Split-dose vs same-day bowel preparation for afternoon colonoscopies: A meta-analysis of randomized controlled trials
Nasim Parsa, Eric A Grisham, Courtney J Cockerell, Michelle L Matteson-Kome, Ramakrishna V Bysani, Sami Samiullah,Douglas L Nguyen, Veysel Tahan, Yezaz A Ghouri, Srinivas R Puli,Matthew L Bechtold
Nasim Parsa, Eric A Grisham, Courtney J Cockerell, Michelle L Matteson-Kome, Ramakrishna V Bysani, Sami Samiullah, Veysel Tahan, Yezaz A Ghouri, Matthew L Bechtold, Division of Gastroenterology and Hepatology, Department of Medicine, University of Missouri - Columbia, Columbia, MO 65212, United States
Douglas L Nguyen, Division of Gastroenterology, Heart of the Rockies Regional Medical Center, Colorado Springs, CO 80907, United States
Srinivas R Puli, Division of Gastroenterology, University of Illinois - Peoria, Peoria, IL 61604, United States
Abstract
Key Words: Afternoon; Colonoscopy; Preparation; Split-dose; Same-day; Meta-analysis
INTRODUCTION
Colorectal cancer (CRC) is a common and devastating disease resulting in significant cancer deaths around the world[1,2]. Colonoscopy remains the screening test of choice for CRC and the only method which encompasses both diagnostic and therapeutic potential[3]. Afternoon colonoscopies have higher rates of suboptimal bowel preparation[4]. Suboptimal bowel preparations are associated with prolonged procedure time, low adenoma detection rate, and increased patient discomfort, complications, and healthcare costs[5-7].
Several studies have suggested that the quality of bowel cleansing for afternoon colonoscopies depends on timing and quantity of the bowel preparation[8,9]. Some studies have shown that split-dosing bowel preparations (SpD) is superior to sameday preparation (SaD, the morning of the procedure) with regard to both cleansing efficacy and tolerability, while other studies report that SaD has a better cleansing and tolerability compared with SpD. Currently, the U.S. Multi-Society Task Force on Colorectal Cancer (USMSTF) recommends SaD regimen as an alternative for SpD for colonoscopies in the afternoon[10]This recommendation was made based on the results of one prospective study comparing the SaD regimen with the SpD regimen and two randomized controlled trials (RCTs) using controls with day-prior regimens[6,11,12].
Recently published RCTs on this topic report mixed results. Moreover, data pooling from the RCTs is challenging given varied bowel preparation regimens and bowel preparation scales. Therefore, a meta-analysis of the RCTs to compare the SaD with the SpD regimens for afternoon colonoscopies was performed.
MATERIALS AND METHODS
Literature search and study selection
Literature search was conducted with a three-fold system. First, multiple databases, including EMBASE, Cochrane databases, MEDLINE/PubMed, Google Scholar, CINAHL, and Scopus were searched in November 2019 for afternoon and colonoscopy. Second, major conference proceeding abstracts (Digestive Disease Week, American College of Gastroenterology, United European Gastroenterology meetings) were searched through November 2019. Third, references from identified studies were searched for any potentially omissions. If data required clarification, we communicated with the authors.
Data extraction
All RCTs on adults comparing the SaD with SpD regimen for afternoon colonoscopies, using the Ottawa bowel preparation score (OBPS) were included. Exclusion criteria were patients < 18 years old or non-RCTs. To reduce confounding, subgroup analyses were performed for the same formulation and volume of bowel preparation using polyethylene glycol with electrolytes (PEG). Two authors (Parsa NP and Grisham EA) independently reviewed all the studies for inclusion and extracted data using standard forms. Any disagreements on inclusion or data extraction were settled by the senior author (Bechtold ML).
Quality assessment of studies
The Cochrane’s Collaboration Risk of Bias Tool was used to assess the quality of studies[13-15]. For each study, a grade, as described as low, moderate, or high, was based on the assessment of limitations, effect magnitude, precision, publication and other forms of bias, and consistency of results[13-15].
Statistical analysis
A meta-analysis was conducted comparing SaD and SpD for afternoon colonoscopies by calculating pooled estimates of quality of bowel preparation. Outcomes were analyzed using mean difference (MD) or odds ratio (OR) by the DerSimonian and Laird method (the random-effects model). TheI2measure of inconsistency was used to assess heterogeneity (P< 0.10 orI2> 50% was deemed significant). If heterogeneity was discovered, researchers used performed a sensitivity analysis to remove the least amount of studies necessary to reach non-significant heterogeneity by comparing results to the original pooled data. RevMan 5.3 (Review Manager, Version 5.3, Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2012) was used for statistical analysis. Funnel plots assessed for publication bias.
RESULTS
Article search and quality assessment
Evaluation of titles and abstracts resulted in 663 articles being identified. After review, 21 articles remaining in which 11 satisfied the inclusion criteria (n= 1846) with mean age range of 51.6-61.8 years[16-26](Figure 1). Studies were global, including many countries (United States, Spain, Italy, China, Korea, India) (Table 1). Most of the studies were deemed high-quality studies based on quality assessment (Table 2).
Overall results
Eight RCTs reported the mean OBPS (n= 1328)[17-21,23-25]. Eight studies reported the number of satisfactory bowel preparations (n= 1483)[16,19,21-26]. Of these, 1202 had satisfactory bowel preparations with 578 in the SaD group and 624 in the SpD group. There was no difference between SaD and SpD for the mean OBPS (MD 0.33; 95%CI:-0.09-0.75;P= 0.13;I2= 74%) (Figure 2A) or the number satisfactory bowel preparations (79.1%vs83%; OR 0.77; 95%CI:0.57-1.03;P= 0.07;I2= 5%) (Figure 2B) despite a trend favoring SpD. Given significant heterogeneity in the mean OBPS analysis, a sensitivity analysis was performed which showed similar results without significant heterogeneity when one study[23]was eliminated (OR 0.18; 95%CI:-0.11-0.46;P= 0.22;I2= 36%).
Same formulation bowel preparation (PEG)
Five studies reported the mean OBPS (n= 877)[17,20,21,23,25]. There was no difference between SaD and SpD for mean OBPS (MD 0.45; 95%CI:-0.13-1.02;P= 0.13;I2= 78%) (Figure 3A). Five studies reported the number of satisfactory bowel preparations (n= 1045)[21-23,25,26]. Of these, 862 had satisfactory bowel preparations (82.5%) with 415 in the SaD group and 447 in the SpD group. There was no difference between SaD and SpD for number satisfactory bowel preparations (81%vs84%; OR 0.83; 95%CI:0.51-1.35;P= 0.46;I2= 39%) (Figure 3B). Given significant heterogeneity in the mean OBPS analysis, a sensitivity analysis was performed which showed similar results without significant heterogeneity when one study[23]was eliminated (OR 0.26; 95%CI:-0.02-0.54;P= 0.07;I2= 0%).
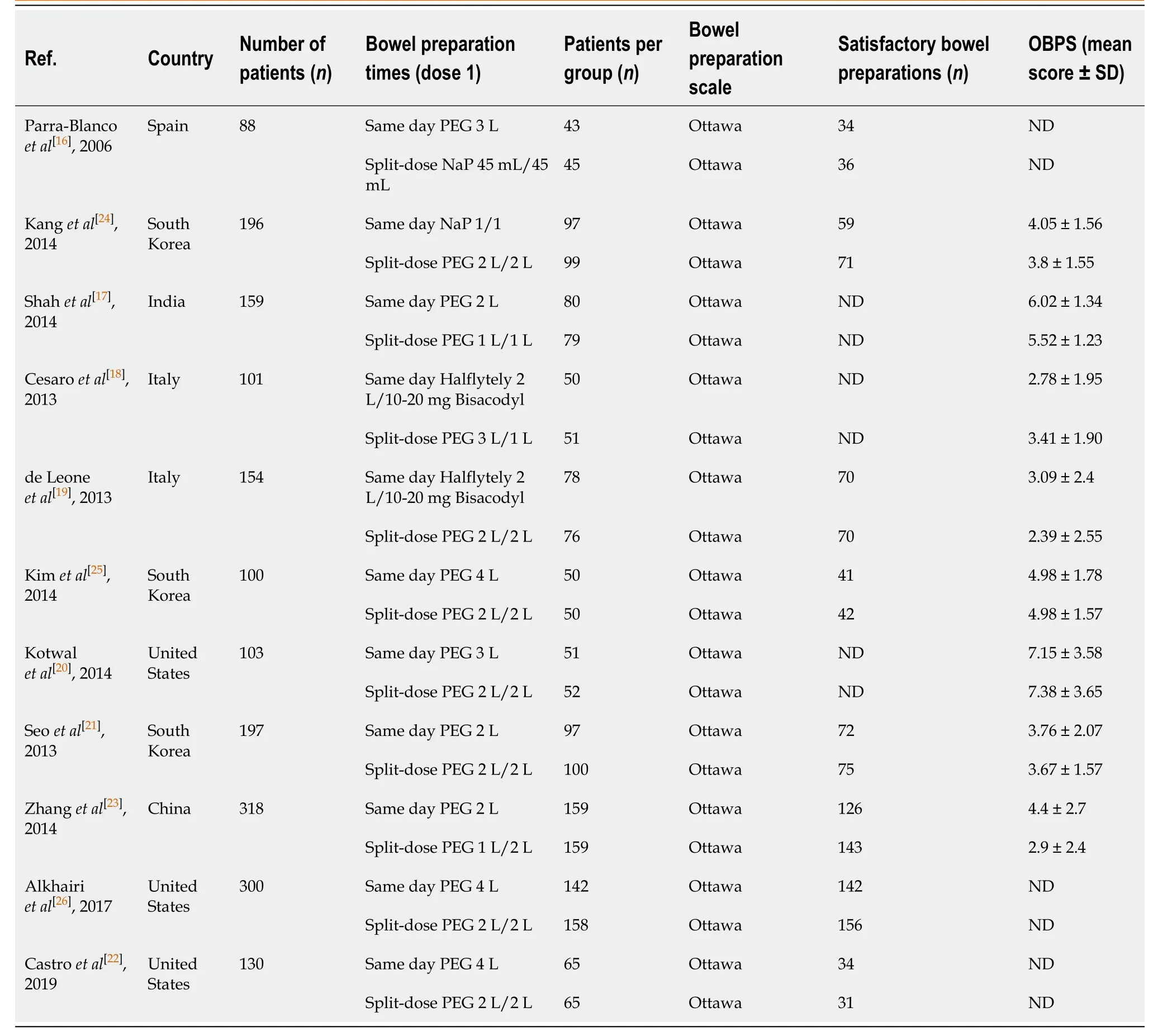
Table 1 Description of studies included in the meta-analysis
Same formulation and volume bowel preparation (4 L PEG)
Three studies reported the mean OBPS (n= 362)[17,20,25]. There was no difference between SaD and SpD for mean OBPS (MD 0.30; 95%CI:-0.08-0.68;P= 0.12;I2= 12%) (Figure 4A). Three studies reported the number of satisfactory bowel preparations (n= 530)[22,25,26]. Of these, 446 had satisfactory bowel preparations with 217 in the SaD group and 229 in the SpD group. There was no difference between SaD and SpD for number satisfactory bowel preparations (84.4%vs83.9%; OR 1.14; 95%CI:0.65-2.01;P= 0.64;I2= 0%) (Figure 4B).
Publication bias
For any outcome, no significant publication bias was identified (Figure 5).
DISCUSSION
The USMSTF currently recommends the SaD bowel preparation as an alternative to SpD for afternoon colonoscopies[10]. This recommendation, which is based on “high-quality evidence”, is based on one prospective study and two RCTs that their control groups received a day-prior bowel preparation regimen[6,11,12]. Since this recommendation, several high-quality trials have evaluated and compared the efficacy of SaDvsSpD for afternoon colonoscopies, supporting the value of this study.

Table 2 Quality assessment of studies included in meta-analysis based upon Cochrane’s Collaboration Risk of Bias tool

Figure 1 Details of search algorithm.
The practice of SaD bowel preparation was supported by two meta-analyses published in 2017. Both studies concluded the noninferiority of the SaD compared with the SpD regimen with regards to bowel preparation for afternoon colonoscopies, consistent with the findings of our study[27,28]. Avaloset al[27]conducted a meta-analysis on 11 RTCs comparing the efficacy of bowel preparation quality between the SaD and SpD regimens and reported a similar results for the bowel preparation quality, patient willingness to repeat the procedure and adenoma detection rate, although SaD patients reported less bloating and improved quality of sleep. Chenget al[28]pooled the results of 14 RTCs and reported comparable results between the SaD and SpD regimens for bowel preparation with substantial heterogeneity (I2= 60%), so subgroup analysis was performed to evaluate the influence of bisacodyl on bowel preparation. Comparing SaDs with bisacodyl to SpDs without it the previous evening showed the results favored SaDs (I2= 0%). If both arms eliminated adjuvants, the analysis revealed that patients in the SpD arm had better bowel preparation with no heterogeneity (OR 0.66; 95%CI: 0.49-0.88). Heterogeneity was a significant limitation of these metaanalyses as many studies used varied bowel preparation scales in the study arms. Furthermore, neither compared the SaD and SpD regimens among patients who received same formula and volume bowel preparation.

Figure 2 Forest plot showing overall bowel preparation results between same-day preparation vs split-dose preparation for afternoon colonoscopies.
This meta-analysis is the first comparing SaDvsSpD bowel preparation for afternoon colonoscopies that used identical validated scales to evaluate the bowel preparation quality. No significant differences were identified between the SaD and SpD regimens for quality of bowel preparation by total OBPS. Moreover, we performed a comprehensive subgroup analysis in order to minimize potential confounding factors. Further subgroup analyses showed no differences in terms of satisfactory bowel preparation based on OBPS between the two groups when receiving the same preparation formula (PEG) as well as receiving same preparation formula and volume (4 L PEG). Only RCTs in adult patients were evaluated and used in this meta-analysis. Moreover, by using the OBPS, which evaluates the bowel preparation quality before the application of any cleansing maneuvers, the amount of time and adequacy of cleaning was not an issue, thereby limiting confounding variables. Results of our study can help guide clinicians and patients to select the optimal method for bowel preparation. The current guidelines indicate that providers are responsible for maintaining optimal bowel preparations at greater than 85%, which is often affected by inadequate bowel preparation ingestion by patients[10]. Given a lack of clinical differences, both SaD and SpD regimens should be offered to patients and their preference should be considered in order to maximize their adherence. This may potentially minimize procedure cancellations and increase the success rates of afternoon colonoscopies.

Figure 3 Forest plot showing same bowel preparation results between same-day preparation vs split-dose preparation for afternoon colonoscopies.

Figure 4 Forest plot showing same bowel preparation (type and volume) results between same-day preparation vs split-dose preparation for afternoon colonoscopies.
The strengths of this meta-analysis are abundant. Inclusion of worldwide RCTs in varying populations, including China, Korea, Spain, Italy, India, and United States, allows for generalization to many populations. Second, the quality of RCTs included were moderate-to-high. Given the lack of ability to blind the patient to the bowel preparation, the included studies were the highest exceptional quality possible. Third, to minimize confounding factors, extensive subgroup analyses were performed and only studies with the same bowel preparation and the same bowel preparation with same volume were evaluated. This effort limits significant confounding factors. Finally, the OBPS was used which limits confounding variables of cleaning effort and cleaning time since evaluated prior to cleaning. Limitations of this meta-analysis were observed. First, significant heterogeneity was observed in two outcomes. Besides a diversity of bowel preparation across studies, there were slightly varied preparations within study arms. Furthermore, some using SaD or SpD preparations with or without bisacodyl. For those two outcomes with significant heterogeneity, sensitivity analyses were performed with similar results without significant heterogeneity when Zhanget al[23]was removed. Second, the type of diet as well as the length of diet restriction during preparation varied among studies and therefore, the influence of diet on bowel preparation could not be further analyzed.

Figure 5 Funnel plot showing no publication bias.
CONCLUSION
In conclusion, our meta-analysis showed that no difference exists between SaD and SpD bowel preparation for the number of satisfactory bowel preparations in the afternoon colonoscopies. Both options should be offered to patients in order to maximize adherence and increase afternoon colonoscopy success rates.
ARTICLE HIGHLIGHTS
Research background
Bowel preparation for afternoon colonoscopies is important for screening for colorectal cancer.
Research motivation
Bowel preparation for afternoon colonoscopies is controversial. Examining the best approach would be beneficial for patients and those performing colonoscopies.
Research objectives
This meta-analysis examines the use of same-day preparation (SaD) or split-dose preparation (SpD) for afternoon colonoscopies.
Research methods
An extensive literature search was conducted using multiple databases. Only randomized controlled trials in adults that compared SaD to SpD with Ottawa bowel preparation score (OBPS) were included. Odds ratio or mean difference was used to analyze outcomes.
Research results
No differences were observed for satisfactory bowel preparation based on OBPS among participants receiving SaD vs SpD overall (P = 0.07), when the two groups received the same preparation formula (polyethylene glycol, PEG) (P = 0.46), and when the two groups received the same formula and volume (4 L PEG) (P = 0.64).
Research conclusions
In patients undergoing afternoon colonoscopies, SpD is comparable with SaD in terms of satisfactory bowel preparations.
Research perspectives
Patients and proceduralists may be confident in using either SaD or SpD for afternoon colonoscopies.
 World Journal of Meta-Analysis2020年6期
World Journal of Meta-Analysis2020年6期
- World Journal of Meta-Analysis的其它文章
- Comparison of hand-assisted laparoscopic radical gastrectomy and laparoscopic-assisted radical gastrectomy: A systematic review and meta-analysis
- How far has panic buying been studied?
- COVID-19-associated stroke risk: Could nutrition and dietary patterns have a contributing role?
