ethics Committee of Chengdu Aier Eye Hospital. The research adhered to the tenets of the Declaration of Helsinki. All patients were adequately informed about the study and signed the consent form.
SubjectsForty-four patients (13 males, 31 females) aged 40 or above who underwent cataract surgery or refractive lens exchange with the implantation of a trifocal IOL (AT LISA tri 839MP, Carl Zeiss Meditec AG) at Chengdu Aier Eye Hospital from June 2018 to January 2019 were included. Eyes with substantial preoperative corneal astigmatism of more than 1.0 D corrected with LenSx femtosecond laser (Alcon, TX, USA) were also included in this study. The exclusion criteria were previous ocular surgeries except for cataract surgery or refractive lens exchange, corneal abnormalities, ocular pathologies, and incomplete follow-up data.
We classified the patients into three groups depending on their ALs: patients with AL<26 mm; patients with AL≥26 mm and <28 mm; and patients with AL≥28 mm. ALs of the highly myopic eye (AL≥28 mm) are defined as extreme myopia[17].
Surgical TechniqueThe same experienced surgeon (Zhou J) performed all surgeries. In each patient, the cataract was removed by phacoemulsification and aspiration with a 2.4 mm temporal corneal incision or superior sclerocorneal incision. The trifocal IOLs were implanted in the capsular bag with an injector. For patients with preoperative corneal astigmatism of more than 1.0 D, arcuate corneal incisions were planned with the Version Image Guided System (Alcon, TX, USA) and were applied with the LenSx femtosecond laser system.
AL, anterior chamber depth (ACD), and corneal curvature were measured by using partial coherence interferometry measurements (20 eyes; IOLMaster 500, Carl Zeiss Meditec AG) or swept-source coherence tomography (SS-OCT; 41 eyes; IOLMaster 700, Carl Zeiss Meditec AG). The IOLs power was calculated with the Barrett Universal Ⅱ and Haigis formulas using the User Group for Laser Interference (ULIB) constants. We selected the IOLs power of each patient with the aim of obtaining a postoperative refraction of 0 D.
Outcome EvaluationAnalysis of visual outcomes at three months postoperatively was performed using the following measures: monocular uncorrected distance visual acuity (UDVA) and corrected distance visual acuity (CDVA) at 4 m, uncorrected intermediate visual acuity (UIVA) and distance corrected intermediate visual acuity (DCIVA) at 80 cm, and uncorrected near visual acuity (UNVA) and distance-corrected near visual acuity (DCNVA) at 40 cm. All the visual acuities were tested with the Early Treatment Diabetic Retinopathy Study chart under photopic lighting conditions (167 cd/m2). The results were reported as logarithm of the minimum angle of resolution (logMAR) values. Defocus curve testing was performed using the distance logMAR chart under an 85 cd/m2lighting condition. After distance correction, lenses from -4.0 D to +3.0 D were placed in 0.5 D steps in front of each eye, then the visual acuity was measured.
OQAS Ⅱ (Visiometrics SL, Terrassa, Spain) was used to evaluate optical quality with a 4.0 mm artificial pupil. The parameters included point spread function (PSF), objective scatter index (OSI), modulation transfer function (MTF) cutoff, Strehl ratio (SR), and OQAS values (OVs) at three contrast levels (100%, 20%, and 9%). OSI is provided as an index to quantify intraocular scatter, defined as the ratio of the light outside the double-pass retinal image to the amount of light of the central zone. MTF cut-off refers to the frequency at which MTF value is 0.01, and SR is the measure of the fractional drop in the peak of the PSF. Each OV is calculated as its corresponding MTF frequency segmented by 30 cpd.
Statistical AnalysisAll data were analyzed using SPSS software for Windows version 23.0 (SPSS Inc., Chicago, IL, USA). The analyses were based on a non-normal distribution of the data. The Kruskal-Wallis test was used to compare data from the three groups. The results of two groups were compared using the Mann-Whitney U test. The sex distribution, rate of femtosecond laser use, and postoperative spherical equivalents were compared using the Chi-squared test. Spearman correlation analysis was used to assess the correlation between variables. A P value <0.05 was considered statistically significant.
RESULTS
Our study included 61 eyes of 44 patients, with 15 patients (21 eyes, 66.67% female) in the AL<26 mm group, 13 patients (19 eyes, 69.23% female) in the AL≥26 mm and <28 mm group, and 16 patients (21 eyes, 75% female) in the AL≥28 mm group. The proportion of eyes that were treated with femtosecond laser-assisted cataract surgery was 52.38% (11/21 eyes) in theAL<26 mm group, 52.63% (10/19 eyes) in the AL≥26 mm and <28 mm group, and 42.85% (9/21 eyes) in the AL≥28 mm group. No significant difference was noted among the three groups (χ2=0.513, P=0.774). Table 1 summarizes the demographic and preoperative clinical characteristics of the three groups. Preoperative spherical equivalent (SE) became lower with increasing AL. Like the trend for SEs, IOL power decreased with increasing AL as well. However, corneal astigmatism and the flattest meridian (K1) differed significantly only between the AL<26 mm group and the AL≥28 mm group. ACD and the steepest meridian (K2) did not differ significantly among the three groups.

Table 1 Demographic and preoperative characteristics of the patients mean±SD (range)

Table 2 Postoperative visual and refractive results mean±SD (range)
Visual AcuityTable 2 shows the visual and refractive outcomes of the patients three months after IOL implantation. There were no significant differences between the mean UDVA, UIVA, UNVA, CDVA, DCIVA, and DCNVA values of the three groups (P>0.05). Additionally, no differences were found between the SE and refractive astigmatism values of the three groups (P>0.05). Corneal astigmatism decreased in all groups after surgery. However, there was no difference in corneal astigmatism values of all groups (P>0.05). The proportion of eyes with a postoperative SE between +0.50 D and -0.50 D was 95.24% (20/21 eyes) in the AL<26 mm group, 84.21% (16/19 eyes) in the AL≥26 mm and <28 mm group, and 85.71% (18/21 eyes) in AL≥28 mm group. No significant difference was noted in this proportion between the three groups (χ2=1.443, P=0.486).
Defocus CurvesFigure 1 shows the monocular throughfocus best corrected visual acuity after three months. The maximum visual acuity value was obtained at a defocus of 0 D which corresponds to the far focus. For high defocus values (positive or negative), the visual acuity decreased as expected. Comparison of the three groups showed statistically significant differences for all vergences except for -1.0 D, -0.5 D and 0 D (P=0.295, P=0.632, and P=0.152, respectively). The intermediate vision values ranging from -2.0 to -1.5 D were significantly different between the three groups, which were better in the AL<26 mm group (AL<26 mm group vs AL≥28 mm group, P=0.002 and P=0.006, respectively). The curve for the AL<26 mm group also showed better near visual acuity from-3.0 D to -2.5 D (AL<26 mm group vs AL≥28 mm group, P=0.000 and P=0.000, respectively).
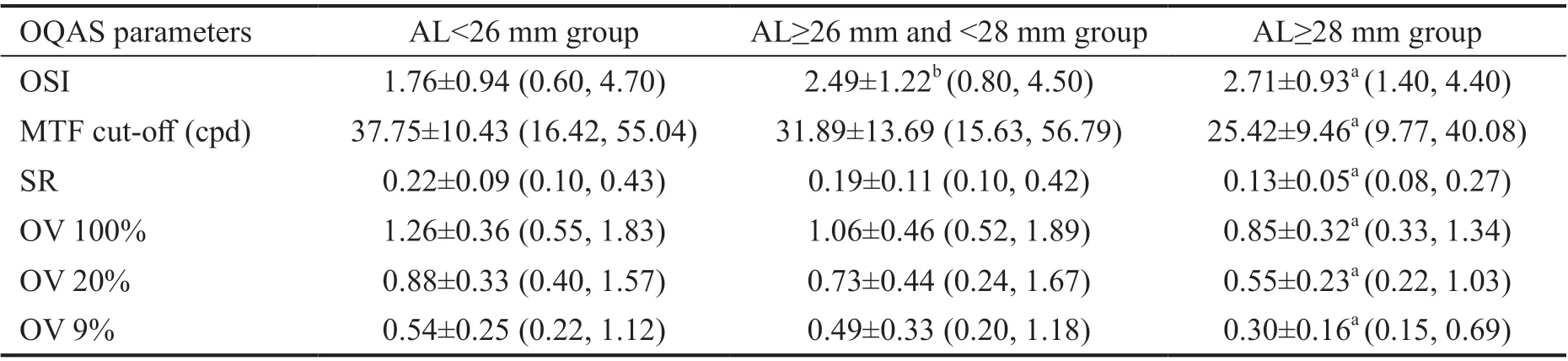
Table 3 Optical quality parameters after implantation of trifocal IOLs mean±SD (range)
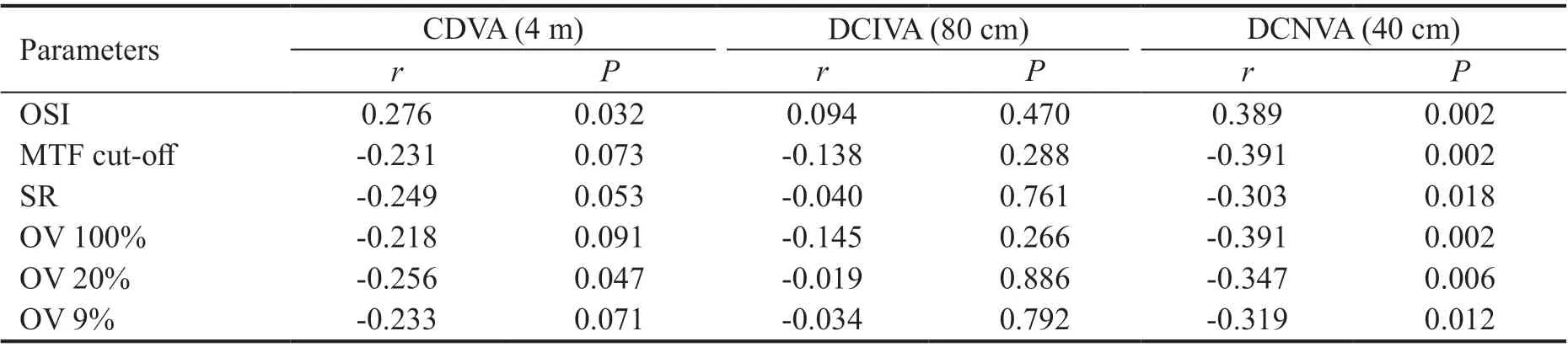
Table 4 Correlation between OQAS parameters and subjective corrected visual acuities
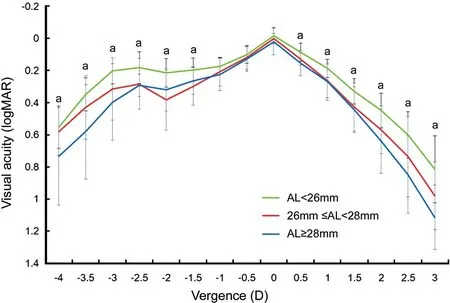
Figure 1 Three-month postoperative monocular defocus curves with correction for distance aP<0.01 compared between AL<26 mm group and AL≥28 mm group.
Objective Optical QualityA comparison of the postoperative OQAS parameters in the three groups is presented in Table 3. The mean MTF cut-off frequency (P=0.111), SR (P=0.226), OV 100% (P=0.111), OV 20% (P=0.065) or the OV 9% (P=0.255) of the AL<26 mm group and the AL≥26 mm and <28 mm group were similar, with no significant differences between groups. However, significant differences were only observed between the OSI values (P=0.044) of these two groups. As shown in Table 3, there were statistically significant differences in the OSI values, MTF cut-off frequency, and the SR between the AL<26 mm group and the AL≥28 mm group (P=0.001, P=0.001, and P=0.000, respectively). The mean OSI was higher in the AL≥28 mm group, whereas the MTF cut-off and SR values was lower in the AL≥28 mm group. Compared with the AL<26 mm group, the OVs (100%, 20%, and 9%) were significantly lower in the AL≥28 mm group (P=0.001, P=0.001, and P=0.000, respectively).
Correlation Between OQAS Parameters and Corrected Visual AcuitiesThe correlation between all OQAS parameters and DCNVA was statistically significant. Besides, statistically significant correlation was also found between OSI, OV 20%, and subjective CDVA. None of the OQAS parameters were correlated with DCIVA (Table 4).
At near distance with -2.5 D (40 cm) defocus, there was a statistically significant correlation between all OQAS parameters and corrected visual acuity. Significant correlation was also observed between OSI, MTF cut-off, OV 100%, OV 20% and corrected visual acuity at 0 D (4 m) and -1.5 D (67 cm; Table 5).
DISCUSSION
In the present study, we compared the visual quality of highly myopic eyes grouped by ALs after implantation of trifocal IOLs. Although there have been studies on the objective and subjective visual quality of trifocal IOLs[18], until now, there is no available research on the optical quality of trifocal IOLs in highly myopic eyes, especially compared the postoperative optical quality using double-pass instrument between different ALs. We found that extremely myopic eyes after the implantation of trifocal IOLs showed lower objective optical quality with more intraocular light scatter.Clinical evaluations have shown that trifocal IOLs provide excellent distance, intermediate, and near acuities after surgery[19-20]. Although both bifocal and trifocal IOLs had good distance visual performance, trifocal IOLs (including the AT LISA tri 839MP trifocal), had a distinct advantage for intermediate vision. Besides, visual acuity at near distance was not impaired by trifocal IOLs and even could be improved by the AT LISA tri 839MP IOLs[21]. The results of previous studies that involved the evaluation of trifocal IOLs in highly myopic eyes showed that UDVA, UIVA, and CDVA values of eyes implanted with IOLs powers greater than or equal to 10.0 D were better than those obtained from eyes implanted with IOLs powers less than 10.0 D[5]. In the present study, we grouped high myopia patients depending on their ALs according to Ogawa et al’s[4]and Rong et al’s[17]methods. In Table 1, IOL powers of the patients in the AL<26 mm group were all above 10 D, whereas the IOL powers of the patients in the AL≥28 mm group were all below 10 D. There was an overlap of IOL power (below or above 10 D) in the AL≥26 mm and<28 mm group. Thus, the method of classifying highly myopic eyes by AL in the current study seems more practical and reasonable.Previous study of the bifocal IOLs divided their patients into two groups (AL≥26 mm group and AL<26.0 mm group) and found good uncorrected and corrected distance and near visual acuities, without differences between the two groups[4]. In the present study, we also found no significant differences in uncorrected and corrected visual performance at all distances between the three groups. Our observation of no difference in UDVA and CDVA may be explained by the absence of any significant difference in the mean SEs of the three groups (P=0.406; Table 2). Furthermore, over 80% of the eyes in all groups in the present study had postoperative SEs ranging from +0.50 to -0.50 D, with no significant differences between the three groups. However, in the previous study, the percentage of SEs between +0.50 to -0.50 D was 72% in the IOL power≤10 D group[6]. This may be due to the biometric measurement used in the study and the choice of appropriate formulas.

Table 5 Correlation between OQAS parameters and corrected visual acuities on defocus curve
Accurate calculation of IOLs power is always challenging in cases of high myopia[22-23]. AL measurements were performed by optical biometry for all eyes. IOLs power was calculated by using the Haigis and Barrett Universal Ⅱ formulas with the ULIB constant. Rong et al[17]suggested that both formulas seem to be most accurate for eyes with AL>28.0 mm and <30.0 mm, whereas the Barrett Universal Ⅱ formula is better than the Haigis formula for eyes with AL≥30.0 mm[17]. We used the IOLMaster 700 for the preoperative biometric measurement of about two-thirds (41/61) of the eyes in the present study. IOLMaster 700 is a SS-OCT-based biometric equipment for measuring AL and calculating IOL power. This new biometer can detect the tomographic visualization of the complete longitudinal section of the eyeball, which includes the fovea[24]. Thus, the accuracy of IOL power prediction was improved in this study.
The optical design of the AT Lisa tri 839MP allocates 50.0% of light to distance, 20.0% to intermediate, and 30.0% to near[18]. As a result of this distance-dominant design, we found distance visual acuity was better than near visual acuity, which is consistent with those of several previous studies on trifocal IOLs[6,20,25]. Previous studies have also shown that trifocal IOLs are not dependent on pupil diameters up to 4.5 mm, and they provide adequate visual performance under all lighting conditions[18]. In our study, UDVA, UIVA, UNVA, CDVA, DCIVA, and DCNVA were measured with an illumination of 167 cd/m2, whereas the defocus curves were obtained under a lower lighting condition (85 cd/m2). Although there was no significant difference between the DCIVA and DCNVA of the three groups, the defocus curve showed that visual acuity was better in the AL<26 mm group from -3.0 D to -1.5 D. However, no significant difference was found when CDVA or visual acuity at 0 D on the defocus curve were compared between the three groups. These results indicate that lighting condition may influence intermediate and near visual performance in highly myopic eyes.
In postoperative cataract patients, internal aberration arises mainly from intraocular structures. The structures of the eyeball and the type of implanted IOLs are the impact factor of internal HOA in pseudophakic eyes[26]. In our study, there was no significant difference between the mean ACDs of the three groups. However, in cases when AL increases over the point of 26.7 mm, the axial elongation can aggravate the pathological myopia in the posterior part of the eyeball[27]. Although some of the cataract surgeries in this study were assisted by the femtosecond laser, the proportion of eyes that underwent femtosecond laser-assisted cataract surgery showed no statistically significant difference between the three groups. Thus, the effect of the femtosecond laser on the optical quality in the three groups should not be considered. Given the main morphological characteristics of highly myopic eyes, the effect of posterior staphyloma on internal HOA must be considered.SR is an useful parameter of optical quality, which is closely associated with aberrations[28]. Zhu et al[26]found that SR was lower in highly myopic eyes than in eyes with normal ALs with a 4 mm pupil size. With a 4 mm pupil, corneal aberration would not affect the results much, which may be closer to the real optical quality of the IOLs[13]. Notably, the AT LISA tri 839MP IOLs is trifocal with an IOLs diameter of 4.34 mm and bifocal between 4.34 and 6 mm[29]; thus, we also chose to measure its optical quality using a 4.0 mm pupil diameter. Moreover, it is noteworthy that OQAS is one of the few system that provides objective assessment of optical quality as it analyzes not only aberration, but also scatter and diffraction in human eyes[30]. However, none of the previous studies compared the optical quality in the highly myopic eyes with different ALs by using this double-pass technique. In the present study, we found that SR decreased with increasing AL, and was significantly lower when AL≥28 mm and is consistent with the results from previous studies. Besides SR, we also compared other objective optical parameters of the AL<26 mm group with those of the AL≥28 mm group, and found significant differences in the mean OSI, MTF cut-off frequency, the three OVs of the two groups, indicating that implantation of trifocal IOLs results in lower objective optical quality when the AL is greater than or equal to 28 mm due to the presence of more intraocular light scatter in such cases.
Correlation analysis demonstrated that a significant correlation existed between all OQAS parameters and DCNVA or visual acuity at the vergence of -2.5 D, indicating that objective visual quality has an impact on near visual quality in highly myopic eyes after implantation of trifocal IOLs. Besides, there was a significant correlation between OSI and CDVA or vergence at 0 D, suggesting that OSI may also be a reliable objective index of distance vision in trifocal IOLs. This result is consistent with that of a previous study on bifocal IOLs, which suggested that the implantation of multifocal IOL caused more intraocular scatter light[13].
A major limitation of this study is its retrospective design. Another limitation is that the eyes with corneal astigmatism of more than 1.0 D before surgery were corrected using the femtosecond laser with lower predictability and precision compared with toric IOLs. Larger sample sizes and longer follow-up periods are necessary to confirm the results in further studies.
In summary, this study demonstrated that implantation of trifocal IOLs provides satisfactory short-term visual and refractive results in highly myopic eyes with different ALs. However, when the AL of the eye was greater than or equal to 28 mm, objective optical quality decreased significantly with poorer intermediate and near visual performance in lower lighting condition. While for optical quality parameters of OQAS, all of them had significant correlation with near vision in highly myopic eyes. These results suggested that the decreased near vision of the extremely myopic eyes in the lower lighting condition was associated with the decrease of the objective visual quality in these highly myopic eyes.
ACKNOWLEDGEMENTS
Conflicts of Interest: Liu H,None;Li FF,None;Xia HJ,None;Zhou J,None.
 International Journal of Ophthalmology2021年3期
International Journal of Ophthalmology2021年3期
- International Journal of Ophthalmology的其它文章
- Corneal stromal mesenchymal stem cells: reconstructing a bioactive cornea and repairing the corneal limbus and stromal microenvironment
- Real-world outcomes of two-year Conbercept therapy for diabetic macular edema
- Role of home monitoring with iCare ONE rebound tonometer in glaucoma patients management
- Comparing posture induced intraocular pressure variations in normal subjects and glaucoma patients
- High interpretable machine learning classifier for early glaucoma diagnosis
- Micropulse laser trabeculoplasty under maximal tolerable glaucoma eyedrops: treatment effectiveness and impact of surgical expertise
