含有微乳头状结构的乳腺单纯型黏液癌临床病理特征与预后分析
晏佩佩 蔡宏伟 冯晓敏
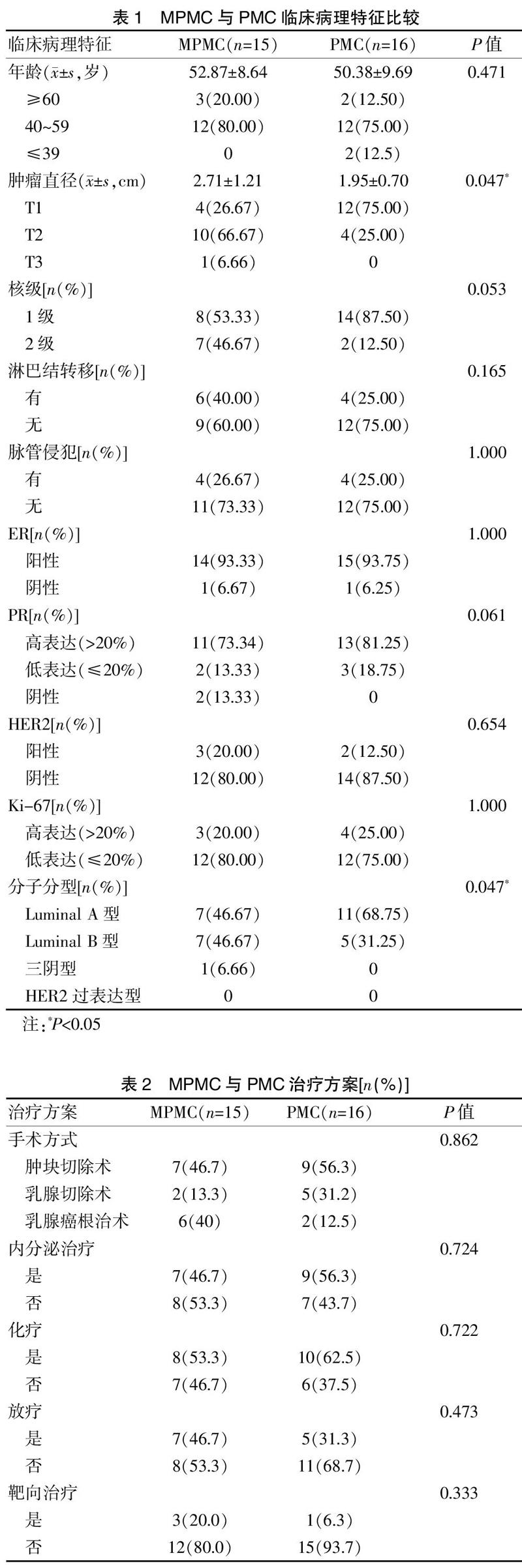
[摘要] 目的 探讨含有微乳头状结构的乳腺单纯型黏液癌(MPMC)与乳腺单纯型黏液癌(PMC)的临床病理特征与预后差异。 方法 筛选2013年4月至2020年11月在本院确诊的31例PMC病例(MPMC 15例,PMC 16例),對临床病理特征及预后进行分析。 结果 MPMC肿瘤直径更大,Luminal B型比例高(P<0.05),MPMC中级别核级比例及淋巴结转移率呈增高趋势。两组脉管侵袭率、ER、PR和HER2、Ki67阳性率比较,差异无统计学意义(P>0.05)。两组各有1例复发转移,均无死亡病例。 结论 与PMC相比,MPMC侵袭力有一定程度的增加,两组预后无明显差异。
[关键词] 微乳头;黏液癌;乳腺;临床病理
[中图分类号] R737.9 [文献标识码] B [文章编号] 1673-9701(2021)31-0142-03
[Abstract] Objective To investigate the difference in clinicopathological characteristics and prognosis between pure mucinous carcinoma of breast with micropapillary feature (MPMC) and pure mucinous carcinoma of breast (PMC). Methods A total of 31 PMC patients (15 MPMC patients and 16 PMC patients) diagnosed in our hospital from April 2013 to November 2020 were screened. The clinicopathological characteristics and prognosis were analyzed. Results The diameter of MPMC tumor was larger and proportion of Luminal B type was higher(P<0.05). The proportion of middle nuclear grade and rate of lymph node metastasis showed an increasing trend in MPMC. There were no statistical differences in vascular invasion rate,ER,PR,HER2 and Ki67 positive rate between the two groups(P>0.05).There was 1 patient of recurrence and metastasis in each group, and there was no death. Conclusion Compared with PMC, the invasiveness of MPMC is increased to a certain extent. There is no significant difference in prognosis between the two groups.
[Key words] Micropapillary; Mucinous carcinoma; Breast; Clinicopathology
乳腺单纯型黏液癌(Pure mucinous carcinoma of the breast,PMC)的形态温和、含有大量细胞外黏液,预后良好[1],细胞外黏液可能限制了肿瘤扩散[2]。浸润性微乳头状癌(Invasive micropapillary carcinomas,IPMC)侵袭性强,预后差[3]。2002年Ng等[4]首次报道了含有微乳头状结构的单纯型黏液癌(Micropapillary pattern of pure mucinous carcinoma of the breast,MPMC)病例,提出将其作为黏液癌的一种新亚型。Mukherjee等[5]认为微乳头状结构可能改变肿瘤侵袭性行为,Bal等[6]认为MPMC是惰性的,微乳头状结构与预后无相关性。目前关于MPMC的研究结论不一致,因此,本研究收集了15例MPMC进行研究分析,探讨微乳头状结构是否会增加PMC的侵袭性,影响预后,现报道如下。
1 资料与方法
1.1 一般资料
收集2013年4月至2020年11月南京市妇幼保健院确诊为PMC的病例31例,均为女性,其中15例为MPMC。
1.2 方法
所有标本经10%中性福尔马林固定、包埋、4 μm厚度连续切片、HE染色后镜下观察,用Envision两步法行免疫组化染色,并设立阴性、阳性对照。免疫组化所用一抗雌激素受体(Estrogen receptor,ER)、孕激素受体(Progesterone receptor,PR)购自福州迈新公司,Ki67、EMA购自北京中杉金桥公司,人类表皮因子生长受体-2(Human epidermal growth factor receptor 2,HER2)购自罗氏公司。
1.3 判读标准
ER、PR、Ki67阳性为胞核着色,计算阳性细胞百分率。参照2018年美国临床肿瘤学会/美国病理学家学会的乳腺癌HER2检测指南对HER2进行评分[7],判定为2+病例通过荧光原位杂交确定为阴性/阳性。
1.4 统计学方法
采用SPSS 23.0统计学软件进行数据分析,用Fishier确切概率法比较两组之间的临床病理特征,P<0.05为差异有统计学意义。
2 结果
2.1 临床资料
MPMC平均年龄(52.87±8.64)岁,PMC平均年龄(50.38±9.69)岁。见表1。MPMC与PMC手术与治疗方案见表2。
2.2 病理特征
MPMC肿瘤直径0.8~5.5 cm,平均(2.71±1.21)cm,PMC肿瘤直径1~4 cm,平均(1.95±0.70)cm,差异有统计学意义(P<0.05)。MPMC细胞核级、淋巴结转移与脉管侵犯率见表1。
2.3 免疫组化结果
免疫结果见封三图6,MPMC微乳头状结构EMA外周膜阳性(封三图6F),部分病例见沙砾体(封三图6E)。MPMC组Luminal B型占比高于PMC(P<0.05)。ER、PR、HER2、Ki-67阳性率见表1。
2.4 随访结果
MPMC随访中位时间56个月(6~90个月),1例复发转移、3例失访。PMC随访中位時间49个月(6~91个月),1例复发转移、2例失访,均无死亡病例。
3 讨论
乳腺黏液癌是一种少见的乳腺癌亚型[1]。2002年,Ng等[4]首次报道含有微乳头状结构的PMC,提出将其作为黏液癌新亚型。有学者[8]发现IPMC侵袭性强,脉管浸润和淋巴结转移率高,黏液癌中的微乳头状结构可能影响肿瘤的生物学行为[5];MPMC也可能是PMC的变型[9],大量的细胞外黏液限制了肿瘤扩散[2],细胞外黏液的含量可能与预后相关[10]。
Kim等[10]将微乳头状成分超过50%的病例归入MPMC;Sun等[11]的纳入标准是微乳头状成分超过1%,本研究纳入标准为微乳头状成分超过50%。PMC好发于中老年女性,MPMC倾向于较年轻的患者[1]。Xu等[12]发现MPMC肿瘤直径更大,肿瘤细胞核大部分为低-中级别核[13]。众所周知,Luminal B型乳腺癌在诊断与治疗方面更复杂,对内分泌治疗敏感性低,预后较差。本研究发现MPMC中Luminal B型比例更高(P>0.05),但随访期内两组患者预后无差异。
TP53和PIK3CA是ER阳性乳腺癌常见的突变基因,IPMC的TP53和PIK3CA突变频率高,1q扩增、16q缺失。Pareja1等[14]发现5例MPMC中2个例16q缺失,3例TP53和PIK3CA的突变频率低。Daniela等[15]检测10例MPMC和11例PMC样本,发现MPMC的PI3K-Akt、mTOR和黏着斑通路等发生改变,这些通路与各种癌症的侵袭性转移相关。MPMC可能在基因水平上不同于PMC,某些特定基因组改变可能是肿瘤侵袭性行为的原因。
在2019年版WHO中提到含有微乳头状结构的黏液癌,但未明确诊断标准,需要更多的病例被报道,才能从形态学、基因改变等方面全面描述这一少见肿瘤,为临床治疗提供更准确的方向。
[参考文献]
[1] WHO Classificaion of Tumours Editorial Board. Breast tumours, lyon (france):International agency for research on cancer[S]. WHO Classification of Tumours series,2019.
[2] Komaki K,Sakamoto G,Sugano H,et al. Mucinous carcinoma of the breast in Japan. A prognostic analysis based on morphologic features[J].Cancer,1988,61(5):989-996.
[3] Gokce H,Durak MG,Akin MM,et al.Invasive micropapillary carcinoma of the breast:A clinicopathologic study of 103 cases of an unusual and highly aggressive variant of breast carcinoma[J].Breast J,2013,19(4):374-381.
[4] Ng WK.Fine-needle aspiration cytology findings of an uncommon micropapillary variant of pure mucinous carcinoma of the breast:Review of patients over an 8-year period[J].Cancer,2002,96(5):280-288.
[5] Mukherjee A,Russell R,Chin SF,et al. Associations between genomic stratification of breast cancer and centrally reviewed tumour pathology in the metabric cohort[J]. NPJ Breast Cancer,2018,4(5):1-9.
[6] Bal A,Joshi K,Sharma SC,et al. Prognostic significance of micropapillary pattern in pure mucinous carcinoma of the breast[J]. Int J Surg Pathol,2008,16(3):251-256.
[7] Antonio C Wolff,M Elizabeth Hale Hammond,Kimberly H Allison,et al. Human epidermal growth factor receptor 2 testing in breast cancer:American society of clinical oncology/college of American pathologists clinical practice guideline focused update[J].J Clin Oncol,2018,36(20):2105-2122.
[8] Siriaunkgul S,Tavassoli FA. Invasive micropapillary carcinoma of the breast[J]. Mod Pathol,1993,6(6):660-662.
[9] Shet T,Chinoy R. Presence of a micropapillary pattern in mucinous carcinomas of the breast and its impact on the clinical behavior[J].Breast J,2008,14(5):412-420.
[10] Kim HJ,Park K,Kim JY,et al. Prognostic significance of a micropapillary pattern in pure mucinous carcinoma of the breast:Comparative analysis with micropapillary carcinoma[J].J Pathol Transl Med,2017,51(4):403-409.
[11] Sun P,Zhong ZX,Lu QY,et al. Mucinous carcinoma with micropapillay features is morphologically,clinically and genetically distinct from pure mucinous carcinoma of breast[J]. Modern Pathology,2020,33(10):1945-1960.
[12] Xu XL,Bi R,Shui RH,et al. Micropapillary pattern in pure mucinous carcinoma of the breast-does it matter or not[J]. Histopathology,2019,74(2):248-255.
[13] 王佩,王映梅,李春梅,等.乳腺浸潤性微乳头状黏液癌14 例临床病理分析[J]. 临床与实验病理学杂志,2018, 34(5):572-575.
[14] Parejal F,Selenica1 P,Brown DN,et al. Micropapillary variant of mucinous carcinomas of the breast display genetic alterations intermediate between mucinous carcinomas and micropapillary carcinomas[J]. Histopathology,2019,75(1):139-145.
[15] Daniela Miricescu,Alexandra Totan,Iulia-Ioana Stanescu-Spinu,et al. PI3K/AKT/mTOR signaling pathway in breast cancer: From molecular landscape to clinical aspects[J].Int J Mol Sci,2020,22(1):173.
(收稿日期:2021-07-10)

