Nursing care of vascular crisis in a child with neck skin contracture and skin flap transplantation after burn: A case report
Yuexin Shi, Fengyi Jiang, Jiamei Yuan, Xiaorong Ma, Kaiyang Lv
Department of Plastic Surgery, Xinhua Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai 200092, China
Keywords:Fasciocutaneous flap transplantation Facial scars Vascular crisis Pediatric nursing
ABSTRACT In this report, we aimed to summarize the nursing points of fasciocutaneous flap transplantation due to scar contracture caused by a large area of head and face scald.A 4-year-old girl suffered from wound bleeding, respiratory tract edema, and vascular crisis and was transferred to the intensive care unit after flap transplantation.The child’s scar recovered well before she was discharged, and the follow-up results were satisfactory.After recovery, she had fewer complications under careful and scientific nursing care.The nursing points were to provide a stable treatment environment through regular wound observation and strict aseptic operation; ensure the nutrition of the child; give the child personalized sedative and analgesic care; and perform anticoagulation,antispasm, and dressing change and provide warmth for vascular crisis.Dressing changes by plastic surgery specialists combined with sedation and analgesia can alleviate children’s pain, enable them to better cooperate with surgical site observation and dressing care,increase the survival rate of the skin in the surgical area,and help improve the prognosis of the child.
1.Introduction
Accidental injuries in children are common.The facial and neck scar contracture deformity caused by burns and scalds does not only affect the patient’s appearance and psychological state but also affect their corresponding physiological functions.Soft tissue deformity also has a severe impact on the growth and development of the patient.1Facial wound repair is a scientific process, and the visual aesthetics after repair needs to be considered comprehensively.The local skin flap has its blood supply,and its rich vascular network on the face provides the basis for anti-infection and tissue regeneration inthe defect area.Therefore,survival and recovery rates of the skin flap after transplantation are high, and the incidence of complications is low.2Vascular crises,one of the complications after skin flap transplantation,mainly occurs 6–72 h after the operation.Therefore,timely observation,detection,and treatment after the operation are crucial,which lead to higher requirements for nursing work.3
2.Case presentation
In January 2021,the Plastic Surgery Department of Xinhua Hospital affiliated to Shanghai Jiao Tong University School of Medicine admitted a disfigured patient with facial and neck scar contracture due to lower eyelid ectropion, upper lip missing, and lower lip ectropion caused by burns(Fig.1).
The patient was a 4-year-old female,weighing 19.5 kg.The neck scar deformity was present for more than a year and nearly half a year after the implantation of the dilator.Physical examination conducted on admission recorded the following findings: body temperature, 37.3°C;pulse, 114 beats/min; breathing, 25 beats/min; clear mind and normal response.Based on the age characteristic of the child, the QUESTT approach (Question the child and parent/caregiver; Use pain rating scales; Evaluate behavior and physiological changes; Secure parent or caregiver’s involvement; Take the cause of the pain into account; Take action and evaluate the results),facial expression scale,color scale,and behavioral scoring methods were selected for comprehensively evaluation of the child’s condition.The pain score was 2 points.Examinations showed that the child’s face,neck,chest,and back had large scars;local hyperplasia; and contractures; double lower eyelids were stretched and everted; scars in the mouth corner were stretched, thereby affecting mouth opening;and neck scar contractures affected receding of the neck.After the implantation of the back dilator, the skin shape was normal,without obvious ulceration or infection.Neck scar deformity correction+back dilator removal+fascia skin flap transplantation+pedicle skin flap transplantation was performed at the scheduled time.After the operation, the patient suffered wound bleeding, venous vascular crisis,and laryngeal edema and was transferred to the pediatric intensive care unit(PICU)immediately.

Fig.1. Preoperative photo of the patient.
Hu et al.4pointed out that enoxaparin sodium (Kesai) is a kind of low-molecular-weight heparin (LMWH), and LMWH has become the most widely indicated anticoagulant drug in arterial and venous thrombotic diseases.Thrombotic diseases involve various disciplines,and most thrombotic diseases have hidden onset.Once the disease onset occurs,the clinical concept of “prevention” should be established.Massicotte et al.5studied the safety and efficacy of LMWH and unfractionated heparin (UFH) in children and teenagers with venous thrombosis and showed that LMWH is a superior treatment.In the prevention of deep vein thrombosis in orthopedics and recurrence during treatment,LMWH is better than UFH.Thus, enoxaparin sodium of 1 900 IU under subcutaneous injection was administered at 9:00 a.m.and 21:00 p.m.on January 8 to 11 and January 14 to 15, 2021.Preparing the enoxaparin sodium injection was a challenge to doctors and nurses.Firstly, doctors correctly calculated the drug dosage according to the weight of the child(4 000 AXalu/0.4 mL),that is,1 900 IU/0.19 mL;discharged the excess liquid before injection; and then administered sedative drugs 30 mins before injection.Secondly,nurses carefully made subcutaneous injection of 0.1 mL each.Small-dose divided injection was administered 12 hours apart.During the injection, bleeding at the needle puncture site was observed, and a small amount of bright red bleeding points was indicative of successful injection.After the injection, the injection site and surrounding skin tissues were strengthened.The skin and mucous membrane tissues should be rosy,with a bit of bright red bleeding as the ideal state.If the skin color is dim,the blood vessels are not well filled,and the surrounding skin temperature drops,then there is a possibility of skin necrosis and skin vasculitis.It was different other injections after which we cannot press after the injection.Every movement must be gentle.Lastly, more focus should be paid on the occurrence of complications such as bleeding after drug use because enoxaparin sodium is used for acupuncture treatment to prevent microvascular thrombosis in the skin flap transplantation area;therefore,the most common complication of the drug is bleeding.The patient’s platelet count before drug administration was 356.00×109/L(normal value:100–300×109/L),and the platelet count was checked every 1–2 days during the use and maintained in the range of 233–414×109/L during the 10 consecutive tests.If the child’s platelet count is found to be significantly reduced to 30%–50%of the initial value, enoxaparin sodium therapy must be discontinued to prevent and treat heparin-induced thrombocytopenia-related thrombotic complications.During the period,other biochemical indicators such as the hemoglobin index of the child were monitored at 62–99 g/L(normal value:110–160 g/L)to understand the child’s blood loss status.
During medication, if there is any bleeding-prone situation in oral care, urine inspection should be performed for red blood cells, the skin and mucous membranes of the whole body should be assessed for bleeding points under natural light, and intravenous fluids should be removed.Any delay in the bleeding time during the pipeline and possibility of bleeding can be detected in time.
After active treatment with special surgical care, the patient recovered and was discharged on the 17th day after surgery.The nursing experience of the patient during hospitalization is summarized in Figs.2 and 3,which show the treatment progress.

Fig.2. The process of skin removal and flap transplantation during the operation of the child.(A)The pre-expanded flap.(B)The contracture completely separated the scar in front of the neck.(C) The flap covered the wound after complete release of the scar.
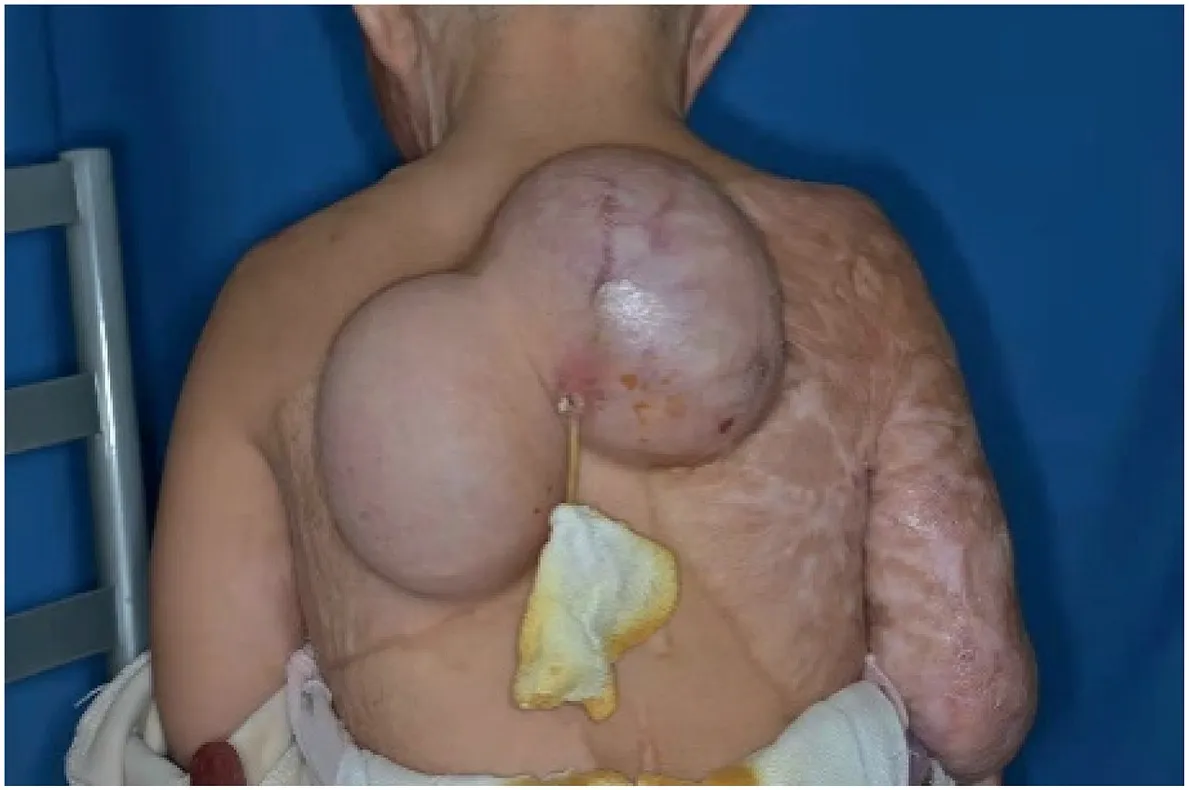
Fig.3. Three months after implantation of the dilator.
2.1.Psychological care
Rehabilitation and reconstruction after scalds require long-term treatment.The patient had a sense of fear in the hospital, which was manifested by crying on seeing the medical staff and not cooperating with various nurses and treatment.Moreover, children’s self-emotion regulation ability is not strong; therefore, most of them cannot selfregulate negative emotions.6Due to the novel coronavirus epidemic,our hospital strictly implemented the rule of “One patient, one escort”and stipulates that only the mother is allowed for company.However,considering that the child was prone to fierce resistance to treatment,after consulting the hospital infection experts,both parents were allowed to accompany the child after her tests yielded negative results.Nurses wore cartoon costumes to make the child comfortable, fully communicated with the parents before the operation, obtained parental understanding, and gave them enough time to calm the child’s emotions to facilitate cooperation with various treatments.After the operation, the nurses praised the child and encouraged her with cartoon stickers.
2.2.Postoperative care
2.2.1.Vascular crisis care
Vascular crisis, including arterial crises and venous crisis, typically occurs within 72 hours of surgery.The skin flap color is the most accessible and most reliable objective indicator for the observation and treatment of vascular crisis.The blood flow observation record of the flap designed by Wang Ru7can be used.The right half of the flap transplanted in the neck showed a blue-purple congestion appearance together with edema (Fig.4), suggesting venous reflux disorder and venous vascular crisis.The nursing staff immediately opened the wound, and gave the wound acupuncture and bleeding to reduce the pressure.They used self-adhesive soft silicone fringe foam dressing (Mepilex) to cover the wound and promote wound healing.The nursing staff closely monitored the child’s bleeding,skin temperature,and skin color changes during the operation.After dressing the wound and injecting anticoagulant drugs,the operation continued until January 18, 2021, and the appearance of purple congestion around the flap turned red.The blood supply of the flap was available for transplantation,and the skin temperature and skin color were normal (Figs.5–7).During the period, relevant biochemical specimens, such as coagulation routine, D-dimer, coagulation factor VIII-IX, anti-Xa factor, and standards for determination of activated coagulation time, were collected, and results were reported and drug dosage was adjusted in a timely manner.
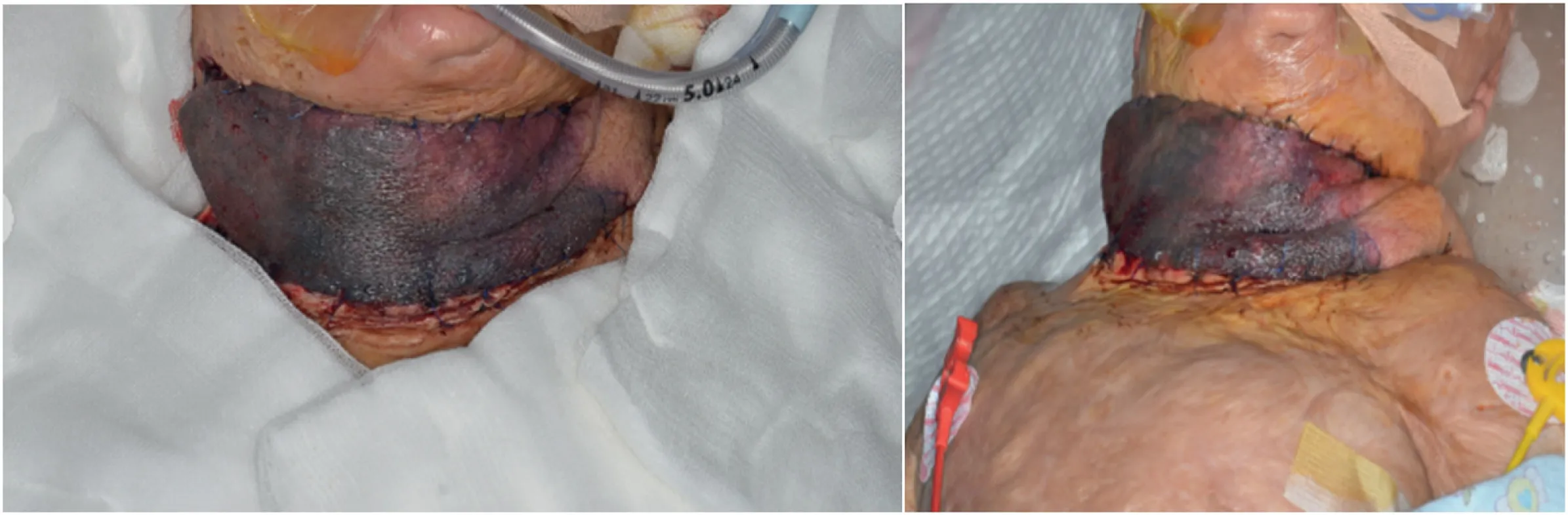
Fig.4. Purple hyperemia around the flap.The color of the skin flap on the first and second days after the operation was bluish purple or dark red,indicating that the venous return was blocked.

Fig.5. Seven days after the operation.Reduced swelling was observed.

Fig.6. After 10 days of continuous dressing change, the purple congestion around the skin flap turned red.The transplanted skin flap could supply blood.

Fig.7. Fourteen days after operation.The dermis of the flap graft area survived with a small amount of epidermal necrosis at the edge.
2.2.2.Sedative and analgesic care
After the child was transferred to the PICU,due to the lack of central suppression in children, the immune response was stronger and the patient was more sensitive to pain than adults.8The staff immediately provided analgesic treatment to the patient,until January 10.The child’s vital signs,such as mentality,pupils,blood pressure,and pulse,were all within a reasonable range during the observation process.At the same time, the Glasgow Coma Scale, PCIS Critical Case Scale, and PRISM Pediatric Death Risk Scale scores were also within the reference range.
2.2.3.Nebulized inhalation administration
During nebulization, the oxygen flow rate was typically set at 4–6 L/min,and the child’s blood oxygen saturation was observed at the same time.Aerosol was used to administer liquid medicine.The nursing staff exhaled slowly to prevent infection-related complications in the child.
2.2.4.Intradermal injection administration
In order to improve blood circulation in skin flaps, it is necessary to observe their survival.The area intracutaneously given with anticoagulant drugs was around the skin flap where the blood supply was poor Each 0.01–0.02 mL injection was administered at an angle of 0–5°.If the needle is inserted too deep,no medicine should be applied to the intradermal tissues and blood vessels.Nurses should not press the injection site in any way after the injection.It is essential to monitor the injection area for any swelling.Blood oozing from the needle eye indicates effective thrombolysis.The staff should wait for 10 min after the injection for the drug to be completely absorbed and subsequently place a sterile gauze to cover the wound.
2.2.5.Enteral nutrition support
Due to the high metabolic rate of children, higher nutritional requirements than adults,and an accelerated postoperative wound healing,children need high nutritional support.9Studies have shown that maintaining a semi-recumbent position is an effective measure to prevent aspiration pneumonia.Due to the immature development of the lower esophageal sphincter and poor control ability, gastroesophageal reflux occurs often.In addition, the skin removal area was on the back and the skin grafting area was on the face.The child was placed on his side and restricted to few activities and was thus prone to aspiration pneumonia.Therefore, on January 10, the child was given an indwelling gastric tube per the doctor’s advice;60 mL of 1:1 pediatric short peptide formula was given, and the gastric tube was injected q3h, during which the bed head height was adjusted to 20°–30°.Digestion was recorded to be good after liquid food administration,and no diarrhea or other discomfort occurred.The biochemical indicators were normal.After consultation with the Department of Pediatric Digestion and Nutrition on January 13, the plan was changed to 1:1 pediatric short peptide formula 120 mL q3h,injected into the stomach;on January 14,it was changed to 150 mL of 1:1 pediatric short peptide formula,injected into the stomach via a gastric tube q3h.
2.2.6.Oral feeding
Enteral nutrition was stopped until January 17, and the oral diet was gradually changed from liquid to semi-liquid to soft food.The nursing staff raised the head of the bed or the chest by 30°–45°to reduce acid reflux.The digestive function of children is characterized by better digestion of sugar, protein,10and glucose,as an essential carbohydrate, satisfying the metabolism of all cells in the human body.11Therefore, nurses gave 5%sugar water before feeding the child in order to increase the blood flow of the intestinal mucosa, reduce intestinal mucosal acidosis, and improve intestinal mucosal metabolism.12After eating,it is essential to observe and record whether the child has hiccups,abdominal distension,and abnormal stools.On January 18,the parents complained that the child had difficulty in defecation and was administered 1 g of bifidobacterium triple viable bacteria powder t.i.d to adjust the intestinal flora.
2.3.Discharge guidance
The child’s family members were instructed to carefully observe the condition of the child’s skin, adhere to the correct cleaning and moisturizing measures, and minimize skin dryness.Scar skin is drier than normal skin,has worse ductility,and is prone to dandruff.Guidance was provided on skin cleansing to the parents: the test water temperature should be kept at 37°C–39°C,the child’s skin should be soaked in warm water,and a warm wet towel should be applied to the face to expose the facial features; the caregiver should wear gloves and then gently scrub the patient’s skin with gauze to remove the skin from scar area that has been soaked and is thus soft.After bathing,a soft towel should be used to dry the patient’s body, and the patient should then be laid on the bed.Subsequently,the urea cream made by Xinhua Hospital should be applied to the scar, massaged for 5–10 min (2 times/day), paying attention to massage the skin with moderate intensity11and keep the child warm.The child’s bedding should be kept clean and flat,and the wound should be kept clean and dry to avoid wound infection.Moreover, the dressing should be changed regularly.It is also essential to guide the child’s parents to return for follow up on time(Fig.8).

Fig.8. The temperature and color of the skin flap grafted on the neck of the child was normal; the wound at the skin removal site was well healed.
3.Discussion
Children are susceptible to large-area burns.However, several difficulties arise once the child is admitted to a hospital.As these patients are young,they do not cooperate well.They are usually frightened and in a serious condition.A pre-expanded perforator flap is an effective treatment strategy for cervical scar contracture in children.The skin flap is fully expanded in advance, the skin at the dilator is fully cared for, and the skin is intact without damage and infection, which improves the survival rate of the skin flap after transplantation.After the child enters the PICU,adequate sedation and analgesia are administered and the dose of sedative and analgesic drugs is dynamically adjusted according to the child’s actual situation to reduce the possibility of vasospasm.This ensures better cooperation during the process of treatment and dressing.The nursing staff detected and correctly determined the occurrence of a vascular crisis after the operation in time, reported the same to the doctor, and administered active treatment.When dealing with hemostasis,anticoagulation,dressing changes,and other treatments,the same should be handled quickly, correctly, and promptly.Every movement should be gentle.All precautions need to be recorded so that the patient can be informed of the same after discharge.During the entire nursing process,the nursing team select the appropriate pain and self-care ability evaluation scale according to the child’s age and physiological characteristics.Based on the age characteristics of the child and the QUESTT approach, facial expression scale, color scale and behavioral scoring methods are selected to comprehensively evaluate the child.It is important to dynamically monitor the pain score of the child,administer corresponding nursing measures, and improve the comfort of the child:every detail counts to ensure successful treatment.
4.Conclusion
Perioperative nursing of flap operation and treatment and nursing of vascular crisis are keys to a successful flap operation.The treatment process involves almost all aspects of complex flap operation nursing.The case summary is as follows: sufficient hemostasis was administered to the child during the operation.Postoperative bleeding should be considered as a cause of the child’s awakening and restlessness during the transportation process, which may cause the wound to pull the skin flap, thereby increasing the blood pressure.Pain after being awake is related to vasospasm caused by anxiety, tension, and other emotions.If the child can be admitted into the ICU with a ventilator tube under continuous sedation for pain relief, it may reduce the risk of postoperative wound bleeding.During the operation,at least one set of arteries and veins should be added at the distal end of the skin flap so as to increase the perfusion pressure and reduce the probability of blood return problem.During the perioperative period, the nursing team should pay more attention to the psychological care of the children and their parents and provide full health guidance and disease communication to alleviate the anxiety of the children and their parents.
Ethics declarations
Ethics approval and consent to participate
The need for ethical approval was waived due to the retrospective nature of this case report.
Consent for publication
The participant gave written informed consent to publish the data contained within this study.Competing interests
The authors declare that they have no competing interests.
Authors’contributions
Shi Y:Study conception and design.Yuan J and Ma X:Investigation.Shi Y and Jiang F: Writing-original draft.Lv K: Writing-reviewing and editing.
Acknowledgments
This work was supported by the General Project of National Natural Science Foundation of China (grant no.81772091) and Three-Year Clinical Action Plan of Shanghai Shenkang Hospital Development Center (grant no.SHDC2020CR3039B).We would like to express our gratitude to Qin Gao and Kanjun Li from Xinhua Harvard CLIMB Initiatives for manuscript discussion and review.
 Chinese Journal of Plastic and Reconstructive Surgery2021年4期
Chinese Journal of Plastic and Reconstructive Surgery2021年4期
- Chinese Journal of Plastic and Reconstructive Surgery的其它文章
- Foreword from Professor Weiguo Hu
- Augmentation mammoplasty with autologous fat grafting
- Progress of laser and light treatments for lower eyelid rejuvenation
- Current state and exploration of fat grafting
- Application of digital technology in nasal reconstruction
- Micro-compound tissue grafting for repairing linear scars
