Role of novel biomarkers in kidney transplantation
Kurtis J Swanson, Fahad Aziz, Neetika Garg, Maha Mohamed, Didier Mandelbrot, Arjang Djamali, Sandesh Parajuli
Kurtis J Swanson, Fahad Aziz, Neetika Garg, Maha Mohamed, Didier Mandelbrot, Arjang Djamali, Sandesh Parajuli, Department of Medicine, University of Wisconsin School of Medicine and Public Health, Madison, WI 53705, United States
Arjang Djamali, Department of Surgery, University of Wisconsin School of Medicine and Public Health, Madison, WI 53705, United States
Abstract Clinical application of biomarkers is an integral component of transplant care. Clinicians and scientists alike are in search of better biomarkers than the current serologic (serum creatinine, donor-specific antibodies), urine-derived (urinalysis, urine protein), and histologic ones we now use. The science behind recent biomarker discovery spans across multiple molecular biologic disciplines, including transcriptomics, proteomics, and metabolomics. Innovative methodology and integration of basic and clinical approaches have allowed researchers to unearth molecular phenomena preceding clinical disease. Biomarkers can be classified in several ways. In this review, we have classified them via their origin and outcome: Primarily immunologic, i.e., representative of immune regulation and dysfunction and non-immunologic, pertaining to delayed graft function, cardiovascular events/mortality, infection, malignancy, posttransplant diabetes, graft, and patient survival. Novel biomarker uses to guide the diagnosis and management of transplant-related outcomes is a promising area of research. However, the use of biomarkers to predict outcomes after kidney transplantation is not well studied. In this review, we summarize the recent studies illustrating biomarker use and transplant outcomes.
Key Words: Biomarkers; Kidney Transplantation; Rejection; Infection; Mortality; Graft survival
INTRODUCTION
Kidney transplantation is the optimal renal replacement therapy for patients with endstage kidney disease (ESKD). Kidney transplant recipients (KTRs) experience survival benefits in all age groups, have improved health-related quality of life, and kidney transplantation is cost-effective compared to hemodialysis or peritoneal dialysis[1-3]. Surveillance of allograft dysfunction is integral to post-transplant management. Ideally, graft injury should be detected and treated before irreversible damage occurs. The gold standard for assessing kidney allografts has been histologic analysisviabiopsy[4]. Allograft biopsies are imperfect, as they can miss early, reversible pathology. Also, they carry approximately a 1%-2% risk of significant complications[5].
Serial measures of glomerular filtration rate along with qualitative/quantitative measures of urine albumin have been the mainstay of allograft surveillance since they are non-invasive, readily available, and interpretable. Changes in these parameters, however, are often neither sensitive or specific, unpredictive of outcomes, and occur late in the disease[6]. This has led to the need for non-invasive predictive data to allow clinicians to more readily diagnose and manage allograft pathology: Novel biomarkers.
What is a biomarker? The National Institutes of Health Biomarker Definition Working Group provides the subsequent definition: A characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic responses, or pharmacological responses to a therapeutic intervention[7]. Another definition per the World Health Organization is the following: Any substance, structure, or process that can be measured in the body or its products and influence or predict the incidence of outcome or disease[8].
In this review, our focus is to highlight biomarker use in the context of key kidney transplant outcomes. As such, we classified biomarkers based on immunological and non-immunological related outcomes. With immunological outcomes pertaining primarily to rejection and immune tolerance, this section offered an opportunity to stratify biomarkers further based on their relation to the immune system. The nonimmunological section, which was highlighted by biomarkers related to tissue injury primarily, was categorized by meaningful outcomes to emphasize the predictive value of these biomarkers. In cases of the novel, unique pathways, further description is provided accordingly.
Over the past several years, the field of biomarker research has grown exponentially as scientists and physicians alike are searching for novel ways to non-invasively detect allograft perturbations early-to help guide management and prognosticate both allograft and patient outcomes. As seen in a commentary in 2018 regarding the most recent iteration of the Banff classification for rejection from 2017, language regarding “thoroughly validated gene transcripts/classifiers” as adjuncts to diagnose antibodymediated rejection (ABMR) affirms the emergence of biomarkers as an additional tool to surveil and diagnose post-transplant pathology[9].
In this review, we aim to summarize the most current literature from the past 5 year (2015-present date) on novel biomarkers in kidney transplant recipients and their relevance to fundamental kidney transplant outcomes.
NOVEL BIOMARKER CLASSIFICATION
Novel biomarker use can be classified into 2 main categories: Immunologic and nonimmunologic. Immunologic biomarkers are those characterizing immune dysfunction ranging from subclinical to overt rejection. Non-immunologic biomarkers are those that demonstrate adverse transplant outcomes whereby immune dysfunction is not the sole aberration at play,e.g., delayed graft function, cardiovascular events, infection, malignancy. While an oversimplification, as innate and humoral immunity are rooted in most pathophysiologic responses, these categories provide a logical classification scheme for the myriad types of novel biomarkers.
Immunological
Surveillance and optimization of recipient immune status are vital to prolonged allograft and patient survival. While current practice offers means to risk-stratify patients for poor immunologic outcomes [human leukocyte antigen mismatch, sensitization, calculated panel reactive antibodies, pre-transplant donor-specific antibodies (DSA)], our current surveillance measures (creatinine, urine protein to creatinine ratio) fail to capture clinically unsuspected rejection, which occurs in 20%-25% of patients after kidney transplant[10]. In other words, early molecular level events occur below our current detection thresholds, leading to missed opportunities for intervention, prevention, and management of poor outcomes. Several recent studies offer promising findings to diagnose, treat, and prognosticate adverse immunologic outcomes.
Chemokines:Chemokines are signaling proteins capable of inducing movement of certain cell types to areas of interest. Chemokines arise early in the immune cascade of rejection and thus can act as biomarkers to non-invasively identify deleterious immune events. Both urine and plasma chemokines have been studied extensively to detect immunologic dysfunction.
In one study, Rabantet al[11]showed that urinary C-terminal amino acid sequence Cystine-X-Cystine (C-X-C) motif chemokines 9 and 10, interferon gamma (IFN-γ) dependent chemokines secreted by various leukocytes along with renal mesangial and tubular cells, correlated with tubulointerstitial and microvascular inflammation (t + i score; g + peritubular capillaritis score; allP< 0.001). The ratio of urinary C-X-C motif chemokine ligand ten (CXCL10) to urine creatinine diagnosed T cell-mediated rejection (TCMR) [area under the curve (AUC) = 0.80, 95% confidence interval (CI): 0.68-0.92;P< 0.001] and ABMR [AUC = 0.76 (95%CI: 0.69-0.82);P< 0.001]. Furthermore, CXCL10: Creatinine plus DSA improved diagnosis of ABMR [AUC = 0.83 (95%CI: 0.77-0.89);P< 0.001] and CXCL10: Creatinine ratio at the time of ABMR predicted risk of graft loss[11]. Similarly, Hriciket al[12]in their study from 2015 showed that positive urinary C-X-C motif chemokine ligand nine is predictive of acute rejection (AR) by a median of 15 d before clinical detection[12].
Urinary chemokines (C-X-C motif chemokine ligand nine specifically) were assessed for their predictive value of 5-year graft outcomes in a more recent study, but no clear association was observed[13].
Plasma-derived fractalkine, IFN-γ, and interferon gamma-induced protein ten were evaluated for prediction of AR in a recent study of 87 KTRs; the combined measure of fractalkine on day 0, interferon gamma-induced protein ten and IFN-γ on day 7 was predictive of AR in 1 month (AUC = 0.866) with a sensitivity of 86.8% and a specificity of 89.8%[14]. In a recent study of 65 KTRs, interleukin (IL)-8 was found to predict rejection with higher levels at day 7, day 30 (P= 0.023, 0.038), and correlate with serum creatinine (Pearsonr= 0.621,P= 0.001)[15].
Another promising biomarker is soluble cluster of differentiation thirty (CD30), a tumor necrosis factor glycoprotein derived from T cells that regulates the balance between T helper type 1 and T helper type 2 immune responses. Early post-transplant elevations within the first 2 weeks in one study predicted AR (AUC = 0.775;P= 0.004) with the sensitivity of 88.8%, specificity of 46.3%[16]. These findings are summarized in Table 1.
In summary, chemokines have potential as novel biomarkers, particularly for predicting acute cellular and antibody-mediated rejection. Prediction of long term outcomes such as graft survival and patient survival, however, were limited. Chemokines may be a useful adjunct to predict early rejection events in kidney transplantation.
Free micro ribonucleic acid:Free micro ribonucleic acid (RNA) are small non-coding RNA segments integral to cellular function. While also present in homeostasis, in certain contexts, they signal perturbations at the molecular level, ergo are linked to disease. Free micro RNA have been studied extensively in renal pathology, both in native and transplanted kidneys. Given their regulatory roles and stability bothin vivoand in vitro, they exude potential as robust biomarkers. Several recent studies demonstrate the role of free micro RNA as biomarkers[17].
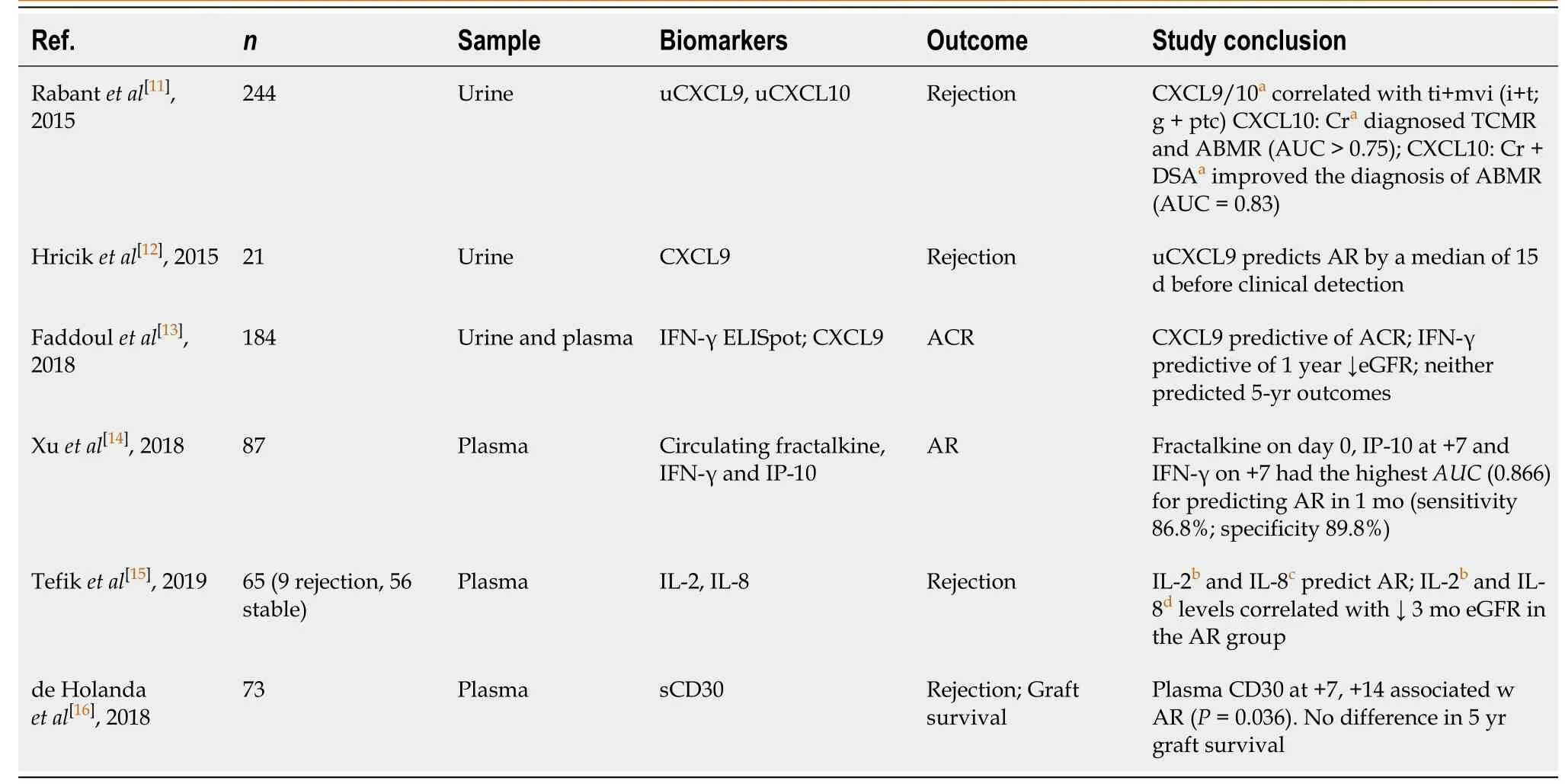
Table 1 Summary of novel biomarker studies of chemokines associated with immunologic outcomes
In their 2016 study of 160 patients, Matzet al[17]showed that the expression levels of specific serum microRNAs miR-15B, miR-103A, and miR-106A discriminated patients with stable graft function significantly from patients with TCMR (P= 0.001996, 0.0054 and 0.0019 respectively) and from patients with urinary tract infection (P= 0.0001, < 0.0001 and = 0.0001)[17]. This group expounded on these findings with a later study, where they showed that miR-223-3p, miR-424-3p, and miR-145-5p distinguished TCMR and ABMR from stable graft function as well as identifying miR 145-5P as a distinct marker of interstitial fibrosis/tubular atrophy[18].
The utility of urine-derived free microRNA was demonstrated in a study of 80 KTRs from 2017 where urinary miR-155-5P predicted AR (AUC = 0.875;P= 0.046) with an 85% sensitivity and 86% specificity[19].
In a major study of 519 KTRs utilizing microRNA from allograft biopsies, Halloranet al[20]showed that use of a centralized microarray algorithm utilizing microRNA, the Molecular Microscope®Diagnostic System, can not only support histology (agreement between Molecular Microscope®Diagnostic System and histology 77% for TCMR, 77% ABMR, 76% no rejection with blinding to histology) but also is more consistent with clinical judgment (87%) than histology (80%) (P= 0.0042) in regards to select casesn= 451 biopsies)[20].
Ledegancket al[21]provided the most comprehensive analysis of microRNAs in the context of kidney transplants in their recent review. They cited 11 studies whereby microRNA upregulation and downregulation were associated with TCMR, ABMR, and chronic ABMR. Across studies, consistently noted biomarkers include the following: miR-142, miR-155, miR-223 (upregulated) and miR-125, miR-30, miR-204 (downregulated)[21].
In their comprehensive review of novel biomarkers, Jamshaidet al[22]reported on a high grade study from 2015 by Lorenzenet al[23]examining long noncoding RNAs[22,23]. In their study of 93 KTRs (31 stable controls without rejection, 62 patients with AR, plus 10 samples from the rejection cohort after antirejection treatment), they found that RP11-354P17.15-001 (L328) was associated with acute TCMR (AUC = 0.76,P< 0.001; sensitivity 49%, specificity 95%). Moreover, L328 normalized after successful antirejection treatment. Interestingly, 51/62 patients presented with subclinical rejection, defined as no change in creatininei.e.L328 was able to detect subclinical rejection[23]. A synopsis of these studies can be found in Table 2.
In summary, free microRNA appears to help discriminate rejection from nonrejection as well as subtypes of AR. Interestingly, these biomarkers were durable despite blinding to histology and consistent with clinical judgment as cited by Halloranet al[20]Free microRNA, particularly from allograft biopsy tissue, appears to enhance diagnosis of rejection and can supplement histology[20].
Leukocyte subclasses:The predominance and activity of different subclasses of leukocytes can indicate recipient immune status. Leukocyte populations thus can serve as biomarkers to detect and identify immune aberrancy preceding clinical disease.
One such population is donor-reactive memory B cells (mBCs). Donor-reactive memory B cells are a subset of the B cell pool with emerging data supportive of a robust response to alloantigen post-transplant[24]. In a 2018 study, mBCs were associated with rejection; in 85 KTRs who underwent for-cause biopsies, donor reactive mBCs were found in 100% patients with ABMR andde novoDSA. They were also present in 72%-80% of patients with chronic ABMR with and without DSA. In the 90 non-sensitized patients, mBC expansion occurred at a higher rate than de novo DSA and independently predicted ABMR [AUC = 0.917 (95%CI: 0.879-0.956);P< 0.001][25].
Donor-specific memory CD4 T cells have also been implicated in rejection. In their study from 2016, Gorbachevaet al[26]showed that in a murine model, mice sensitized with memory CD4 cells experienced an acute rise in serum creatinine > 1 mg/dL (1.7 ± 0.6 mg/dL by 6–8 d post-transplant) and developed allograft failure at 7 days. At the time of rejection, the recipient mice had high titers of DSA and increased frequencies of donor–reactive T cells producing IFN-γ compared with controls at matching time points[26].
Through the use of genomics in combination with histologic scoring, Yazdaniet al[27]were able to derive specific immune cell types and demonstrate that the presence of natural killer (NK) cells are predictive of ABMR (AUC = 0.98,P< 0.001); ABMRvsTCMR (AUC = 0.91,P< 0.001) as well as ABMR histology. They found that 22/24 biopsies with microvascular inflammation (g + ptc) had elevated NK levels (AUC = 0.89,P< 0.0001). Moreover, activated NK cells had the best predictive capability of graft failure at 1-2 years compared to other leukocytes (AUC = 0.74). Notably, NK cell infiltration predicted graft failure independent of histologic diagnosis (P= 0.039)[27].
In their study from 2017, Cortes-Cerisueloet al[28]found that in 23 KTRs receiving belatacept-based immunosuppression, patients with a higher frequency of cluster of differentiation twenty-eight and cluster of differentiation four T-cells experienced more rejection[28]. Though counterintuitive, the authors postulated that this was related to CD28+ cells exhibiting a pro-inflammatory phenotype relative to CD28-subset. With optimal cutoff determination, they were able to discriminate rejectors from nonrejectors with a sensitivity of 80% and specificity of 100%. Therefore, cluster of differentiation twenty-eight and cluster of differentiation four frequencies can act as a biomarker to determine optimal candidates for belatacept therapy. The studies mentioned above are summarized in Table 3.
In summary, leukocyte subclasses offer unique opportunities as biomarkers in that they (1) offer another vantage point into antigen-antibody dynamics that can occur independently of or preceding detectable donor-specific antibodies (2) highlight the role of less understood pathophysiologic mechanisms (NK cells) and their predictability of graft failure and (3) can potentially provide clinicians with an individualized recipient immune profile to guide management in terms of immunosuppression.
Gene expression profiles:Gene expression profiling (GEP) is an approach within the field of molecular biology whereby thousands of genes are analyzed simultaneouslyviamessenger RNA to describe cellular function. Differential expression of genes, particularly those associated with immune cells and interleukins, are some of the earliest events leading to immune dysregulation and poor transplant outcomes. Consequently, these gene expression profiles can yield robust, viable biomarkers. Multiple encouraging profiles have been developed recently as cited below.
In their study of 307 KTRs from Clinical Trials in Organ Transplantation-8, Friedewaldet al[10]created a rejection biomarker for subclinical acute rejection (sc-AR) based on GEP, which had the following characteristics: [sensitivity 64%, specificity 87%, positive predictive value (PPV) 61%, negative predictive value (NPV) 88%]. Moreover, their GEP biomarker was predictive of persistent subclinical AR[10].
A similar study examining the Genomics of Chronic Renal Allograft Rejection cohort led to the development of the Targeted Expression Assay, which allowed for the prediction of sc-AR at 3 months in 113 KTRs (AUC = 0.830; NPV = 0.98, PPV = 0.79)[29].
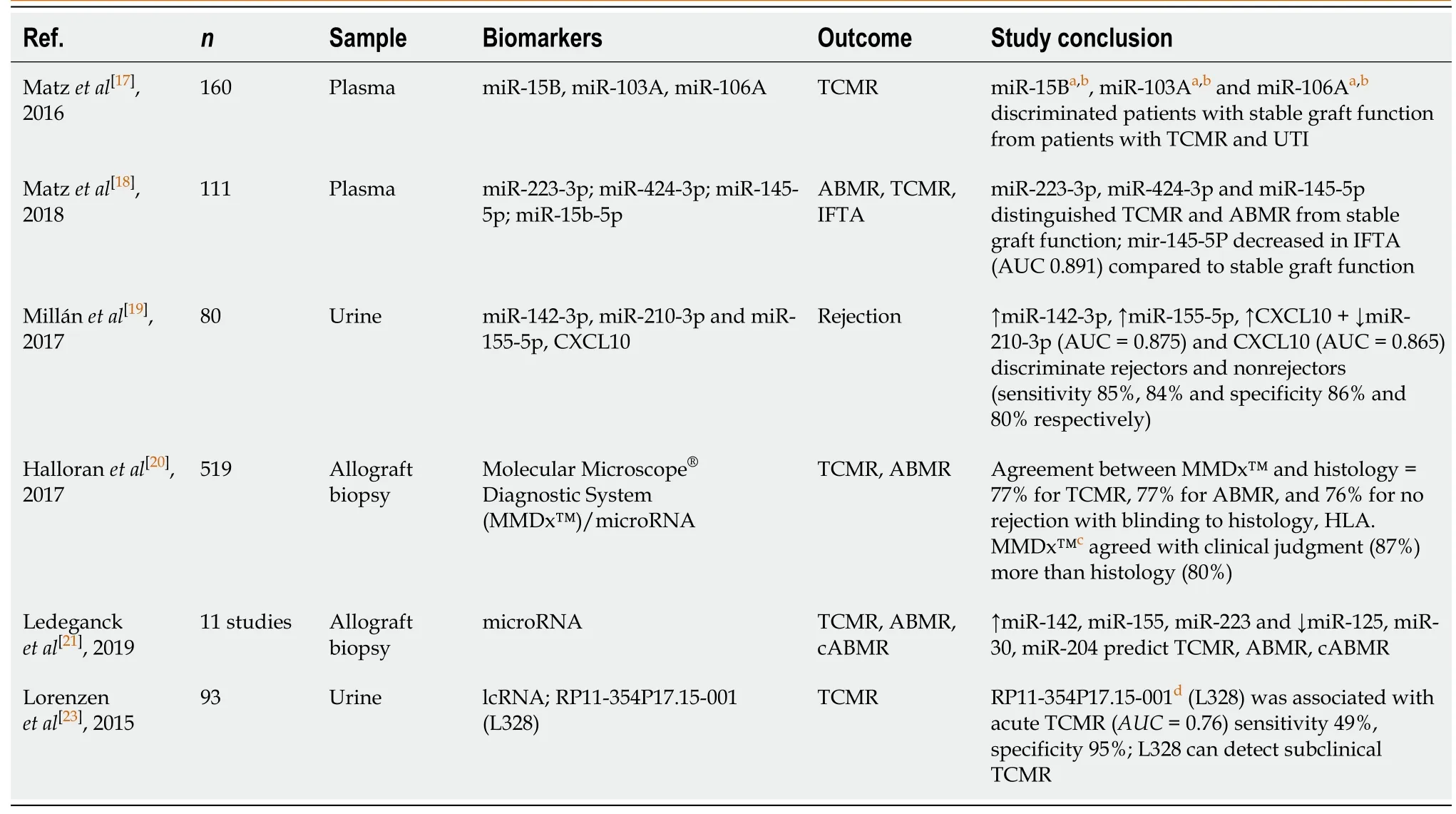
Table 2 Summary of micro-ribonucleic acid-related novel biomarker studies associated with immunologic outcomes
A significant development in gene expression assays in kidney transplantation was the development of the Kidney Solid Organ Response Test. This is a 17 gene set created in 2014 that was found to detect AR accurately. Crespoet al[30]expanded on this work with the use of Kidney Solid Organ Response Test plus IFN-γ enzyme-linked immunosorbent spot assay in the Evaluation of Sub-Clinical Acute Rejection Prediction trial of 75 KTRs where they found that in combination, these assays synergistically can predict sc-AR, subclinical T cell-mediated rejection and subclinical antibody-mediated rejection (AUC > 0.85,P< 0.001)[30].
One of the most promising gene expression profiles is the TruGraf®Molecular diagnostic test, a non-invasive test to surveil patients with a stable renal function that is now reimbursed by Medicare. This test was first validated in 2014 whereby Kurianet al[31]showed that the TruGraf®GEP could distinguish patients with rejection from those with non-rejection dysfunction and excellent allograft function[31].
In 2019, Firstet al[32]expanded on these findings with TruGraf®in their study both retrospectively and prospectively. In their retrospective arm, they found that in the evaluation of 192 patients at 7 transplant centers, in 87.5% of the cases, investigators’ clinical decisions were influenced by TruGraf®test results. In the prospective arm of 45 patients at 5 centers, TruGraf®supported 87% of the clinical decisions with 93% of investigators stating they would use TruGraf®in subsequent patient care. In these studies, TruGraf®often led to the non-invasive diagnosis, affirming conservative approaches as well as obviating the need for biopsy[32].
Gene expression profiles can also be derived from urine, as demonstrated in a study from 2019, where a common rejection module of 11 genes was analyzed from 150 KTRs. Interestingly, an accurate prediction from 2 genes (Proteasome 20S Subunit Beta 9, CXCL10) was equivalent to the 11-gene model (sensitivity 93.6%, specificity 97.6%)[33]. Table 4 summarizes these studies.
In summary, gene expression profiles are promising biomarkers in surveilling immune status. As seen by their validation, reimbursement from the Centers for Medicare and Medicaid Services, and acceptance among investigators, gene expression profiles are helping to pave the way for broader use of biomarkers in kidney transplantation.
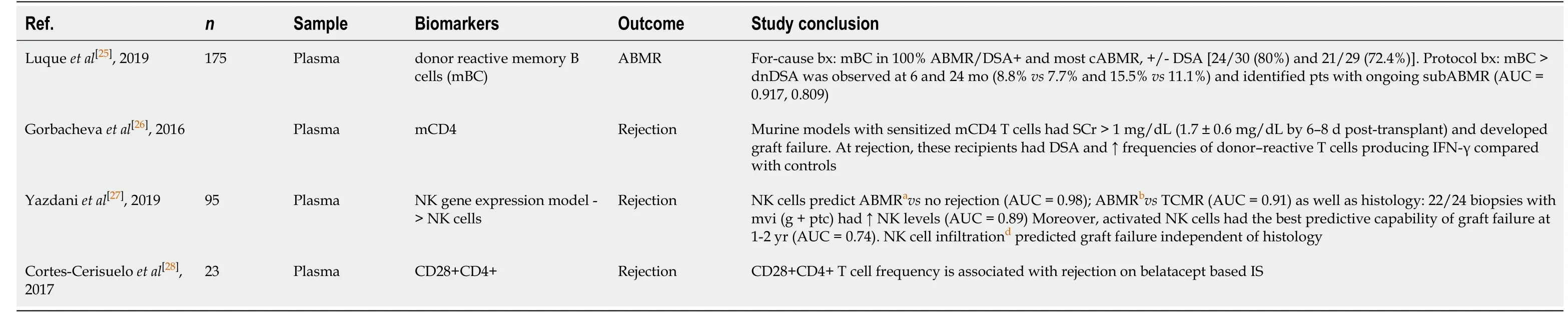
Table 3 Summary of leukocyte subclass related biomarkers associated with immunologic outcomes
Donor-derived cell-free deoxyribonucleic acid:Allograft transplantation can be considered genome transplantation with grafts having a unique allogenomic signature. At baseline, cell-free deoxyribonucleic acid (DNA) is circulating at low levels. However, in the case of injury, including rejection, increased high levels of cellfree DNA are shed into the bloodstream and are thus measurable as a biomarker. Becket al[34]described quantification and reference values for donor-derived cell-free deoxyribonucleic acid (dd-cfDNA) in their study from 2015[34]. Given this recent quantification, dd-cfDNA is a nascent area of research. Donor-derived cell-free DNA has been shown to predict the decline in estimated glomerular filtration rate (eGFR), de novo donor-specific antibody formation, and biopsy-proven rejection in multiple studies. Three recent studies highlight the utility of dd-dfDNA[35].
In their study of 189 KTRs, Oellerichet al[35]found that in patients with biopsyproven rejection, median dd-cfDNA (cp/mL) was 3.3-fold and median dd-cfDNA (%) 2.0-fold higher than medians in stable patients without rejection. Receiver operating characteristic analysis showed superior performance (P= 0.02), of measuring ddcfDNA (cp/mL) (AUC = 0.83) compared to dd-cfDNA (%) (AUC = 0.73). Diagnostic odds ratios were 7.31 for dd-cfDNA (cp/mL), and 6.02 for dd-cfDNA (%) respectively. Remarkably, plasma creatinine showed a low correlation (Pearsonr= 0.37) with ddcfDNA (cp/mL)[35].
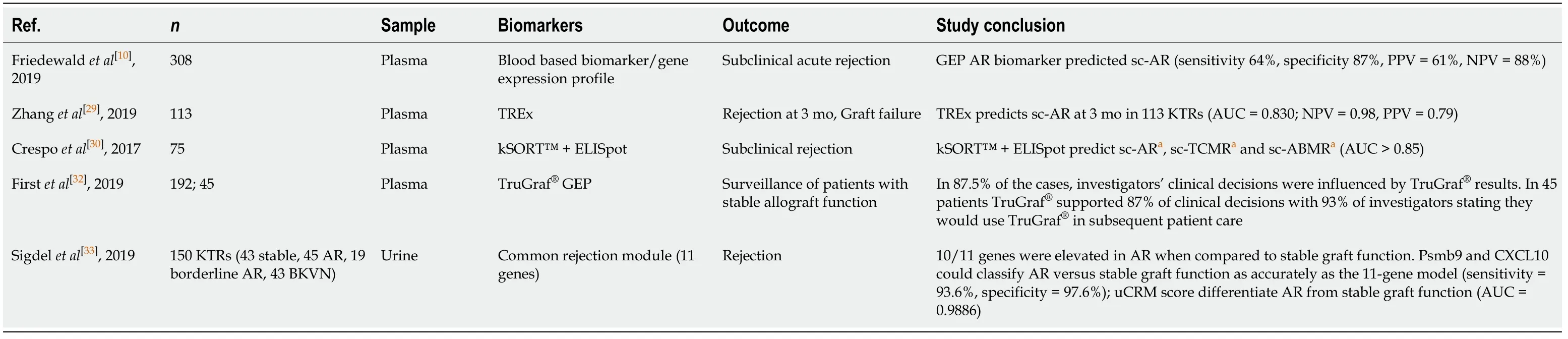
Table 4 Summary of gene expression related biomarkers associated with immunologic outcomes
Stiteset al[36]in examining 79 KTRs with TCMR 1A/borderline rejection found that forty-two patients had elevated dd-cfDNA compared to thirty-seven patients with low levels; elevated levels of dd-cfDNA predicted adverse clinical outcomes, including eGFR decline by 8.5%vs0% in low dd-cfDNA patients (P= 0.004), de novo donorspecific antibody formation was seen in 40% (17/42)vs2.7% (P< 0.0001), and future or persistent rejection occurred in 9 of 42 patients (21.4%)vs0% (P= 0.003)[36].
One of the most important developments in dd-cfDNA technologies has been targeted next-generation sequencing techniques. These techniques allow for the quantification of dd-cfDNA without the need for the prior donor or recipient genotyping[37].
One of the more well-known assays, Allosure®, has been validated in several studies. Notably, Allosure®is commercially available and reimbursed by Medicare. In the study Circulating Donor-Derived Cell-Free DNA in Blood for Diagnosing Acute Rejection in Kidney Transplant Recipients study (ClinicalTrials.gov Identifier: NCT02424227) from 2017, it was shown to discriminate rejection from controls (AUC = 0.74,P< 0.0001; PPV = 61%, NPV = 84%); as well as ABMR from non-ABMR [AUC = 0.87 (95%CI: 0.75-0.97)][38]. Ongoing trials using Allosure®(clinical trials NCT04057742, NCT03326076) are being conducted at various transplant centers throughout the country.
In their comprehensive review on dd-cfDNA, Knightet al[39]cited 2 recent studies (Huanget al[40]and Whitlamet al[41]) of its application in the context of kidney transplantation[39-41]. In their study of 63 KTRs, Huanget al[40]found that dd-cfDNA discriminated patients with ABMR (median 1.35%; interquartile range (IQR): 1.10%-1.90%) compared to those with no rejection (median 0.38% (IQR: 0.26% to 1.10%);P< 0.001). dd-cfDNA did not distinguish TCMR from no rejection however. Whitlamet al[41]in their study of 61 KTRs, found that dd-cfDNA concentration and fraction were predictive of acute antibody-mediated rejection (aAMR) (AUC = 0.92, 0.85) and composite diagnosis of ABMR (AUC = 0.91, 0.89). Graft derived cell free DNA (gdcfDNA) exhibited modest sensitivity (0.90; 0.85) and specificity (0.88, 0.79) for aAMR and ABMR[41]. These findings are summarized in Table 5.
Donor-derived cell-free DNA is a robust biomarker in predicting rejection outcomes. Moreover, there is evidence supporting its ability to predict longer-term outcomes. The use of dd-cfDNA as a supportive tool for diagnosis and management is already taking place with the implementation of Allosure®and other similar assays.
Immune tolerance: In addition to identifying immune dysfunction, biomarkers can reflect immune quiescence and tolerance in kidney transplant recipients. While this terminology is vague, Mathewet al[42]in their review, define immune tolerance nicely as “long-term allograft survival in the absence of immunosuppressive treatment and the presence of stable donor-specific immune responsiveness[42].” In one review, Chanonet al[43]describe biomarker identificationviadifferential expression from a tolerance group (stable graft function or healthy non-transplant volunteers) compared to a dysfunction group (acute or chronic rejection). They cite several potential biomarkers, including T cell, B cell, and macrophage populations, as well as genomic signatures from B and T cells along with microRNA[43]. In a recent review, Newellet al[44]describe that in 32 tolerant individuals, 31 genes (26 B cell-specific) distinguished tolerant from non-tolerant KTRs[44]. Two promising genes, cited in prior studies are B cell receptor genes immunoglobulin kappa variable 1D-13 and immunoglobulin kappa variable 4-1[44,45].
While less clear of an outcome than others described previously, immune tolerance is one of the primary aims after kidney transplantation. Having tools to validate and reassure clinicians beyond our current insensitive measures and/or detect early perturbations before overt disease manifests can improve patient care.
Non-immunological
The use of biomarkers to identify and predict transplant outcomes applies to nonimmune related outcomes. In the following sections, various biomarkers will be discussed in the context of their non-immune outcomes.
Graft quality:Assessing allograft quality/viability is an essential step in kidney transplantation to appropriately allocate organs and predict future outcomes. With the incidence of ESKD increasing and improved transplant outcomes, the demand for donation continues to grow. Refined preservation techniques have helped to broaden the donor pool, giving way to viable donation with higher risk allografts. This in turn has narrowed the margin of error for prognosticating graft quality. In the past five years, biomarker discovery has emerged to help appraise potential allografts. Several robust studies are described below:
Parikhet al[46]described in their study of 671 KTRs that perfusate biomarkers of tissue injury were associated with 6-month allograft functionviaeGFR: Each doubling of perfusate neutrophil gelatinase-associated lipocalin (NGAL) and liver fatty acidbinding protein were independently associated with lower 6-month eGFR (1.7 mL/min per 1.73 m2; 1.48 mL/min per 1.73 m2respectively)[46].
Moseret al[47]in their study of 41 donor kidneys [16 Live donors, 16 donations after brain death (DBD); 9 donations after circulatory death (DCD)] undergoing machine cold perfusion, compared various tissue injury biomarkers. They found that tissue injury markers matrix metalloproteinase-2, lactate dehydrogenase, and NGAL were found in highest perfusate concentrations in DCD kidneys, followed by DBD and living donor allografts (allP< 0.0001)[47].
In their unique study comparing modified adenosine and lidocaine (AL) solution to the University of Wisconsin (UW) solution for organ preservation, Hamaouiet al[48]utilized perfusate lactate in addition to histology and perfusion dynamics to help compare viability. They found that in 10 DCD porcine kidneys perfusedviahypothermic machine perfusion with modified AL solution had significantly lower perfusion lactate levels (3.1 mmol/Lvs4.1 mmol/L,P= 0.04) during reperfusion than those in UW solution. Of note, on histology, UW solution perfused kidneys had a greater degree of tubular dilatation than modified AL kidneys (P= 0.03). This demonstrates a potential application of perfusate lactate to detect ischemia-reperfusion injury[48].
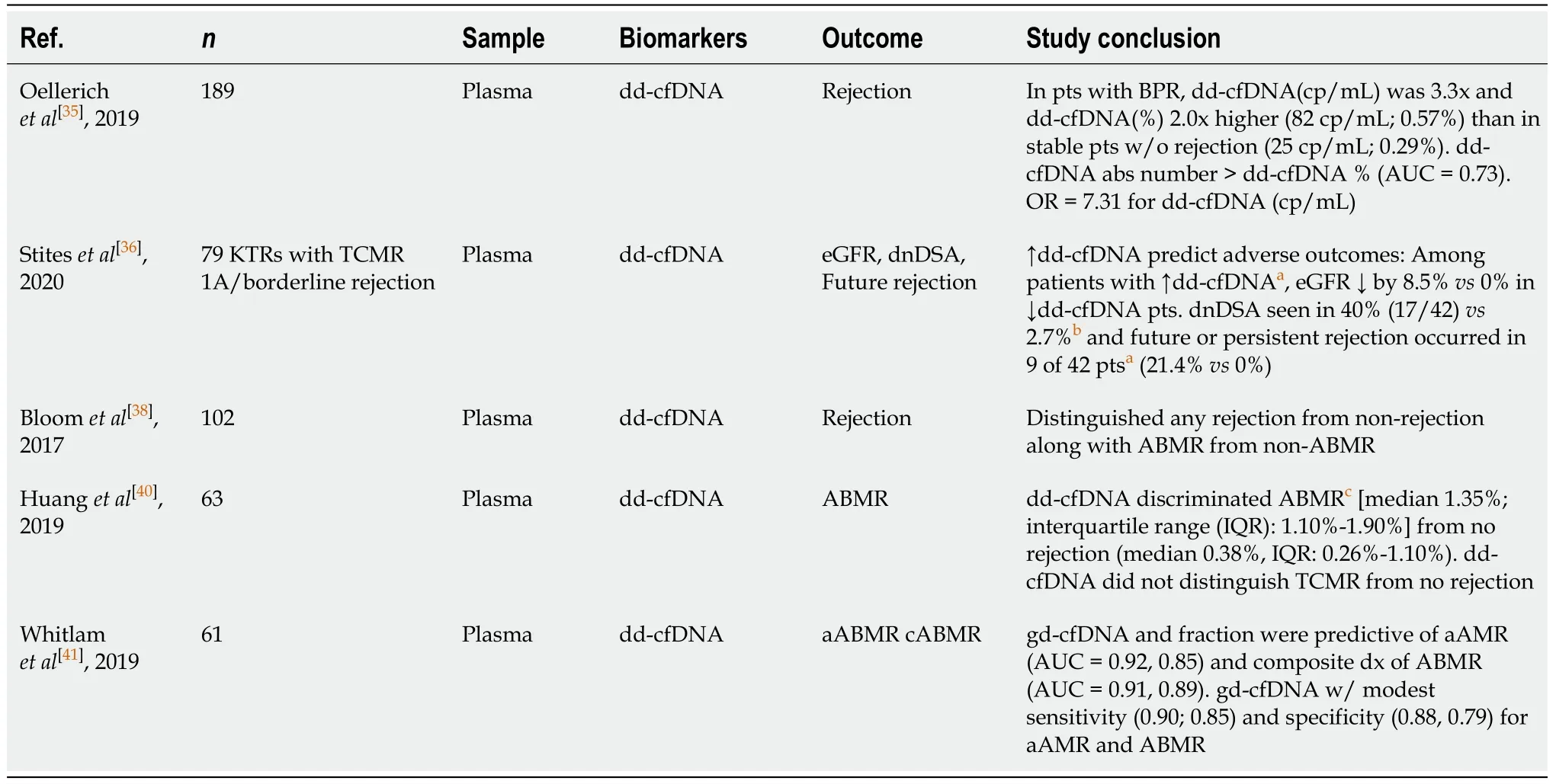
Table 5 Summary of donor-derived cell-free deoxyribonucleic acid biomarkers associated with immunologic outcomes
A notable recent study is that of van Smaalenet al[49]from 2017. The investigators examined cytotoxic extracellular histones, which have been described as markers of cell injury (as seen in inflammation, thrombosis, sepsis namely) in 390 DCD kidney perfusates and sought to determine if their presence was associated with allograft viability. They found extracellular histone concentration was independently associated with 1-year graft failure [hazard ratio (HR) = 1.386 (95%CI: 1.037-1.853)]. Moreover, they observed that 1-year graft survival was improved for the low extracellular histone group (83%vs71%,P= 0.008), which was maintained up to 5 years (76%vs65%,P= 0.014)[49].
In their recent study from 2019, Weissenbacheret al[50]utilized perfusate allograft injury biomarkers NGAL and kidney injury molecule-1 (KIM-1) in addition to histology, urine output, sodium levels to help quantify allograft viability in the context of normothermic kidney perfusion with urine recirculation. While their study was limited in terms of size (11 allografts), lack of organ transplantation, and differing methods (urine recirculationvsnot), the highest perfusate NGAL level was found in the lowest quality kidney (Kidney 4). In the perfused kidneys without urine recirculation, NGAL and KIM-1 decreased over time, but as the authors conclude, with such a small sample size, it is difficult to assign any predictive value based on this cohort[50].
In their review from 2020, De Beuleet al[51]nicely summarize the current status of the allograft viability assessment. They illustrate potential roles for different biomarkers in different perfusion contextse.g., hypothermic, normothermic machine perfusion[51]. In the context of hypothermic machine perfusion, they, in conjunction with a recent meta-analysis performed by Guzziet al[52]report that glutathione Stransferase and its isoforms alpha- and pi-, a family of detoxification enzymes associated with acute kidney injury and renal injury, have moderate predictive ability for delayed graft function (DGF)[52]. In terms of normothermic machine perfusion, few data exist. However, the authors describe potential roles for NGAL and endothelin-1 based on a trial of 56 discarded human kidneys after 1 h of normothermic machine perfusion. In this study, Hosgoodet al[53]demonstrated that higher levels of urinary NGAL and endothelin-1 correlated with a higheri.e.worseex vivonormothermic kidney perfusion score[53]. They also note that markers of acid-base homeostasis plus lactate and aspartate aminotransferase as demonstrated in the analysis of porcine perfusate after 8 hours of normothermic machine perfusion correlated with posttransplant allograft function[54]. These studies are summarized in Table 6.
The aforementioned research demonstrates potential roles for biomarkers in adjunct with current scoring systems to help classify organs for appropriate allocation. While more research is needed, glutathione S-transferase as well as markers of tissue injury, namely NGAL, appear to show promise on this front.
Delayed graft function:Delayed graft function is a form of acute kidney injury defined by the need for renal replacement therapy in the first week after transplant. DGF is a significant transplant outcome as it is independently associated with AR and graft failure[55]. It is unknown, if biomarkers able to predict the incidence and duration of DGF early, could change management and improve outcomes.
Remarkably, biomarkers detectable within preservation solution during the peritransplant period offer diagnostic/prognostic information regarding DGF. We will review several notable studies below:
Parikhet al[46]in their study cited previously also found that base NGAL concentration was significantly higher in allografts with DGF (P= 0.004). This was also observed in post values of IL-18 (P= 0.005), and base/post perfusate liver fatty acidbinding protein levels (P= 0.029, 0.006). After multivariate adjustment as well as delta concentration (post minus base) however, these biomarkers did not significantly correlate with DGF development[46]. Similarly, in another study, van den Akkeret al[56]were able to demonstrate that NGAL at day one could predict DGFvsimmediate graft function, and also NGAL level at day 1, 4 and 7 correlate with the duration of DGF[56].
Van Smaalenet al[49]in their study analyzing extracellular histone levels found that extracellular histone concentration was significantly higher in the DGF group (median 0.70 mg/mL (IQR: 0.43 to 0.98) compared to grafts that functioned immediately [median 0.42 mg/mL (IQR: 0.07 to 0.78);P< 0.001][49]. Curiously, there was no significant difference in extracellular histone concentration in grafts with primary nonfunctionvsDGF (P= 0.437).
Van Balkomet al[57]showed that in 16 DCD kidneys in their discovery cohort, five perfusate proteins [leptin, granulocyte-macrophage colony-stimulating factor granulocyte-macrophage colony-stimulating factor (GM-CSF), periostin, plasminogen activator inhibitor-1 and osteopontin] out of 158 tested in addition to body mass index and dialysis duration predicted DGF.Viamultivariate analysis, leptin and GM-CSF were found to be the most predictive. Subsequent validation with 40 kidneys found that leptin, GM-CSF + body mass index generated a highly predictive model of DGF [AUC = 0.89 (95%CI: 0.74-1.00)], which performed better than both kidney donor risk index and DGF risk calculator (AUC = 0.55, 0.59)[57].
In a recent study from 2019, Roestet al[58]found that in 8 allografts from both DCD and DBD donors, higher levels of perfusate microRNA mir-505-3p correlated with DGF (OR = 1.12,P= 0.028). This was confirmed in a validation cohort of 40 allografts, of which 20 developed DGF (P= 0.011). Interestingly, this predictive capability held true solely for DCD allografts (P= 0.009)[58].
In addition to perfusate markers, plasma and urine-derived biomarkers have been found to predict and prognosticate DGF. These biomarkers are associated with tissue injury. As described in several studies, both urine and plasma-derived NGAL were predictive of DGF development[59-63]. These were directly compared in the review by Liet al[64]In their review of 14 studies (8 evaluating urine NGAL, 6 evaluating plasma NGAL), the composite AUC for 24 hours uNGAL was 0.91 (95%CI: 0.89-0.94) and the overall diagnostic OR for 24 hours uNGAL was 24.17(95%CI: 9.94-58.75) with a sensitivity of 0.88 and a specificity of 0.81. The composite AUC for 24 hours blood neutrophil gelatinase-associated lipocalin was 0.95 (95%CI: 0.93-0.97) with an overall diagnostic OR for 24 hours blood neutrophil gelatinase-associated lipocalin = 43.11 (95%CI: 16.43-113.12) with a sensitivity of 0.91 and a specificity of 0.86.
In another study, Banket al[65], showed that urinary tissue inhibitor of metalloproteinases-2 decrease preceded resumption of allograft function and can predict DGF resolution[65].A unique study of DGF utilized microRNA and found that levels of homo sapiens-mature form of microRNA-217 (hsa-miR-217); hsa-miR-125b along with donor age and type of donation predicted DGF with a sensitivity of 61% and specificity of 91%[66]. The aforementioned comprehensive review from Ledegancket al[21]cites 4 studies where biopsy samples of microRNA correlated with DGF. In these studies, the upregulation of miR-21-3P and miR-182-5p were measurable biomarkers[21]. Table 7 highlights these studies.
Biomarkers appear to be predictive of delayed graft function, as early as the peri-transplant period as demonstrated by perfusate markers. Urinary and plasma NGAL, among others, show promise and could augment care by changing management before the development of DGF as well as help prognosticate duration.
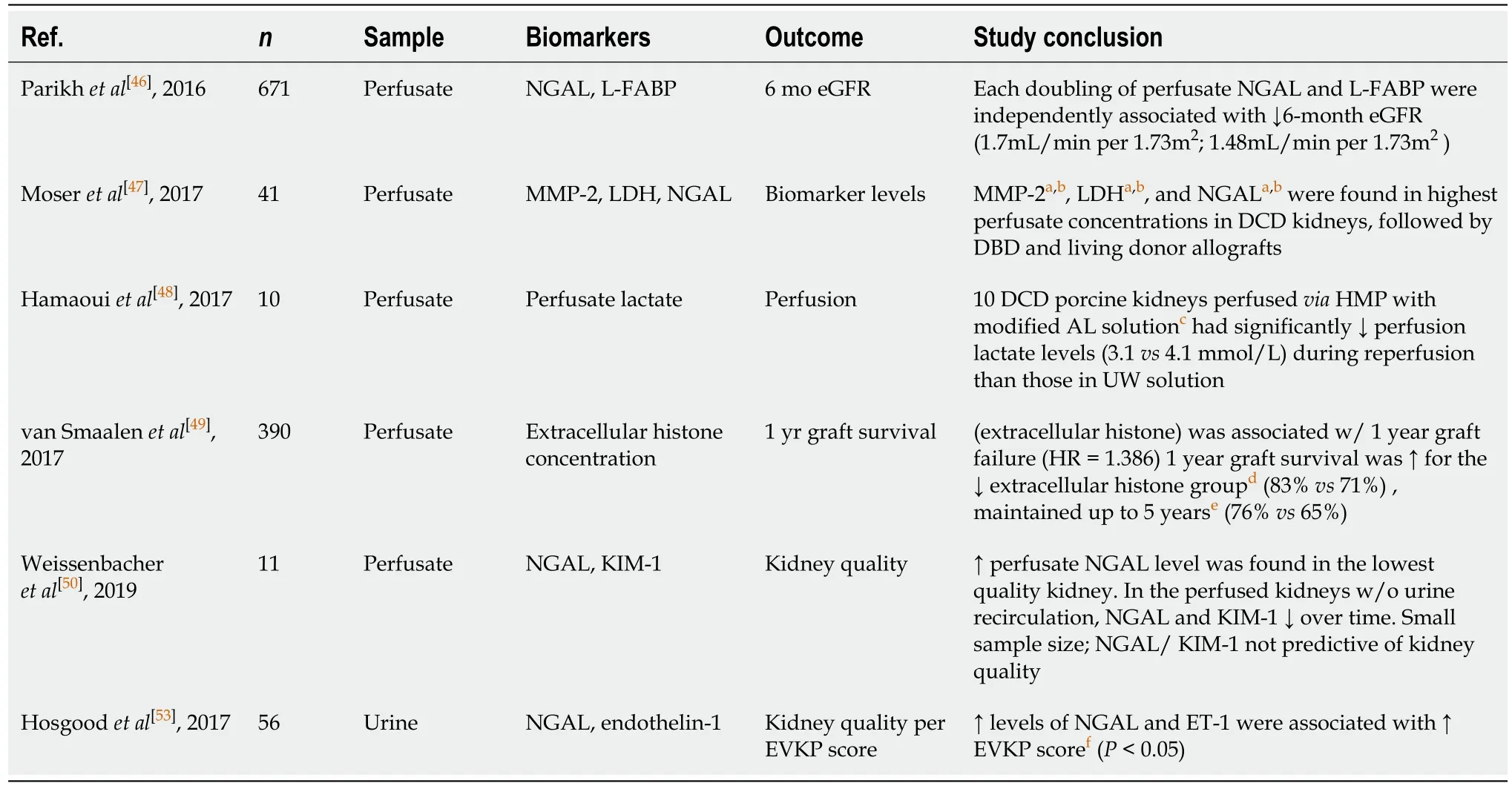
Table 6 Summary of biomarkers associated with graft quality
Cardiovascular events/mortality:Cardiovascular disease is the leading cause of death post-kidney transplantation[67]. Early detection and prediction of outcomesvianovel biomarkers is a crucial area of research. Several recent studies have explored biomarker use concerning cardiovascular outcomes. Extensive biomarker research has been conducted using KTRs from the Folic Acid for Vascular Outcome Reduction in Transplantation (FAVORIT) cohort[68-70].
Bansalet al[69]in 2016 examined 1027 KTRs from this cohort and found that each log increase in urine NGAL/creatinine independently associated with a 24% greater risk of cardiovascular events [adjusted hazard ratio (aHR) = 1.24 (95%CI: 1.06-1.45)], a 40% greater risk of graft failure [aHR = 1.40 (95%CI: 1.16-1.68)], and a 44% greater risk of death [aHR = 1.44 (95%CI: 1.26-1.65)]. Urine KIM-1/creatinine and IL-18/creatinine independently associated with a higher risk of death [aHR = 1.29 (95%CI: 1.03-1.61) and 1.25 (95%CI: 1.04-1.49 per log increase, respectively)][69].
In another study of 1184 KTRs, Parket al[70]found that higher urine alpha 1 microglobulin (A1M) (HR per doubling of biomarker = 1.40 (95%CI: 1.21-1.62), monocyte chemoattractant protein-1 (MCP-1) [HR = 1.18 (95%CI: 1.03-1.36)], and procollagen type I intact N-terminal peptide [HR = 1.13 (95%CI: 1.03-1.23)] were associated with cardiovascular events, as well as death (HR per doubling A1M = 1.51 (95%CI: 1.32-1.72); HR per doubling MCP1 = 1.31 (95%CI: 1.13-1.51);HRper doubling procollagen type I intact N-terminal peptide = 1.11 (95%CI: 1.03-1.20).
Interestingly, a study published in 2020 showed that soluble cardiac biomarker, a member of the IL-1 receptor family, which is predictive of cardiovascular mortality in patients with heart disease as well as those with chronic kidney disease, is associated with cardiovascular events [aHR = 1.31 (95%CI: 1.00-1.73);P= 0.054] and mortality [aHR = 1.61 (95%CI: 1.07-2.41);P= 0.022] in KTRs[71].
Another novel biomarker implicated in cardiovascular mortality is plasma malondialdehyde (MDA), as described in their study published in 2020. In this study, they showed that plasma MDA concentration was significantly associated with the risk for cardiovascular mortality after adjustment for potential confounders, including renal function, immunosuppressive therapy, smoking status, and blood pressure. This association was stronger in KTRs with decreased allograft function [eGFR ≤ 45 mL/min/1.73 m2; HR=2.09 (95%CI: 1.45-3.00) per 1-standard deviation increment)][72]. The findings of these studies are summarized in Table 8.
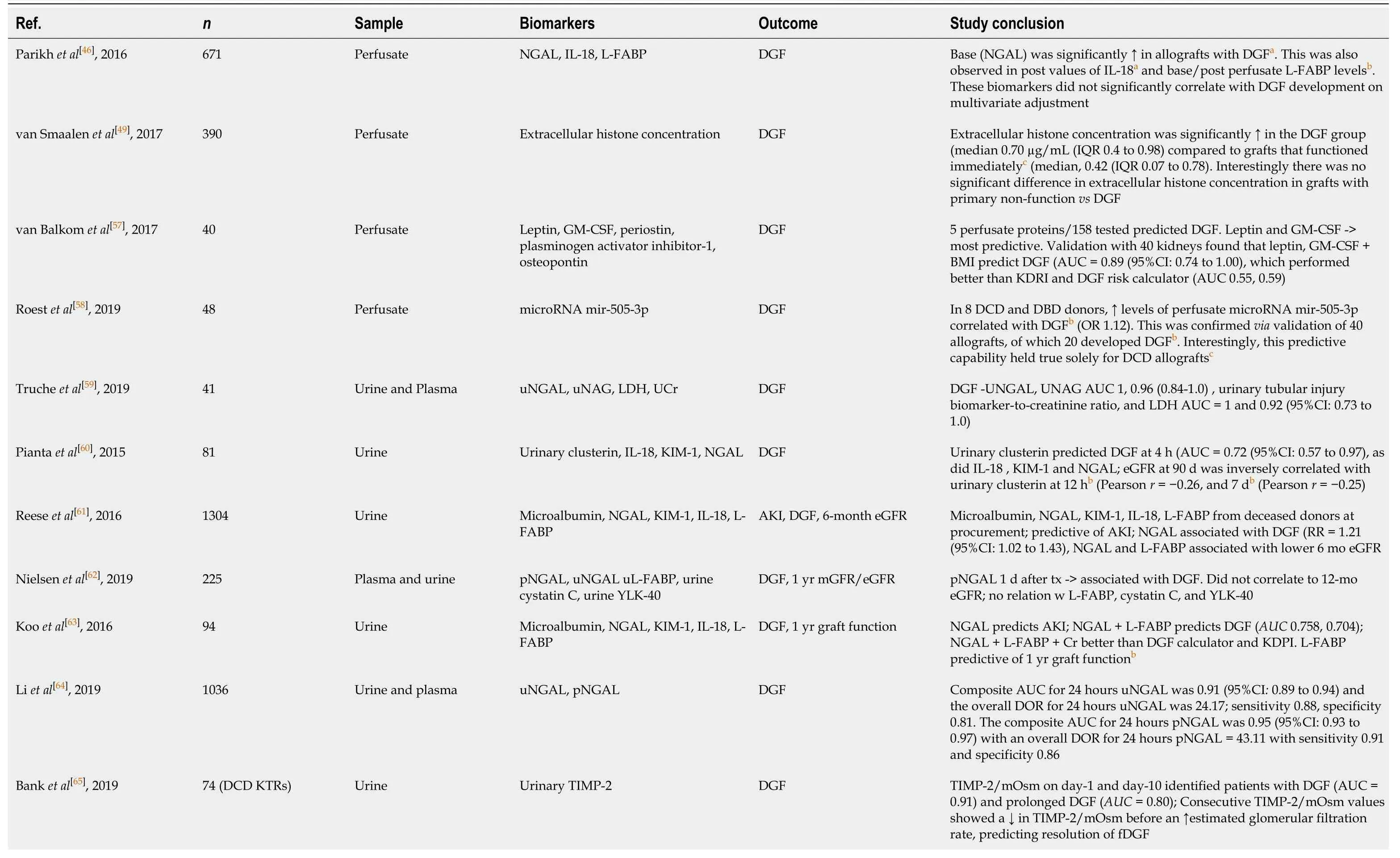
Table 7 Summary of biomarkers associated with delayed graft function
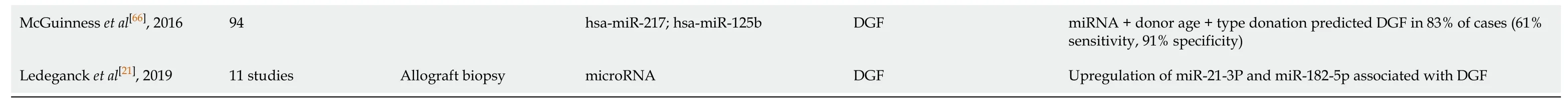
aP < 0.005 vs non-DGF allografts.bP < 0.05 vs non-DGF allografts.cP < 0.001 vs immediately functioning grafts. NGAL: Neutrophil gelatinase-associated lipocalin; IL-18: Interleukin eighteen; L-FABP: Liver fatty acid binding protein; DGF: Delayed graft function; IQR: Interquartile range; GM-CSF: Granulocyte-macrophage colony-stimulating factor; BMI: Body mass index; AUC: Area under the curve; KDRI: Kidney donor risk index; RNA: Ribonucleic acid; mir: Pre-microRNA; DCD: Deceased cardiac death donor; DBD: Deceased brain death donor; OR: Odds ratio; u: Urinary; uNGAL: Urinary neutrophil gelatinase-associated lipocalin; uNAG: Urinary N-acetyl-β-glucosaminidase; LDH: Lactate dehydrogenase; UCr: Urine creatinine; KIM-1: Kidney injury molecule-1; CI: Confidence interval; eGFR: Estimated glomerular filtration rate; RR: Relative risk; pNGAL: Plasma neutrophil gelatinase-associated lipocalin; YLK-40: Chitinase-3-like protein mGFR: Measured glomerular filtration rate; KDPI: Kidney donor profile index; DOR: Diagnostic odds ratio; TIMP-2: Tissue inhibitor of metalloproteinases 2; mOsm: Milliosmoles; fDGF: Functional delayed graft function; hsa: Homo sapiens; miR: Mature form of microRNA.
In summary, multiple biomarkers show promise in predicting cardiovascular events and mortality. Analysis of the FAVORIT cohort and others with urinary biomarkers provides some of the most robust data in favor of biomarker use to supplement current standards of care. However, more unique biomarkers utilized in cardiovascular trials, namely cardiac biomarker, as well as other unique markers of inflammation, while needing more research, may also help to prognosticate cardiovascular outcomes.
Infection:Infections, both with common pathogens or opportunistic infections, are commonplace post-transplant due to induction and maintenance immunosuppression. Infection is a crucial outcome, as it is the second leading cause of death for KTRs[67]. Interestingly, novel biomarkers may help to stratify risk after transplant.
Plasma soluble cluster of differentiation 30 at baseline and at 1 mo were demonstrated in a study of 100 KTRs to predict bacterial infection [AUC = 0.633 (95%CI: 0.501-0.765); AUC = 0.846 (95%CI: 0.726-0.966)][73]. Similarly, Sadeghiet al[74]demonstrated that patients with post-transplant cytomegalovirus (CMV) were found to have higher levels of IL-23 (8.6 ± 4.4vs8.0 ± 17;P= 0.025) and IL-23/Cr ratios (P= 0.040) than patients without CMV disease after transplantation. Moreover, they showed that pre-transplant IL-23 > 7 pg/mL increases the risk for post-transplant CMV [relative risk = 4.50 (95%CI: 1.23 to 16.52);P= 0.023][74].
Genetic polymorphisms that modify recipient infection risk can be used as biomarkers. This was demonstrated in a study of 189 KTRs where a genetic polymorphism in the Nuclear Factor kappa-light-chain-enhancer of activated B cells-94ins/delATTG increased the risk of CMV infection; survival free from CMV infection was 54.7% for ins/ins group and 79.4% for deletion carriers one year after transplantation (P< 0.0001)[75]. Table 9 highlights the conclusions of these studies.
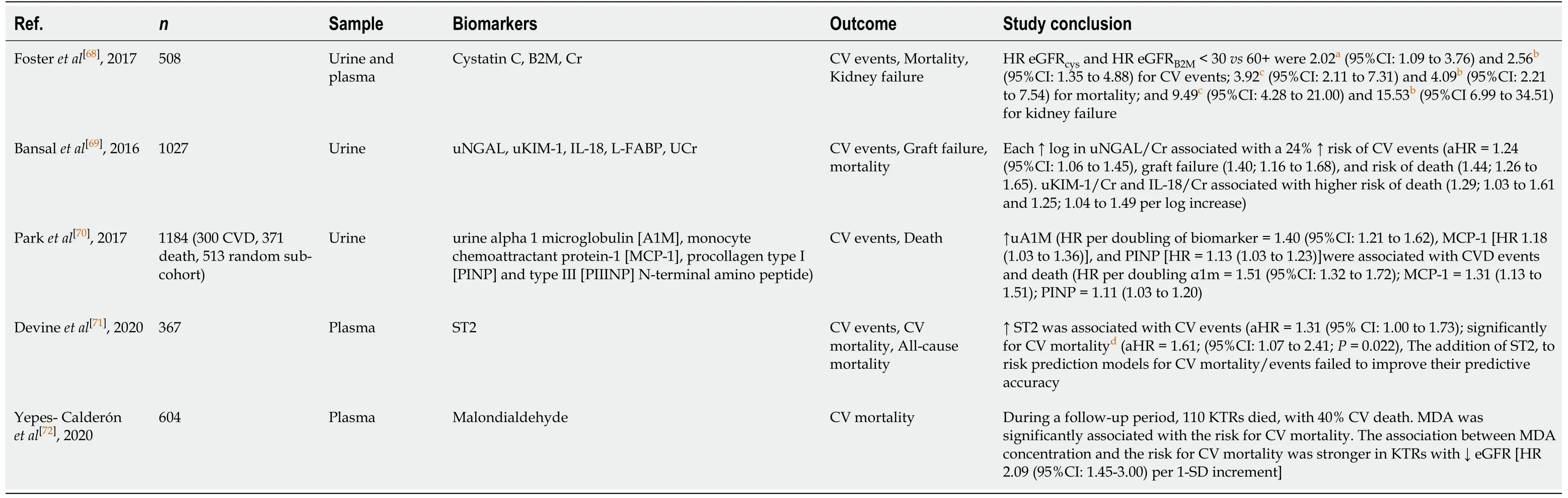
Table 8 Summary of biomarkers associated with cardiovascular events and cardiovascular mortality
An important infection in KTRs is BK polyomavirus (BK). BK virus is a doublestranded DNA virus commonly observed in the general population as a commensal organism that can cause disease including ureteral stenosis, allograft nephropathy, and graft loss in kidney allograft recipients[76]. Several studies within the past 5 years have demonstrated the utility of novel biomarkers in identifying BK virus nephropathy (BKVN).
Kimet al[77]showed in their cross-sectional study from 385 KTRs that the presence of elevated BK urinary microRNAs bkv-miR-B1-5p and bkv-miR-B1-3p in KTRs with biopsy-proven BKVN were able to significantly distinguish them from recipients without the disease (AUC = 0.989, 0.985)[77]. While promising, the study was small with only 13 KTRs with BKVN.
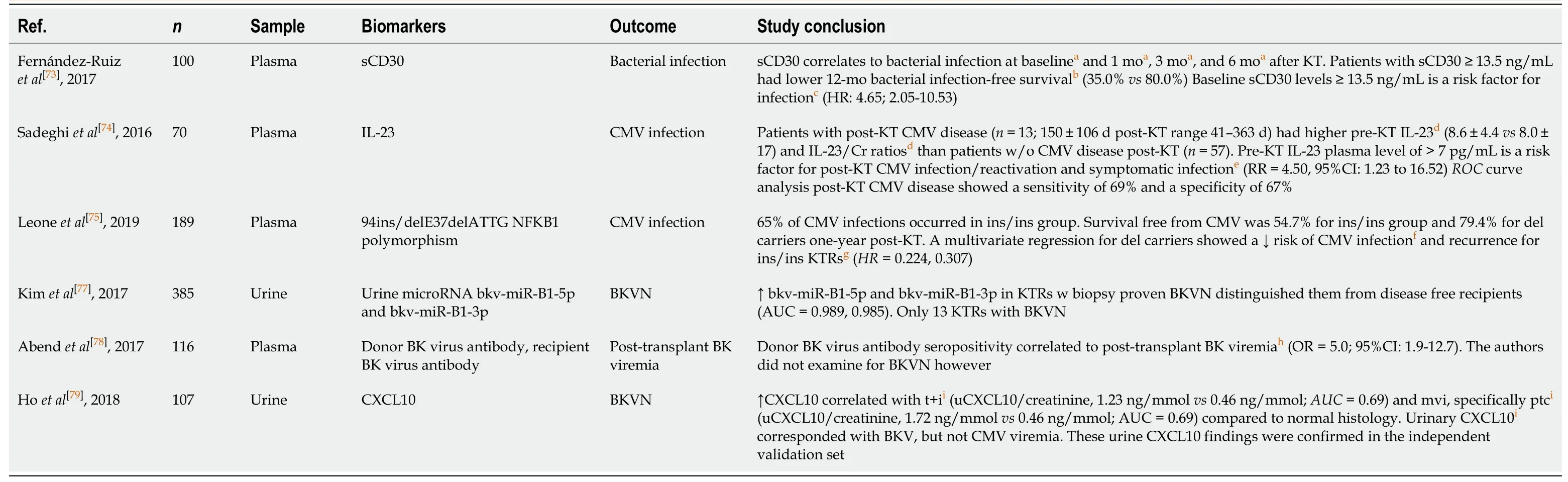
Table 9 Summary of biomarkers associated with infectious outcomes
Due to its ubiquity in the general population, the determination of the serostatus of the BK virus between donors and recipients is not standard. However, as shown by Abendet al[78]in their study of 116 deceased donor kidney transplant recipients, they found that donor BK virus antibody seropositivity correlated to post-transplant BK viremia (OR = 5.0 (95%CI: 1.9 to 12.7);P= 0.0001)[78]. The authors did not examine for BKVN however.
Serum and urine levels of CXCL10, have been demonstrated as a novel biomarkers in the context of rejection, as stated previously. In their recent study, Hoet al[79]demonstrated a further application for CXCL10 in terms of early BKVN. The authors observed elevated urine levels of CXCL10 in patients with subclinical BKVN. Elevated urinary CXCL10 occurred in the context of tubulointerstitial inflammation, peritubular capillaritis and BK viremia (allP< 0.05) They hypothesize that this could be due to either sampling errorvsearly disease preceding histologic phenomena whereby tubulointerstitial inflammation is only identifiable on a molecular level[79].
Upon its emergence in December 2019, severe acute respiratory syndromecoronavirus-2 (SARS-CoV-2) coronavirus, also known as coronavirus disease (COVID19), has been one of the most impactful pandemics in recent history. Given the high virulence and high transmissibility of SARS-CoV-2 coronavirus, much research has gone into diagnosing and prognosticating coronavirus disease. One such biomarker reported in both KTR and non-KTR literature is IL-6. Ahmadpooret al[80]postulate key mechanisms for COVID 19 infection, noting that when an adaptive immune response is blunted, particularly in populations with low naïve T cells including KTRs, innate-immune mediated inflammation can persist and lead to cytokine storm and severe illness[80]. They refer to the study by Velazquez-Salinaset al[81]who described the role of IL-6 in animal and human viral infections (vesicular stomatitis virus, influenza pneumonia, hepatitis B, lymphocyte choriomeningitis virus namely), noting that IL-6 can lead to T-cell inhibition and mitigate cell-mediated antiviral responses potentiating this effect[81]. In light of this, IL-6 is being used as a biomarker and therapeutic target. In their case report describing a patient recovering from COVID19 pneumonia, Lauterioet al[82]illustrate the use of IL-6 as a biomarker and therapeutic targetviathe monoclonal antibody tocilizumab[82]. Currently, investigators in Italy are recruiting subjects in clinical trial NCT04317092, TOCIVID-19, examining the efficacy of tocilizumab therapy.
While a smaller area of study, biomarker use to predict infection is an emerging one, particularly in the context of newly surfacing diseasee.g.COVID19. This could augment current biomarker research as learning about immune-related changes in the context of infection/infection risk will likely bolster our understanding of the immune system and have broad-ranging applications to immune responses after transplantation.
Malignancy:Malignancy is a common complication of kidney transplantation, likely related to the widespread immunologic changes related to induction/maintenance immunosuppression. The development of malignancy after transplant is a crucial outcome as it is the third leading cause of death for KTRs[67]. Biomarkers offer an opportunity for surveillance and prognostication before the development of the evident disease.
Hopeet al[83]in their study of 82 KTRs (56 with known malignancy, 26 without) found that weak NK cell activity, derived from lactate dehydrogenase and interferongamma quantification using reactive T-cell enzyme-linked immunospot, was associated with metastatic cancer, cancer-related death, or septic death [HR=2.1 (95%CI: 0.97 to 5.00)][83].
IL-27 was shown to discriminate patients with post-transplant neoplasiavsKTRs without cancer with a sensitivity of 81% specificity of 80% in a recent study[84].
In their study from 2019, Garnieret al[85]examined the pretransplant populations of cluster of differentiation forty five isoform with alternative mRNA splicing of exon (CD45RC) T cells in 89 KTRs. CD45RC expression dictates either a more regulatory (low expression) phenotype or pro-inflammatory (high expression) phenotype. Intriguingly, they found that differences in these populations predicted opposing outcomes: KTRs with a low CD4+CD45RC high population (< 51.9%) carried a 3.7 fold risk of cancer [HR = 3.71 (95%CI: 1.24 to 11.1);P= 0.019]vsthe high CD4+CD45 high population having a 20-fold higher risk of rejection [HR = 21.7 (95%CI: 2.67 to 176.2);P= 0.0004][85]. The results of these studies are illustrated in Table 10.
While the literature on biomarker predicting malignancy after transplant is limited, these studies provide some interesting insights on immunoregulation and various adverse outcomes. While age-appropriate cancer screening, dermatology follow-up, and appropriate precautions are key tenets of post-transplant care, perhaps adjunctive testing conveying malignancy risk can reiterate their importance to clinicians and patients alike.
Post-transplant diabetes:Post-transplant diabetes mellitus (PTDM) is an adverse outcome after kidney transplantation, stemming from shared disease processes leading to ESKD along with diabetogenic conditions, including immunosuppression and inflammation. PTDM is an important outcome due to decreased allograft and patient survival[86]. Biomarkers have been studied to predict the development of this condition.
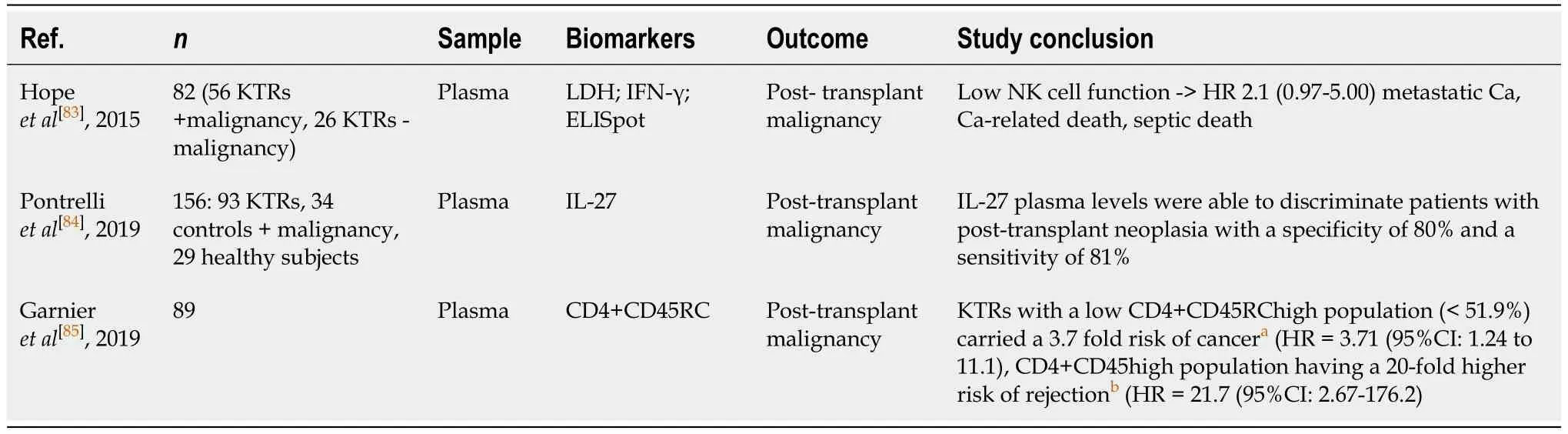
Table 10 Summary of biomarkers associated with post-transplant malignancy
In one study, Heldalet al[87]studied 20 plasma biomarkers in 852 KTRs and found 6/20 significantly associated with the development of PTDM[87].
Similar to their prior work examining MDA in the context of cardiovascular outcomes, Yepes-Calderonet al[88]found that in Cox proportional-hazards regression analyses, MDA was inversely associated with PTDM, independent of immunosuppressive therapy, transplant-specific covariates, lifestyle, inflammation, and metabolism parameters [HR = 0.55 (95%CI: 0.36 to 0.83 per 1- standard deviation increase);P< 0.01][88]. The results of these studies are illustrated in Table 11.
Diabetes after transplant is a novel area of research in terms of predictive biomarkers. A need for more sensitive assays besides our current testing is needed to help change management and prevent/treat this disease. As demonstrated by the work from Yepes-Calderónet al[88], there is overlap with certain biomarkers and pathways in terms of cardiovascular health, diabetes, inflammation and thus more research in this realm will likely have larger implications in post-transplant disease processes.
Graft survival:With the goal of kidney transplant being to restore kidney function for a recipient’s lifespan, graft survival is critical. Unfortunately, transplantation, in most cases, is a form of renal replacement therapy, as allograft failure often precedes death. Novel biomarkers provide a non-invasive strategy to help prognosticate allograft survival.
Several recent studies on novel biomarker use address graft survival[16,63,68,69,89-91]. In their examination of the FAVORIT cohort, Ixet al[90]found that in 748 KTRs, urinary injury markers A1M and MCP-1 unadjusted [HR per doubling = 1.73 (95%CI: 1.43 to 2.08); HR per doubling = 1.60 (95%CI: 1.32 to 1.93)] and adjusted [aHR per doubling = 1.76 (95%CI: 1.27 to 2.44)]; aHR per doubling = 1.49 (95%CI: 1.17 to 1.89) were associated with allograft failure[90]. Similarly, Fosteret al[68]found that in 508 KTRs from the FAVORIT cohort after multivariable adjustment, hazard ratios for eGFR measured by cystatin C and eGFR measured by beta-2-microglobulin < 30vs60+ were 9.49 (95CI: 4.28 to 21.00) and 15.53 (95%CI: 6.99 to 34.51; bothP< 0.001) for kidney failure in stable kidney transplant recipients[68].
O’Connellet al[89]found that a 13-gene gene expression profile set predicted graft loss in their study of 204 KTRs at 2 (AUC = 0.842) and 3 years (AUC = 0.844), findings that were validated in 2 public data sets[89].
In their study published in 2018, Heylenet al[92]showed that ischemia during kidney transplantation leads to DNA hypermethylation, which is a long-lasting effect seen at 1-year post-transplantation and is associated with interstitial fibrosis (P< 0.001), vascular intima thickening (P= 0.003) and glomerulosclerosis (P< 0.001) on the 1-year protocol-specified biopsies[92].
A unique study from 2019 showed that in 133 KTRs, the higher absolute number of Treg cells 1 year after transplantation was significantly associated with improved 5-year survival (92.5%vs81.4%, Log-rankP= 0.030). This finding was preserved after multivariate Cox regression analysis [hazard ratio for death-censored graft loss = 0.961 (95%CI: 0.924 to 0.998);P= 0.041], irrespective of 1-year proteinuria, and renal function[93].
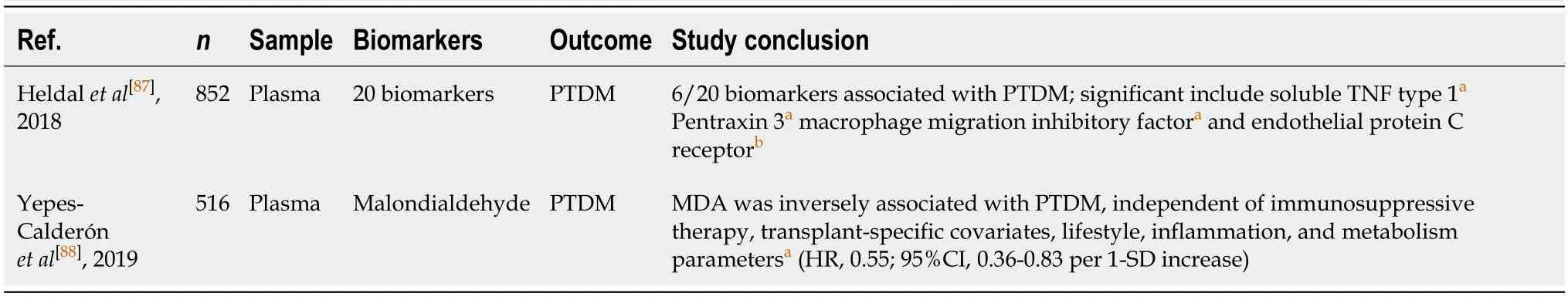
Table 11 Summary of biomarkers associated with post-transplant diabetes mellitus
Patient survival:In combination with graft survival, patient survival is one of (if not) the primary outcome(s) for kidney transplantation. Multiple studies specifically examined this in terms of cardiovascular mortality, as was mentioned previously[68-70].
One notable study utilizing 2 prospective biomarkers related to the lectin complement pathway, collectin liver-1 and collectin kidney-1 identified the following: High collectin liver-1 and collectin kidney-1 Levels at the time of transplantation were significantly associated with overall mortality in multivariate Cox analyses [HR = 1.50 (95%CI: 1.09-2.07);P= 0.013] and [HR = 1.43 (95%CI: 1.02-1.99);P= 0.038][91]. The cited studies on patient and graft survival are summarized in Table 12.
Graft and patient survival are the 2 major outcomes of interest after kidney transplantation. As previously stated, transplant across ranging allograft quality and donor/recipient characteristics is the optimal renal replacement strategy for survival. Even after the first year post-transplant, survival for KTRs is inferior to patients without ESKD. Narrowing this gap is a primary objective in transplantation. Perhaps with biomarker prediction/prognostication early (even as soon as hours after transplantation), more aggressive strategies can be undertaken to improve graft and patient survival. Moreover, they can complement current prognostication tools to help communicate impending poor outcomes with patients and prepare patients for next steps albeit graft failure and/or mortality.
FUTURE POTENTIAL BIOMARKERS
In our search, we queried a few particularly unique biomarkers/applications. In this section, we will briefly mention these findings.
In their proteomics study, Moseret al[47]described interesting findings in terms of alpha-one-antitrypsin levels across different deceased donor kidneys. They note that in a model of cardiac ischemia, alpha-one-antitrypsin was associated with antiinflammatory and myocardium protection. As alpha-one antitrypsin is a clinically available therapeutic [AralastTM(Baxter, United States), Zemeria®(CSL Behring, United States), future studies of either animal models or human subjects could be conducted[47].
In their review, De Beuleet al[51]postulated a potential biomarker role for flavin mononucleotide (FMN), a subunit of mitochondrial complex I. This molecule has been demonstrated in porcine kidney transplant models and human liver graft perfusion, as markers of mitochondrial, early allograft dysfunction and loss. This has not been studied in the context of human kidney transplantation[51].
DNA hypermethylation in the context of biomarker use in our search was a relatively unique approach, and showed promise, as mentioned earlier[92]. In a recently published review, Yanget al[94]combined multiple biomarker modalities, including urine chemokine CXCL10, clusterin, cell free deoxyribonucleic acid, methylated cell free deoxyribonucleic acid, urine protein, and urine creatinine into a comprehensive score, the Q score. In their evaluation of 601 KTRs, they were able to distinguish stable allograft function [median score = 13.1 (95%CI: 8.8-17.9] from AR [median score = 45.2 (95%CI: 40.8-57.9);P< 0.00001]. On aggregate, they found the Q score to be accurate [AUC = 9.99 (95%CI: 0.98-0.99);P< 0.00001] with a sensitivity of 95.2%, and specificity of 95.9[94]. De Vrieset al[95]in their study evaluating the tryptophan/kynurenine pathway, one associated with a pro-inflammatory state, showed that in 561 KTRs, serum kynurenine and 3-hydroxykyurenine were independently associated with allograft failure [HR = 1.72 (95%CI: 1.23-2.41)][95].
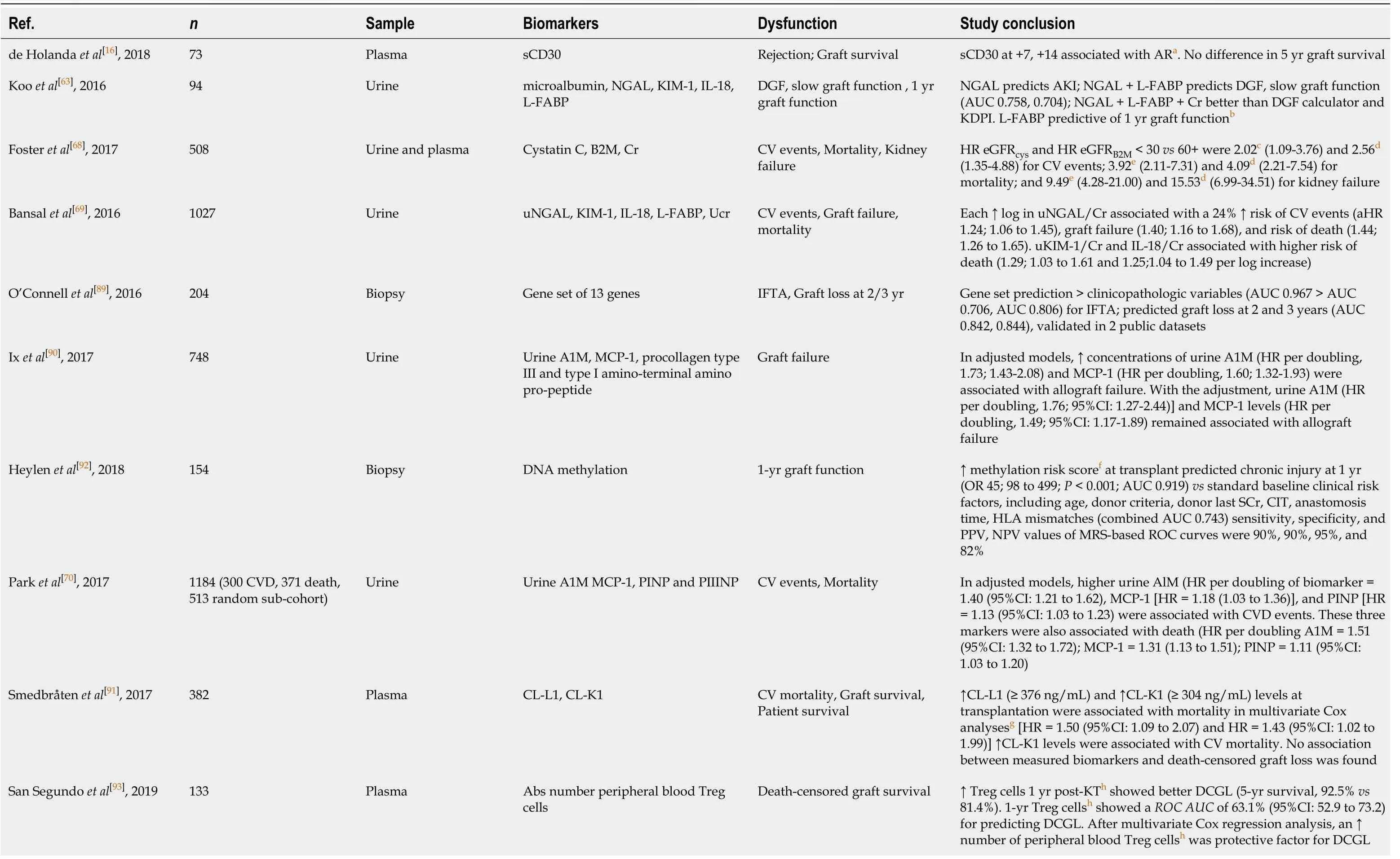
Table 12 Summary of biomarkers associated with graft survival and/or patient survival
aP < 0.05 vs grafts without rejection.bP < 0.05 vs immediate function grafts.cP < 0.05 vs eGFRcys > 60.dP < 0.005 vs eGFRB2M > 60.eP < 0.005 vs eGFRcys >60.fP < 0.005 vs low methylation risk score at transplant.gP < 0.05 vs KTRs with collectin levels below cutoff.hP < 0.05 vs KTRs with absolute number of peripheral blood Treg cells below threshold. sCD30: Soluble cluster of differentiation thirty; AR: Acute rejection; uNGAL: Urinary neutrophil gelatinase-associated lipocalin; KIM-1: Kidney injury molecule 1; IL-18: Interleukin eighteen; L-FABP: Liver fatty acid binding protein; DGF: Delayed graft function; AKI: Acute kidney injury; AUC: Area under the curve; KDPI: Kidney donor profile index; B2M: Beta-2-microglobulin; Cr: Creatinine; CV: Cardiovascular; HR: Hazard ratio; Abs: Absolute; eGFR: Estimated glomerular filtration rate; eGFRcys: Estimated glomerular filtration rate based on cysteine; eGFRB2M : Estimated glomerular filtration rate based on beta-2-microglobulin; u: Urine; UCr: Urine creatinine; aHR: Adjusted hazard ratio; IFTA: Interstitial fibrosis tubular atrophy; A1M: Alpha 1 microglobulin; MCP-1: Monocyte chemoattractant protein-1; PINP: Procollagen type I intact N-terminal peptide; PIIINP: Procollagen type III intact N-terminal peptide; DNA: Deoxyribonucleic acid; OR: Odds ratio; SCr: Serum creatinine; CIT: Cold ischemia time; HLA: Human leukocyte antigen; PPV: Positive predictive value; NPV: Negative predictive value; MRS: Methylation risk score; CI: Confidence interval; CL-L1: Collectin liver-1: CL-K1-collectin kidney-1; Treg: Regulatory T cells; KT: Kidney transplant; DCGL: 95% eath censored graft loss; ROC: Receiver operating characteristic.
Another unique study by Kostidiset al[96]from 2019 showed that urinary branchedchain amino acids over pyroglutamate and lactate over fumarate were predictive of prolonged delayed graft function (AUC = 0.85)[96].
B cell soluble factors have been implicated in autoimmune diseases such as systemic lupus erythematosus and exert the potential to be nascent biomarkers in the context of kidney transplantation. In their study published in 202, Irure-Venturaet al[97]showed that in 109 KTRs, pre-transplant B-cell activating factor (pg/mL) was significantly higher in patients with clinical ABMR during the first year (853.29 pg/mL (IQR: 765.37 to 1545.99 pg/mL) than kidney transplant without clinical rejection (594.60 pg/mL (IQR: 453.21-803.93 pg/mL) or controls (P= 0.003 andP< 0.001). This corresponded to an AUC = 0.784, with sensitivity 80%, and specificity of 73.3% for predicting ABMR within 12 months of transplantation[97].
Novel biomarker use in kidney transplantation is a vibrant area of research with multiple pioneering approaches and strategies being undertaken to discern the complex pathophysiology after transplantation and improve patient care. As these studies demonstrate, there are myriad pathways and processes implicated in deleterious post-transplant outcomes. As we have described, several nascent biomarkers derivedviamultiple biomolceular disciplines confer similar predictive properties. As we gain understanding and familiarity with biomarkers, one can hope that scientists and clinicians alike will further incorporate biomarkers in a way analogous to the multi-domain testing inherent to clinical medicine. Perhaps this approach of combining biomarkers across various domains will work synergistically to advance the field of transplant medicine.
CONCLUSION
This article summarizes emerging research about novel biomarker use in kidney transplantation. Further innovation and integration of multiple disciplines/”omics” (transcriptomics, metabolomics, proteomics) will lead to advanced biomarker discovery and implementation, which in turn will augment our current standard of care to predict and enhance post-transplant outcomes.