Cultural adaptation and content validity of a Chinese translation of the ‘Person- Centered Primary Care Measure’: findings from cognitive debriefing
Emily Tsui Yee Tse , Cindy Lo Kuen Lam, Carlos King Ho Wong ,,2 Weng Yee Chin, Rebecca S Etz, Stephen J Zyzanski, Kurt C Stange
ABSTRACT
Objectives To develop an equivalent Chinese translation of the Person- Centered Primary Care Measure (PCPCM) and to establish its cultural adaptability and content validity through cognitive debriefing.
Design The original English PCPCM was first translated into Chinese by double forward- translation by professional translators. The reconciliated Chinese version was then doubly back- translated into English by two other professional translators blinded to the forward- translation. On affirmation on its linguistic equivalence with the developers of the original English PCPCM, the reconciliated Chinese PCPCM was sent for cognitive debriefing with 20 Chinese- speaking primary care subjects by a trained interviewer using structured probing questions to collect their opinions on the clarity, comprehensibility and relevance of each item and response option in the Measure.
Setting Subjects were invited from a primary care clinic in Hong Kong to undergo the cognitive debriefing interviews. The interviews were divided into four groups chronologically to allow revision of the items to be made in between.
Participants Ten males and 10 females above the age of 18 completed the cognitive interviews. They were all Cantonese- speaking Chinese recruited by convenience sampling. Subjects with cognitive impairment, could not read Chinese, too old or too sick to complete the interviews were excluded from the study.
Results An average of 3.3 min (range 3—4 min) was required for the subjects to self- complete the Measure. All items were generally perceived to be easily understood and relevant. Modifications were made to items with the content validity index (CVI) on clarity or understanding <0.8 in each round of the interviews or if a majority of the subjects suggested rewording. Revisions were made to two items in the Chinese PCPCM throughout the whole cognitive debriefing process before the final version was confirmed. The average CVI on clarity of the Chinese PCPCM items ranged from 0.75 to 1. The average CVI on understanding ranged from 0.7 to 1. The average CVI on relevance ranged from 0.55 to 1.
Conclusions The content validity of the PCPCM was ascertained in terms of its clarity, understandability and relevance to allow further testing of its psychometric properties in a larger Chinese population.
INTRODUCTION
The Person— Centered Primary Care Measure (PCPCM) (online supplemental appendix 1) was developed in 2019 in the USA from extensive surveys that asked hundreds of patients, clinicians and payers what matters in (primary) healthcare. The findings were analysed and then refined at the Starfield Summit III with the aim to measure concisely the value of a primary care practice. The Measure had undergone three sets of psycho—metric analyses with its construct identi—fied, its reliability and concurrent validity confirmed.1It has been fielded with success in 35 Organisation for Economic Co— oper—ation and Development countries since its emergence.2It is a simple yet comprehensive measure featuring the important domains of primary care including accessibility, advocacy, community context, comprehensiveness, continuity, coordination, family context, goal— oriented care, health promotion, integration and relationship.1Each item is scored on a 4— point scale: definitely, mostly, somewhat and not at all. To fill out the questionnaire, information processing including interpre—tation of the questions and recalling of the clinic experience would be needed from the patients. They have to decide on their way of response and choose a response option which best fits them.3—5Subjects have to interpret the meaning of words or phrases in the questionnaire. Previous experience in the field revealed that translation itself (of questionnaires from a foreign language) may be a source of confusion for the respondents.56When response options do not correspond to the subjects’ situations, they may become confused and do not know which response option to choose.45Researchers need to look for the problems and correct them before the questionnaire can be formally administered in the general population.
In order for the PCPCM to be applicable to another culture, it has to be translated to the native language and confirmed to be valid in the target population. Ensuring the content validity in that target subjects’ interpretation of the questionnaire items being equivalent to what the original questionnaire developer intends to measure is a prerequisite for further psychometric testing. More—over, the response options of each item need to allow the subjects to respond in the way which best fits their opin—ions and situations.
The National Center for Health Statistics Question—naire Design Research Laboratory at the Centers for Disease Control and Prevention advises adopting cogni—tive debriefing to identify any problem or confusion in questionnaires.4In cognitive debriefing, interviewers apply one— on— one interviews to investigate the approach subjects employed to process the data when they answer the questions. Problems in item interpretation, deci—sion processes and response option selection can be recognised. Other problems, for instance, instructions, design and structure of the questionnaire, can also be identified through cognitive debriefing.45
This paper describes our first step to adapt the PCPCM for the evaluation of patient— centred care in primary care in Hong Kong where 95% of the population are Chinese. The aim of this study was to establish the cultural adapt—ability and content validity of a Chinese version of the PCPCM. The objectives were to develop an equivalent Chinese translation of the PCPCM and to evaluate the clarity, understanding and relevance of each item. This will in turn provide an equivalent Chinese PCPCM that is applicable to Chinese primary care patients for pilot psychometric testing. We believe, with a validated Measure, the performance of various primary care prac—tices in our community would be accurately reflected and could provide guidance for the government and consumers on health resources allocation.
METHODOLOGY
Development of the Chinese PCPCM and evaluation of content validity
The Chinese translation of the PCPCM was developed according to the International Society For Pharma—coeconomics and Outcome Research Principles of Good Practice: The Cross— Cultural Adaptation Process for Patient— Reported Outcomes Measures.7At the ‘Preparation’ stage, an Expert Review Panel consisting of six local primary care experts from the academic, profes—sional body, public and private clinical sectors were invited to assess the face validity of the original English PCPCM in the Hong Kong Chinese context. They unanimously agreed that the PCPCM was measuring the important aspects of primary care including ‘accessibility’, ‘compre—hensiveness’, ‘community— based’, ‘continuity of care’, ‘holistic care’, ‘coordinated care’, ‘evidence— based prac—tice’, ‘rapport building’, ‘patient advocate’, ‘preventive care’, ‘patient enablement’ and ‘patient— centred care’. They confirmed no amendment was needed for the PCPCM prior to translation.
Two professional translators who are native Chinese speakers, were employed to translate the original English version of the PCPCM into Chinese independently. Two bilingual investigators (ETYT and CLKL) reviewed the translations and formed the first draft of the Chinese PCPCM. Another two professional translators blinded to the original PCPCM were employed to back— translate the first draft to English. The back— translation was assessed and confirmed to be equivalent to the original measure by its developers (RE and KS). This first draft of the Chinese translation (online supplemental appendix 2) was sent for cognitive debriefing with 20 Chinese patients attending a public sector primary care clinic in Hong Kong to evaluate the clarity and interpretation of each item and response option.
Sampling of subjects
Subjects were recruited from a government— funded primary care clinic in Hong Kong where nearly all patients were Cantonese— speaking Chinese. Subject inclusion criteria were Cantonese— speaking adults (≥18 years old) without cognitive impairment and able to read Chinese. Exclusion criteria were subjects who were too old (whom may have difficulty in reading the questionnaire) or too sick to complete the interview. The sampling was purpo—sive to include subjects with a wide range of ages and education levels with an equal distribution of gender.
Procedures
The cognitive debriefing was conducted between July and August 2019. A trained research assistant carried out the cognitive debriefing using an interviewer guide with struc—tured probing questions (table 1). Subjects were encour—aged to give comments on any difficulty in completing the questionnaire and give recommendations to replace any unclear wording. All the debriefing interviews were conducted one— on— one in the primary care clinic. Written informed consent was obtained prior to each interview.
At the start, the interviewer explained the aim of the study and the procedures of the cognitive debriefing to the subject. The interview was audiotaped. Demographic data (table 2) of the subject were collected. The subject then completed the Chinese PCPCM by him/herself and the time of completion was recorded. The audiotaping and cognitive debriefing started afterwards. The subjectanswered four questions on their general impression on the questionnaire and then five probing questions for each item of the PCPCM. Each cognitive debriefing inter—view lasted 20—30 min. Each subject was given HKD100 (~US$13) supermarket voucher in appreciation of his/her contribution to the study.
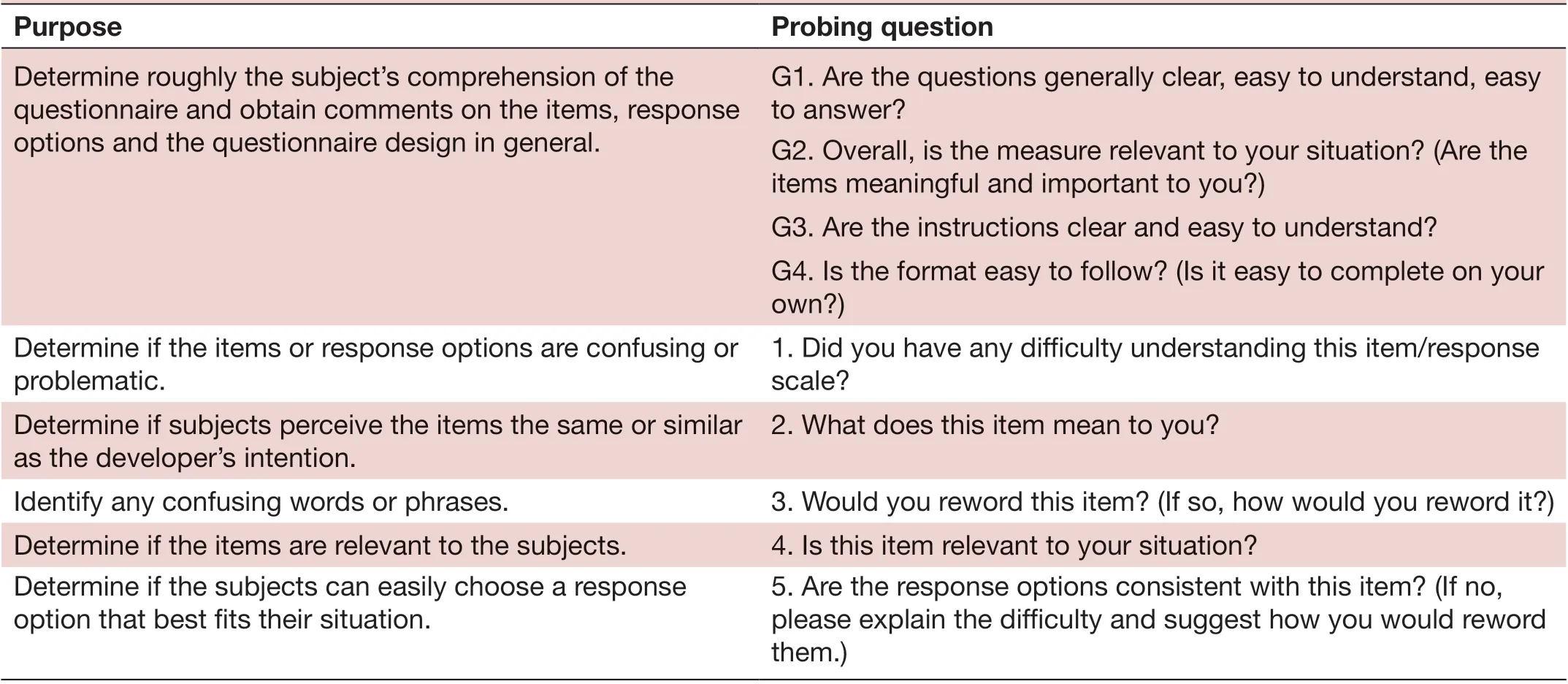
Table 1 Structured cognitive debriefing interviewer guide
The subjects’ answers to the interview were recorded and transcribed verbatim. Interview results were summarised in a tabular format. The transcript was reviewed by the investigators to identify any problem in the content of the draft Chinese PCPCM after the completion of eachround of interviews. When a problem was recognised, the investigators (ETYT and CLKL) deliberated on the problem item and revised the content accordingly, and further tested in the next group of subjects. The process continued until there was no more problem found in each item. The whole cognitive debriefing process was performed through 4 rounds of interviews with 20 different subjects. The first, second, third and fourth rounds consisted of nine, five, three and three subjects, respectively. The content validity index (CVI) was calcu—lated by the total number of positive ratings divided by the number of subjects in that round. Revisions were made to items with the CVI on clarity or understanding <0.8 after each round of interview or if a majority of the subjects suggested a rewording. The revised measure was subsequently tested with the next round of subjects until no more problem was identified (at the fourth round).
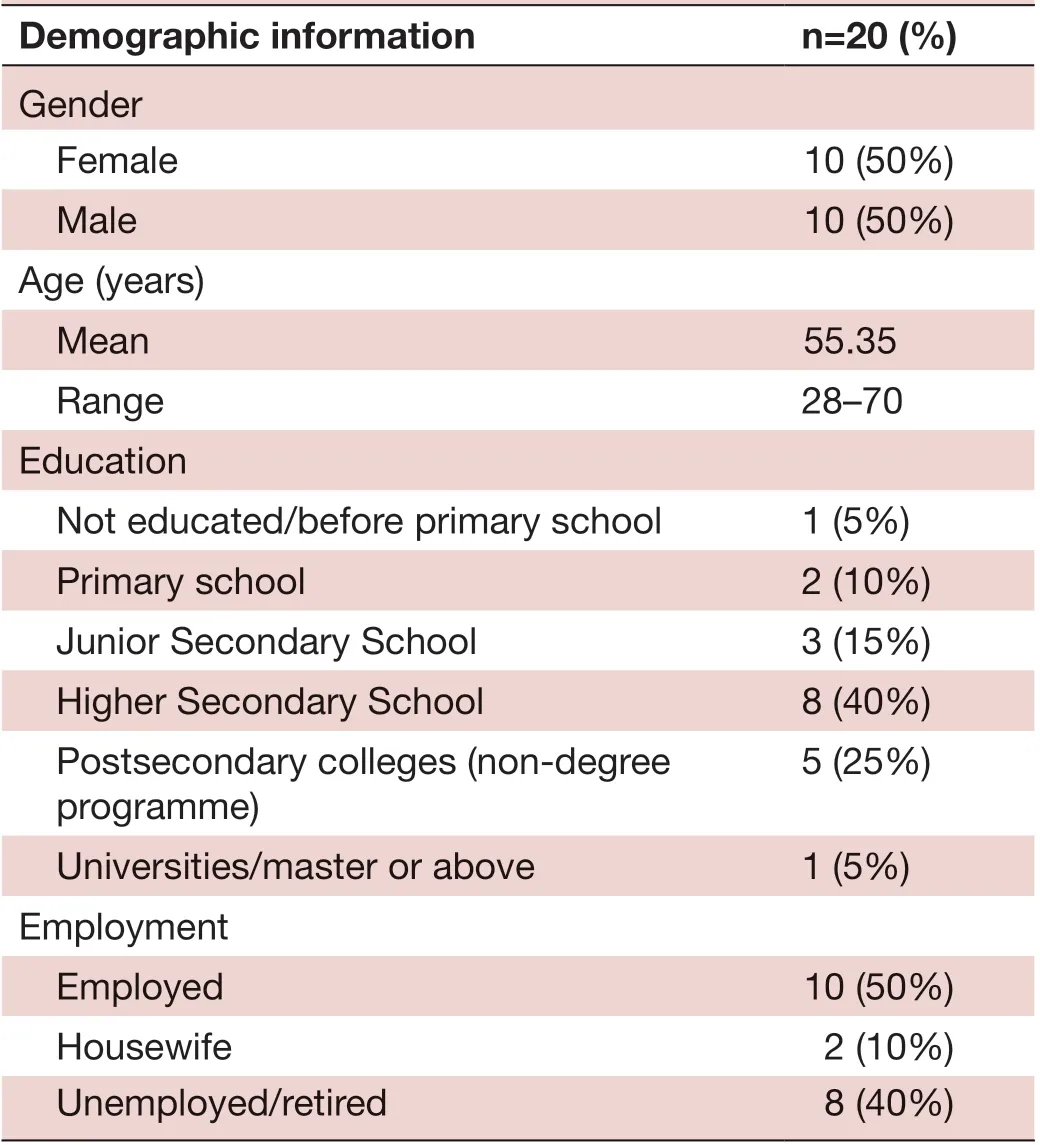
Table 2 Characteristics of cognitive debriefing subjects
RESULTS
The mean completion time of the Chinese PCPCM among the 20 subjects was 3.3 min (ranged from 3 to 4 min).
The 11 items related to person— centeredness together with the response scale, and an additional item asking for the duration of the subject having known the doctor (online supplemental appendix 2) underwent content validation. As mentioned in the methodology section, the whole cognitive debriefing process was performed through 4 rounds of interviews with 20 different subjects. Sixteen subjects (80%) commented the items in the Chinese PCPCM in general were clear, easy to understand and to answer (question G1 stated on table 1). All subjects confirmed relevance (question G2 stated on table 1) and clarity of the instructions (question G3 stated on table 1) of the Measure on the whole. One out of the 20 subjects commented on the format of the response scale (questionG4 stated on table 1): He found the distinction between ‘mostly’ and ‘somewhat’ to be unclear. He suggested that could be changed to a percentage scale to indicate the respondent’s degree of agreement with the item. Another subject (an elderly aged 68) expressed that it was a bit difficult to complete the Chinese PCPCM on his own.
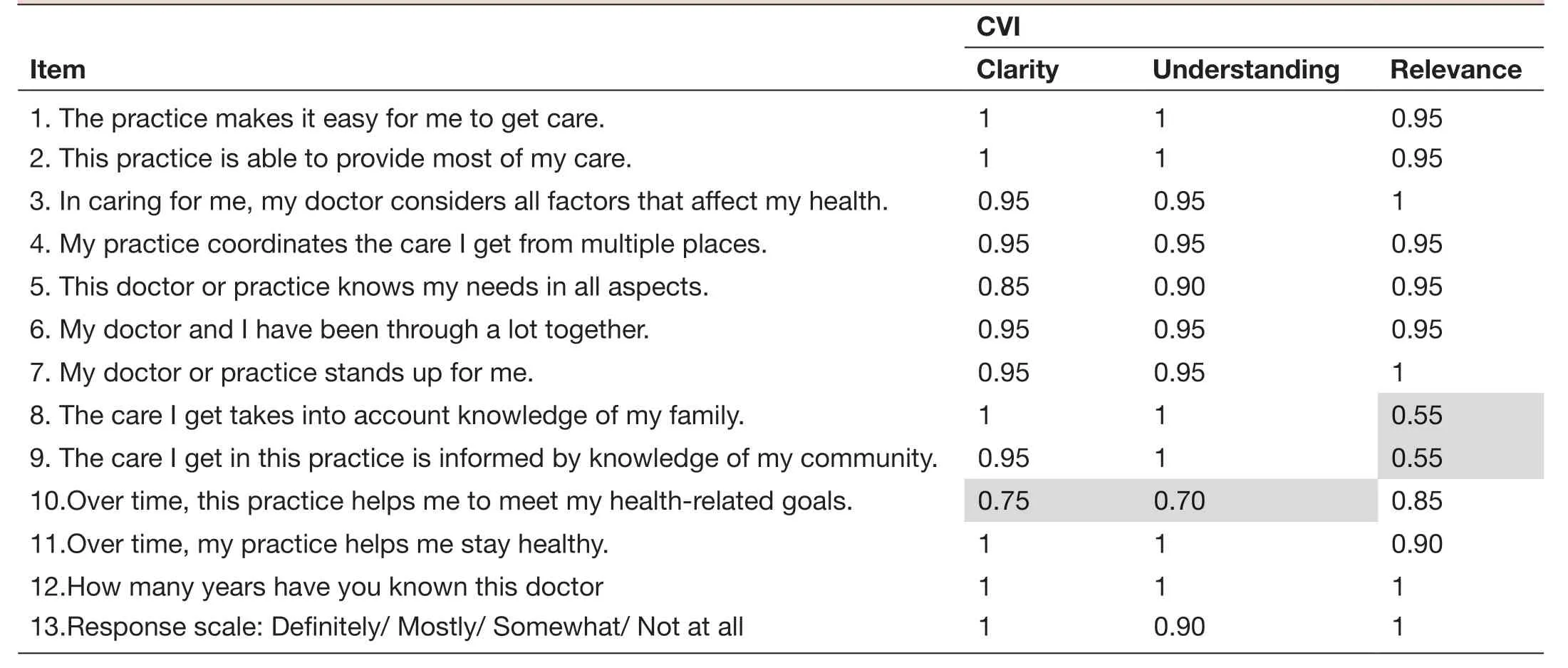
Table 3 Average CVI on clarity, understanding and relevance of each item in the PCPCM during the four rounds of cognitive debriefing interviews
After obtaining the subjects’ general impression on the Chinese PCPCM, they were asked to explain the meaning of each item and to suggest if any rewording needed to improve comprehension. The average CVIs on clarity, understanding and relevance of each item are shown in table 3. As revealed by the answers to the general probing questions, majority of patients actually found most of the question items to be clear, easy to understand, relevant to them and did not require rewording. The exception was for items 5, 8, 9 and 10.
For item five, the English version was ‘This doctor or practice knows me as a person.’ We translated that into ‘這位醫生或這間診所對我個人很了解’ initially. This translation literally means ‘This doctor or practice under—stands me well.’ Although the CVI on clarity and under—standing in the first round of interviews with the nine subjects was 0.89 and 1, respectively (table 4), subjects actually interpreted the meaning quite diversely. For example, they suggested the meaning to be knowing his or her medical background, habits, diet pattern, drug allergies and so on. In view of the broad interpretation spectrum, some subjects suggested a rewording to limit the scope to ‘medical aspect’. On consulting the orig—inal PCPCM developers in the USA, they confirmed that it was their intention to allow the subjects to have their own interpretations because how primary care had functioned and had added value to patients’ lives were actually complex notions. They suggested us to reword the translation to cover a larger meaning including the patient’s day to day life, medical problems, risk factors, health behaviours, what is important in his or her life, the patient’s dreams, failures and even larger aspirations. We hence reworded the question to ‘這位醫生或這間診所對我全人很了解’ meaning ‘This doctor or practice knows me as a person holistically’ in the second round of interviews. In contrary to our expectation, the CVI on clarity and understanding did not increase but dropped to 0.6. The subjects commented that the word holisticwas remote and inaccurate in their relationship with the doctors. From their experience, doctors would not know too much about a patient’s life other than the medical aspect. The local investigators (ETYT and CLKL) delib—erated on the item and suggested a rewording to ‘這位醫生或這間診所對我各方面的需要都很了解’ meaning ‘This doctor or practice knows my needs in all aspects’ as this seemed to be more comprehensible within the local Chinese context. The suggestion was supported by the US team. On testing that out with the subjects in the third and fourth rounds of interviews, the CVI on clarity and understanding rose to 1.
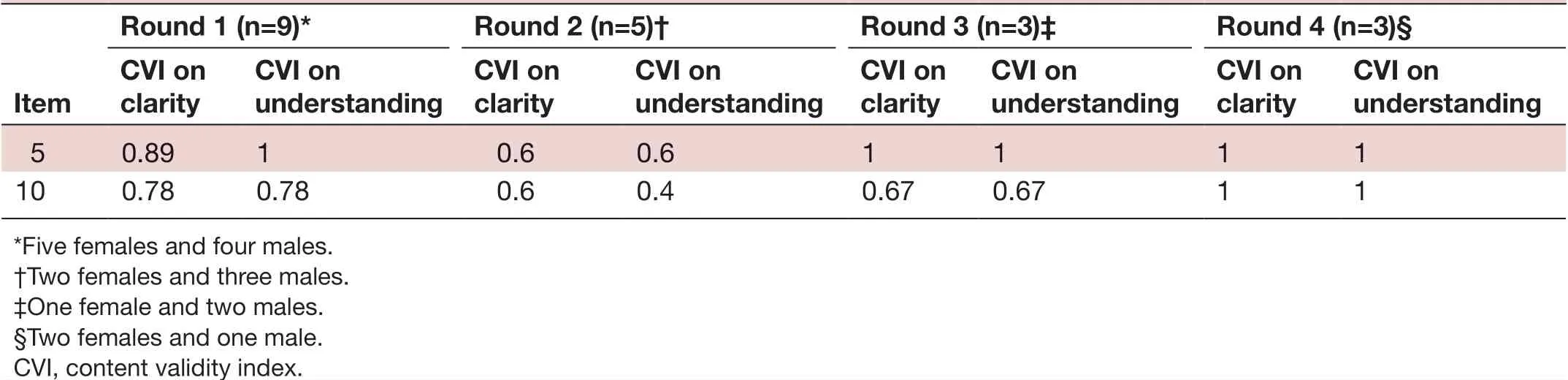
Table 4 CVI on clarity and understanding of items 5 and 10 in each round of interviews
The average CVI on relevance of items eight and nine were both 0.55. Those items were ‘The care I get takes into account knowledge of my family’ and ‘The care I get in this practice is informed by knowledge of my community’. For item eight, a few of the subjects stated that they had never talked about their family in front of the doctors. They thought that was beyond the scope of medical consultations. One subject even expressed that being asked about the family background during medical consultations would be too intrusive into one’s privacy. Among many subjects who thought the item was irrelevant to them, they believed it would be of higher relevance to patients at advanced age or with physical disabilities. For item nine, some subjects pointed out that the doctors in this clinic might not actually know much about the local community as they were not living in this district. Even if they knew the district well, that had nothing to do with taking care of patients. Only a minority of the subjects made the link that the doctor or the practice could mobilise resources in the community to help patients or could direct patients to services in the vicinity.
For item 10, the average CVI on clarity and under—standing was 0.75 and 0.70 (table 3), respectively. The English version of this item was ‘Over time, this practice helps me to meet my goals.’ We translated that into ‘這間診所一直在幫助我實現我的目標’ initially. The CVI on clarity and understanding in the first round of interviews with the nine subjects was both 0.78 (table 4). When looking into the subjects’ comments in details, actually many of them interpreted the item within the context of ‘health— related goals’. As the intention of this item in the original English PCPCM was to explore a larger context of different goals in life and the CVIs were just marginally low, we tried to keep the translation to test through the second and third round of interviews. However, the CVI on clarity still remained low (0.6 and 0.67) in these two rounds while the CVI on understanding further dropped to 0.4 and 0.67 in the second and third round, respec—tively. Advice was sought from our US team again and they agreed that it would be appropriate to add ‘health— related’ to the ‘goals’ concerned. We hence reworded the question to ‘這間診所一直在幫助我實現我健康相關的目標’ meaning ‘Over time, this practice helps me to meet my health— related goals’ in the fourth round of interviews. This time, the CVI on clarity and understanding rose to 1 (table 4).
Interpretations on individual items, suggestions of rewording by subjects and the follow— up actions taken by the investigators (where applicable) are listed in table 5.
Overall revisions made to the draft Chinese PCPCM
Based on the results of the cognitive debriefing interviews and discussion among the local and US investigators, revi—sions were made to items 5 and 10 only. The final version of the Chinese PCPCM is attached as online supplemental appendix 3.
DISCUSSION
A measure that can capture the patient— perceived value of primary care is much needed to evaluate the quality of care and to document the health benefit of interventions. Barbara Starfield differentiated beautifully the differ—ence between patient— centred and person— centred care. She stated ‘Both patient— centered and person— focused care are important, but they are different. In contrast to patient— centered care (at least as described in the current literature with assessments that are visit— based), person— focused care is based on accumulated knowledge of people, which provides the basis for better recognition of health problems and needs over time and facilitates appropriate care for these needs in the context of other needs. That is, it specifically focuses on the whole person’.8The PCPCM is a standardised and valid solution to assess primary care practice from an individual’s perspective.1Our study showed that the concept was applicable to the Chinese culture and an equivalent Chinese transla—tion was possible. The average content validity (CVI) index on clarity of each item is over 0.8 except item 10 (0.75). The average CVI on understanding of each item is over 0.8 except item 10 (0.7). The CVI in clarity and understanding of this item eventually reached 1 in the final round of interviews. The CVI on relevance of each item was ≥0.85 except items eight and nine. All items and response scale were considered generally applicable and valid in the Hong Kong Chinese primary care subjects.
We found our subjects had different interpretations of the meaning of item 5. The idea that ‘The doctor or a practice knows me as a person’ was rather foreign to the subjects attending busy public primary care clinics in Hong Kong. Some subjects interpreted it as ‘(The doctor) knows my medical record or my health conditions’. This demonstrated that semantic equivalence is not sufficient in the translation of a psychometric measure from one language to another. It is important to take into consider—ation of the cultural and contextual differences between the original and target populations. The clinical practice in USA is different from that in Hong Kong. The primary care home model advocated in the USA in the past two decades promoted more time on caring the patients on the whole and more attention to all aspects of their living.9Primary care in Hong Kong, similar to those in most other Chinese and Asian societies, is mainly doctor— led and the high workload limited the amount of time and scope ofservice patients can get. Another common problem in the system is that patients may not see the same doctor each time they attend because there are more than 10 doctors working in rotation in one clinic (as a norm in the local public primary care system). This leads patients to think along the line of different doctors ‘read and know their medical records or their health conditions’ instead of ‘know them as a person’. Our study revealed interesting cultural and practical context differences in the expecta—tion of person— centredness in primary care. It highlighted the importance of overcoming the regional, cultural and organisational differences in order to achieve practical global benchmarking in primary care service delivery and research collaboration.
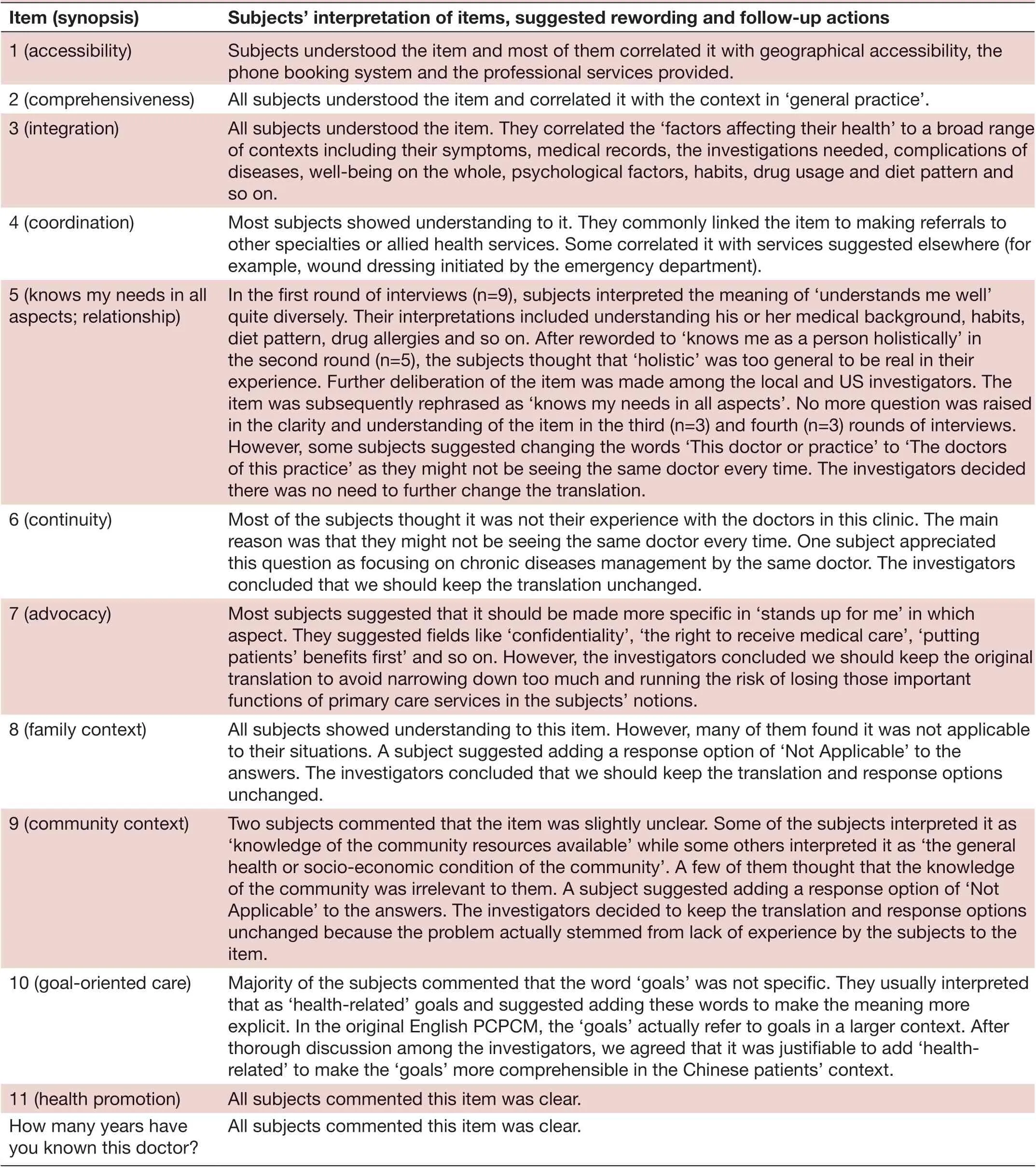
Table 5 Subjects’ interpretations on individual item, suggested rewording and investigators’ follow- up actions
Continued
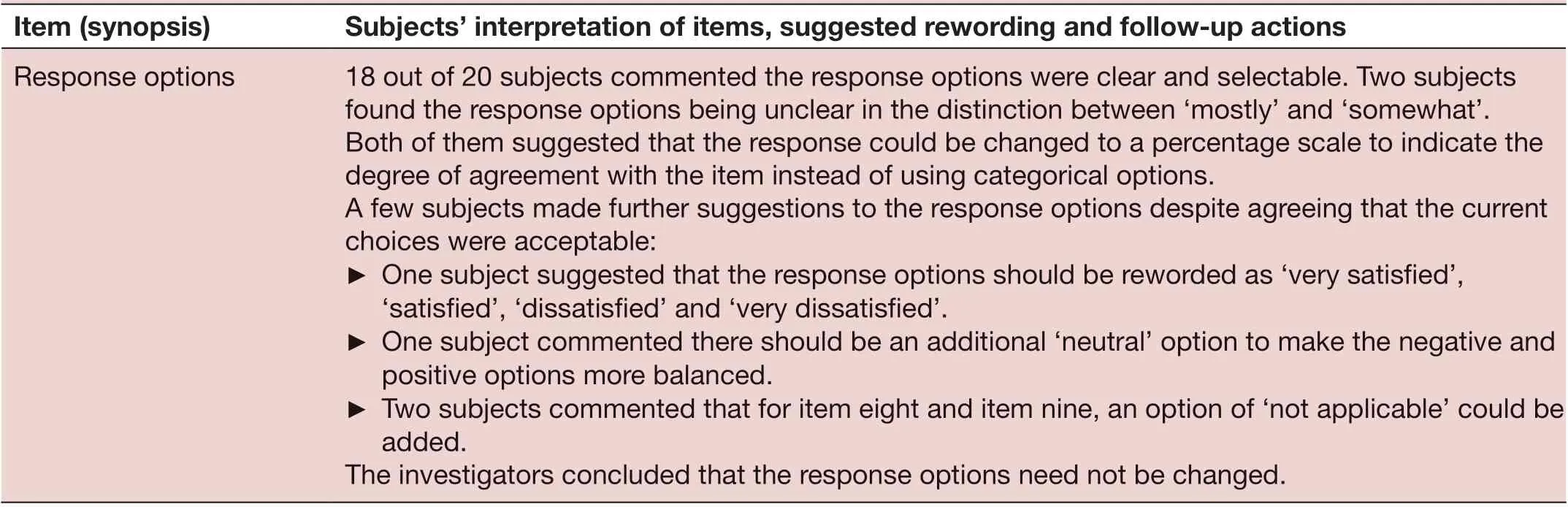
Table 5 Continued
Strengths and limitations
In our study, formal double forward— translations and backward— translations were applied. The original authors of the PCPCM reviewed the English back— translation to assure semantic equivalence of the Chinese translation.
However, our study shared the same limitation with other studies using cognitive debriefing: subjects may not have given ‘sufficient mental effort’ to the debriefing and it is difficult to assess if they have.1011Subjects might just want to give a socially desirable response, that is, faking good610leading to futile results. Another problem is the potential danger of using probing questions to identify subjects’ comprehension problems. For simple questions, subjects may be so automatic to give responses that do not need much cognitive processes. If subjects are prompted for elaboration of the questions or recommendations of rewording when none is available in their head, they may compose a vague reply rather than replying they have no idea.10
FUTURE RESEARCH
A respondent debriefing can be included in the cognitive debriefing. Other than just asking the probing questions on each item in the questionnaire, additional probing questions can also be asked on why the subjects chose the particular response items. It helps us to further under—stand how subjects interpreted the questions and how they reached their answers.12—14This kind of debriefing can help to recognise questions which subjects could not answer precisely.1215
CONCLUSION
In search of a concise and comprehensive new measure to evaluate the value of a primary care practice from the patients’ perspective, the Chinese translation of the PCPCM is now available and ready for further psycho—metric testing on a wider population to confirm its validity, reliability, sensitivity and responsiveness. Eventually, we can include person— centred care as a routine measure of quality and outcome of primary care in more countries, regions and cultures to benefit more residents.
TwitterCarlos King Ho Wong @CarlosWongHKU
AcknowledgementsWe would like to thank Professor Samuel Y S Wong, Dr Lee Siu Yin Ruby, Dr Tsang Chiu Yee Luke, Dr Wan Wing Fai, Dr Chiu Chi Fai Billy (from the academic, professional body, public and private clinical service fields) for their contributions in the Expert Review Panel at the beginning of the study to confirm the face validity of the English PCPCM in our local context. Thanks also go to Ms Lam Sau Mei Joyce, our project’s research assistant, who made a significant contribution to the implementation of the study, collection of the research data, statistical analysis, results interpretation and manuscript drafting.
ContributorsETYT, CLKL, WYC, RSE and KCS contributed to the concept of the study. ETYT, CLKL, CKHW, RSE, SJZ and KCS contributed to the analysis and interpretation of the data. ETYT, CLKL, WYC and CKHW contributed to the drafting of the manuscript. All authors contributed to the critical revision of the manuscript for important intellectual content and approved the final version for publication and took responsibility for the accuracy and integrity of the study.
FundingNew staff Start- up Package granted by Li Ka Shing Faculty of Medicine, The University of Hong Kong (204610519).
Competing interestsNone declared.
Patient consent for publicationNot required.
Ethics approvalInstitutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (HKU/HA HKW IRB), reference number UW 18-492.
Provenance and peer reviewNot commissioned; externally peer reviewed.
Data availability statementAll data relevant to the study are available on reasonable request.
Open accessThis is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY- NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non- commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non- commercial. See: http:// creativecommons. org/ licenses/ by- nc/ 4. 0/.
ORCID iDsEmily Tsui Yee Tse http:// orcid. org/ 0000- 0001- 7409- 9507 Carlos King Ho Wong http:// orcid. org/ 0000- 0002- 6895- 6071
——记郑州市郑东新区中州大道小学
 Family Medicine and Community Health2020年4期
Family Medicine and Community Health2020年4期
- Family Medicine and Community Health的其它文章
- Perceived barriers and primary care access experiences among immigrant Bangladeshi men in Canada
- The process of transprofessional collaboration: how caregivers integrated the perspectives of rehabilitation through working with a physical therapist
- Reformulation and strengthening of return- of- service (ROS) schemes could change the narrative on global health workforce distribution and shortages in sub- Saharan Africa
- New hypertension and diabetes diagnoses following the Affordable Care Act Medicaid expansion
- How well did Norwegian general practice prepare to address the COVID-19 pandemic?
- Family medicine residency training in Ghana after 20 years: resident attitudes about their education
