Accelerating the elimination of hepatitis C in Kuwait: An expert opinion
Fuad Hasan, Ahmad Alfadhli, Abeer Al-Gharabally, Mahmoud Alkhaldi, Massimo Colombo, Jeffrey V Lazarus
Abstract The hepatitis C virus (HCV) is estimated to affect 71 million people worldwide. In 2016, the World Health Organization adopted the first global health sector strategy to eliminate viral hepatitis as a public health threat by 2030. In December 2018, the European Association for the Study of the Liver, International Liver Foundation convened an expert panel to address the elimination of HCV in Kuwait. Several steps have already been taken to eliminate HCV in Kuwait, including free HCV treatment for Kuwait’s citizens, high blood safety standards, and the implementation of screening and awareness programs. The expert panel made several recommendations aimed at accelerating the elimination of HCV in Kuwait: The development of a national strategy and action plan to guide all HCV elimination activities; the formation of a coordination mechanism to support collaboration between hepatitis working committees; the prioritization of microelimination at primary, secondary or tertiary facilities, in prisons and rehabilitation centers; and ensuring the involvement of multiple stakeholders – including relevant civil society groups – in all activities. Enhanced screening and linkage to care should be prioritized in Kuwait, with the expansion of the prescriber base to primary healthcare providers and nurse practitioners to be considered. Raising awareness and educating people about HCV infection also remain essential to achieve the goal of HCV elimination. Lastly, a national HCV registry should be developed to help monitor the implementation of viral hepatitis plans and progress towards achieving national and international targets.
Key words: Awareness; Hepatitis C virus; Kuwait; Micro-elimination; Registries; Prescribers
INTRODUCTION
The hepatitis C virus (HCV) remains a public health threat in many countries, causing substantial morbidity and mortality[1,2]. While 15%-45% of the infected population become HCV free within six months without treatment, the rest develop chronic infection[3,4]. According to the World Health Organization (WHO), an estimated 71 million people have chronic HCV infection globally[3], which left untreated can lead to cirrhosis and hepatocellular carcinoma (Figure 1)[3,4]. According to the WHO global hepatitis report, in 2015, 1.75 million new HCV infections occurred[5], while in 2016, HCV led to an estimated 399000 deaths globally[3].
In response to the global burden of HCV and the associated morbidity and mortality, the WHO adopted the goal of eliminating viral hepatitis as a public health threat by the year 2030[6]. In 2016, 194 countries, including Kuwait, adopted the first global health sector strategy to combat viral hepatitis (Table 1)[6,7]. Figure 2 shows the continuum of viral hepatitis services and retention cascade, which forms the basic blocks by which these elimination targets will be achieved[6,7]. However, in 2019, only nine of the 194 countries to adopt the strategy were on track to reach the elimination targets. Kuwait, was one of the countries not on track to reach elimination targets before 2050[8].
Estimated at 1%, the prevalence of HCV in the Arabian Gulf is considered high[9]. In Kuwait, HCV remains a pressing public health issue. The country witnesses high inward migration from HCV-endemic areas[10], with 75% of the population of 2 million being expatriates[11]. Mohamoudet al[9]2016 estimate the prevalence of HCV among Kuwaiti nationals at 0.44% [95% confidence interval (CI): 0.29-0.62], rising to 1.45% (95%CI: 0.75-2.34) among the entire resident populations including nationals and expatriates.
In December 2018, the European Association for the Study of the Liver, International Liver Foundation (EILF) convened an expert panel in Kuwait[7]to discuss the country’s HCV elimination efforts and to determine urgent priorities. The expert panel was comprised of 12 local key opinion leaders and other stakeholders, including EILF board members, and gastroenterologists and experts from various health departments in Kuwait[7]. This meeting had the following four objectives: (1) To assess the current state of HCV elimination efforts in Kuwait; (2) To review the action plan of HCV elimination followed in other countries; (3) To identify factors for successes, including knowledge gaps and barriers to HCV elimination in Kuwait; and (4) To develop recommendations to advance HCV elimination efforts in Kuwait[7].

Table 1 Global health sector strategy on viral hepatitis targets

Figure 1 Natural history of hepatitis C infection. HCC: Hepatocellular carcinoma.
CURRENT EFFORTS TO ADDRESS HCV IN KUWAIT
The panel identified several targets that have been achieved in Kuwait including mandatory HCV screening for all prisoners followed by free treatment for infected individuals; free HCV treatment for citizens of Kuwait, individuals born or married to a Kuwaiti national, and stateless individuals; high blood safety standards with 100% of blood donations screened for HCV, HBV, and HIV since 1992, 1978, and 1987, respectively; and implementation of several HCV awareness and screening efforts at national and local levels[7].
The Kuwait Hepatology Association, which includes healthcare practitioners from six major hospitals of Kuwait, has proposed standards of practice for screening. According to these standards, screening should be initiated using an antibody test; in cases with a positive antibody test, confirmation should be made by PCR[10].

Figure 2 The continuum of hepatitis services and the retention cascade.
In Kuwait, direct-acting antivirals (DAAs) have been introduced as an effective and shorter HCV treatment option with limited side-effects. There are various DAA regimes available in Kuwait including Pro [Paritaprevir (75 mg)/ritonavir (50 mg) + ombitasvir (12.5 mg)], PrOD [Paritaprevir (75 mg)/ritonavir (50 mg) + ombitasvir (12.5 mg)/dasabuvir (250 mg)], SOF/LDV [sofosbuvir (400 mg) and ledipasvir (90 mg)] and DAC/SOF [daclatasvir (60 mg)/sofosbuvir (400 mg)]. Ribavirin may be administered in combination with these regimes; the decision is based on the previous therapy, the genotype, demographic profile and any comorbidities. However, the cost and accessibility of these therapies are barriers to ensuring treatment for all HCV patients. Combination of grazoprevir/elbasvir has received approval from the European Medical Agency in 2016 but is not available in Kuwait. Moreover, simeprevir/ sofosbuvir regimen is not often prescribed in Kuwait as the test for Q80K polymorphism is not available, making it challenging to prescribe for non-cirrhotic patients[10]. In Kuwait, only gastroenterologists and hepatologists can prescribe HCV treatment. Moreover, there is no national strategy or action plan for the prevention and control of HCV. These and the aforementioned barriers hinder Kuwait’s efforts to achieve HCV elimination. Based on these challenges, the panel made recommendations on how to accelerate the elimination of HCV in Kuwait[7].
RECOMMENDATIONS TO ELIMINATE HCV BURDEN IN KUWAIT
The expert panel discussed the major challenges and bottlenecks around HCV care in Kuwait and strategized priority actions to accelerate its elimination. Informed by the country’s current HCV elimination efforts and evidence of effective approaches from around the world, the panel developed seven recommendations to achieve HCV elimination in Kuwait (Figure 3)[7].
A national strategy and action plan are critical to guide and drive action for the elimination of HCV as a public health threat in Kuwait by 2025
Ambitious health goals, such as disease elimination, require sustained efforts and targeted action, with a national strategy to guide these efforts. This should be informed by the specific context, including the opportunities and challenges to eliminating HCV, and should include specific objectives and targets[7]. A plan of action plays a critical role in guiding actions towards achieving these goals, providing direction for all stakeholders and ensuring that all critical factors are addressed in parallel[12,13].
Several countries have developed and implemented strategies and action plans to guide efforts for HCV elimination[14,15]. For example, the United States National Academies, with the support of partners, developed a national strategy for addressing HCV. In the first phase of this process, stakeholders considered the feasibility of HCV elimination from a biological perspective and the specific barriers and challenges the virus presents, such as it being typically asymptomatic. In the second phase, stakeholders outlined the strategy by which elimination could be achieved; this process included establishing targets and measurable indicators to monitor the implementation of the strategy and the overall progress towards elimination[14,15]. Action plans are commonly co-developed by a core team of stakeholders who are directly working to achieve a specific health goal. However, the successful implementation of such plans is only feasible with the support and commitment of a wide range of stakeholders across the public and private sectors, from those engaged in public health approaches (e.g., policymakers, patient groups, social workers and researchers) to those involved in clinical management (i.e., multidisciplinary clinical teams)[7].
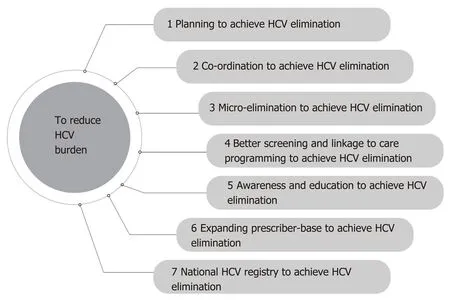
Figure 3 Steps to eliminate hepatitis C virus from Kuwait. HCV: Hepatitis C virus.
In 2016, at the first European Policy Summit on HCV, the HCV elimination manifesto was launched[16]. A key intent of the manifesto is to highlight the importance of engaging all relevant stakeholders in the development of national elimination strategies. From national working committees, including governmental, medical, and civil society representatives, to specialty care and primary care clinicians, a wide range of stakeholders must be engaged in the development of national HCV elimination action plans. At the clinical level, the management of HCV requires a multidisciplinary clinical team. Figure 4, adapted and modified from Nazarethet al[17], highlights the complex nature of HCV management and emphasizes the need for engagement and coordination across health systems. The European HCV elimination manifesto also highlights the need for integrated care pathways incorporated into national elimination strategies[16].
With respect to HCV elimination, the strategic plan informs the development of the action plan, which outlines the specific activities that will prevent new infections, effectively diagnose and treat existing infections, and ensure infection control[11]. The action plan should outline in detail the steps to achieve HCV elimination, and the roles and responsibilities of the various stakeholders. In 2018, the New York State Department of Health prepared an action plan for HCV elimination. To achieve its aims, a task force was established with five workgroups to cover the following: (1) HCV prevention; (2) HCV care and treatment access; (3) HCV testing and linkage to care; (4) Surveillance, data and metrics; and (5) Social determinants[18]. Qatar has also published a plan for the elimination of HCV, which includes primary prevention, early detection, clinical management, and continuous monitoring[19]. Evidence from Greece also highlights the importance of an action plan to ensure the effective use of resources and to enhance HCV screening and treatment[20].
Effective HCV elimination plans have also been shown to benefit the management of liver diseases more generally. Modeling of the HCV elimination plan for Italy’s Liguria region shows that the plan’s successful implementation would lead to significant savings in healthcare costs by averting the need to treat HCV associated liver-related disease[21]. A study from the Netherlands also documented the introduction of the national plan for HCV elimination. The plan provided a structural framework for the implementation of elimination activities and outlined targets related to each step in the HCV healthcare cascade: (1) Awareness and prevention; (2) Testing and diagnosis; (3) Linkage to care; (4) Access to medication; (5) Monitoring and evaluation; and (6) Social welfare and participation for all affected groups[16,22].

Figure 4 Multidisciplinary team for management of hepatitis C.
To achieve HCV elimination, tracking of operational performance across the viral hepatitis service continuum is critical. This allows for challenges and bottlenecks to be identified and addressed in a timely manner and enables stakeholders to determine when a reprioritization or refocusing of efforts is required. At the national and municipal level, Rwanda and New York, respectively, have engaged a task force to provide input to healthcare departments regarding the progress of HCV programs[17,23]. Chicago’s task force for HCV elimination has set the aim of reducing the number of new HCV transmissions to zero[24].
Cascade-of-care (CoC) monitoring is also essential to understand the effectiveness and impact of strategies and to determine improvement or deterioration in the HCV epidemic[25,26]. Defined targets and high-quality data are central to effective monitoring and informing strategic decisions about the program[26]. It is recommended that when devising national targets, including in Kuwait, these align with the goals and indicators of the WHO Global Health Sector Strategy on Viral Hepatitis 2016-2021 and the WHO regional action plan[6,7].
In summary, a strategy will be essential for guiding hepatitis elimination efforts in Kuwait while a multi-stakeholder plan of action will be required to effectively implement this strategy. For accountability, a committee or taskforce can be established to oversee the implementation of the plan and to monitor progress, in line with the predefined targets. A principal or central person leading these efforts can help to further reinforce accountability.
A coordination mechanism is critical to provide operational oversight of all screening and linkage to care programs to ensure intensive action to eliminate HCV
HCV programs at national and local levels require effective and efficient coordination across and between multiple agencies and disciplines. The key characteristics of a well-coordinated HCV mechanism include the identification of roles and responsibilities of key organizations, individuals, and working groups; quantification of the service needs (i.e., prevention, diagnosis, treatment, and care); and establishing agreed goals and targets. All of this should be accompanied by adequate investment, including in project management expertise, and be underpinned by a robust accountability framework[27].
Many countries working towards HCV elimination need to ensure proper coordination among the working committees by reporting to a national oversight committee. Such a structure promotes efficiency by minimizing the duplication of efforts with respect to planning and implementing activities to achieve HCV elimination. The US Department of Health and Human Services has made efforts to track the progress of their HCV elimination strategy. The department assisted stakeholders engaged in raising awareness to identify additional volunteers, who spread awareness among the population, local jurisdictions, and non-governmental organizations to support the attainment of the elimination target[28]. One of the goals of the US national viral hepatitis action plan specifically focuses on coordinating, monitoring, and reporting on the implementation of planned activities, highlighting the importance of coordination within efforts to achieving HCV elimination[29]. Similarly, a study from Australia in 2019 used the Delphi method to identify the critical organizational and operational elements of community-based HCV treatment models. The authors reported that integration and coordination of care and support were important from the perspective of both patients and healthcare providers[30].
As per the expert panel, several HCV screening and linkage to care programs are presently implemented in Kuwait; however, there is currently limited coordination of activities and information sharing among programs[7]. To ensure that every individual receives proper diagnosis and treatment, it is essential to have robust, coordinated linkage to care for all HCV diagnosed individuals. It is also important to differentiate between coordination mechanisms at the national level (i.e., coordination between primary, secondary, and tertiary care) and between specialists (e.g., gastroenterologists, hepatologists,etc.). Moreover, the development of an inventory of existing and proposed screening and linkage to care programs (from the national strategy/action plan) operating in Kuwait would be helpful[7]. Overall, strong coordination mechanisms are key to delivering effective large-scale HCV elimination programs. Coordination mechanisms need to include all key stakeholders (e.g., policy makers, public health professionals, multi-disciplinary clinical teams) and should prioritize the effective utilization of resources and the timely and efficient sharing of information between stakeholders[7].
Enhanced HCV screening and linkage to care programming is important to achieve HCV elimination
There are various definitions of linkage to care within the HCV literature. Saabet al[31]defined linkage to care as confirmation of HCV diagnosis by an HVC RNA test and establishment of a follow-up appointment for treatment with a specialist. Others defined linkage to care as confirming HCV by HCV RNA testing[32]or referral to a specialist and attending the first appointment within six months of diagnosis[33]. Some include both screening and attending the first appointment[34].
Generally, HCV infection is detected following an algorithm (Figure 5, adapted from Wilkinset al[35], 2015). All patients diagnosed with chronic HCV infection should then be considered for treatment. HCV treatment is chosen based upon the virus genotype, the extent of fibrosis or cirrhosis, prior therapy received, comorbid conditions, and adverse effects. However, the principal aim of all therapies is to reduce the complications and mortality associated with HCV[35].
The development of an inventory of available data to examine the viral hepatitis care cascade (Figure 2) and to determine areas of drop-out is key for improving linkages to care and guiding actions to specifically address bottlenecks and challenges[36]. Monitoring the prevalence of HCV is key to enable effective and efficient resource allocation and utilization. Adequate resource allocation to health care providers as well as diagnostic laboratories and hospitals is critical to enable screening and treatment. Screening and treatment capacity depend upon the resources available in the country[37,38]. It is especially critical that available resources are utilized in the most effective and efficent way.
As part of Rwanda’s initiative to eliminate HCV the country has developed a fiveyear plan which includes several activities aimed at enhancing screening and linkage to care[23]. The plan includes an expansion of the workforce of general practitioners, nurses, and laboratory personnel, a reduction in the price of DAAs, and the provision of training to the key individuals and those engaged in conducting awareness campaigns. Through these activities, it is estimated that more than 4 million people will be screened and around 112000 adults treated, averting 10638 new infections, and more than 35000 premature deaths[23].
In certain population groups, such as incarcerated individuals and people who inject drugs (PWID), timely screening and linkage to care can be challenging. For example, in many prison hospitals HCV treatment is provided to all new positive cases in order to prevent re-infection, a concept known as “treatment as prevention[39].” However, once released from prison, treatment is generally discontinued due to a lack of follow-up[39]. For these types of population groups there is a need to have multiple, parallel approaches for identifying and linking individuals to programs, such as drug harm reduction services for PWID[40].

Figure 5 Algorithm for hepatitis C virus diagnosis. HCV: Hepatitis C virus.
Modeling studies can be useful to quantify the screening targets and resources required to meet national and international goals. For example, a recent publication for Malaysia modeled a stepwise approach to scale up HCV screening in order to reach the WHO 2030 targets. The model estimated screening of < 1 million PWID per year between 2018-2026, before expanding to the general population, with a total of 6 million people screened between 2018-2030. The total cost of screening was estimated at $58 million[41]. Zuckermanet al[42], suggested that there should be established recommendations for screening and diagnosis of HCV to help overcome disparities in diagnosis and linkages to care. A modeling study on the impact of enhanced screening and treatment on HCV in the US estimated a significant reduction in HCV-related deaths. Increasing treatment four-fold was projected to result in an 80% reduction in HCV prevalence by 2025, with significant reduction in liver outcomes including cirrhosis and hepatocellular carcinoma[43].
To meet the WHO HCV elimination targets, it is essential to implement successful prevention interventions, outreach screening programs, improve infection control, design initiatives for high-risk subpopulations, such as PWID, and link these programs to other harm reduction services, and conduct extensive screening for HCV followed by treatment[44].
Micro-elimination programs can be a key element of the national strategy and action plan to fast-track HCV elimination in high-risk populations
The micro-elimination approach focuses on eliminating HCV in high-risk subpopulations and can be applied in settings such as hospitals, prisons, and rehabilitation centers[37]. Micro-elimination enables “quick-wins” in a long-term national plan by eliminating HCV in high-risk groups. The approach can be initiated taking geographic areas, sub-populations, or age-cohorts into consideration. As done in screening programs, modeling studies can be utilized to identify and estimate the impact of HCV infection in high-risk regions or population groups[37].
Lazaruset al[45,46](2017 and 2018) propose that target groups suitable for microelimination include patients with advanced liver disease, hemophilia and/or engaged with drug treatment units, prisoners, children, migrant communities from high prevalence regions, PWID in networks, men who have sex with men, and generational cohorts of high prevalence and geographically defined areas. Hemodialysis patients should also be assessed for HCV infection[47]. People visiting barber shops, beauty salons, tattoo parlors, and fitness centers (the latter because of injectableable steroid use) should also be assessed as per the expert panels recommendations[7]. Adults born between 1945 and 1965, known as “baby boomers”, are also considered a cohort with a high prevalence of HCV and should be screened at least once for HCV[33]. In the US, the prevalence of HCV is expected to be five-fold higher in baby boomers compared to other adults as they are thought to have become infected during its outbreak between 1960-1980[48]. Crowleyet al[49]reported screening of prisoners in an Irish prison to be a useful case finding model that enabled the diagnosis of new cases and facilitated linkage to HCV care. Currently, in Kuwait, all prisoners are screened for HCV infection and, if positive, provided free treatment[7].
The prevalence of HCV is significantly higher in PWID than in the general population[50]. Analysis from the US highlighted the need for PWID to be universally screened for HCV in order to achieve elimination[43]. In the Netherlands, microelimination has been at the forefront of HCV elimination efforts, with PWID a key population group screened and linked to care. This pragmatic and efficient approach has taken the country closer to the goal of HCV elimination[22]. In Iceland, the universal HCV treatment program has been combined with an additional screening of PWID in order to achieve the national HCV elimination targets[51].
To accelerate HCV elimination in PWID, the micro-elimination program should adhere to recognized best practice as follows: (1) Access to sterile equipment used for injecting (this would form a part of a large-scale harm reduction program); (2) Testing of volunteers after a regular time period (e.g., 12 mo); and (3) Following up individuals who reported having a high-risk injection episode[7]. Micro-elimination of HCV in PWID involves expanding and integrating harm reduction services to HCV screening and treatment[52]. In Australia, DAAs were approved for use through the Pharmaceutical Benefits Scheme, which significantly boosted the treatment uptake in marginalized communities, including PWID[53].
Micro-elimination programs are also associated with numerous challenges. Targeting vulnerable and often disenfranchised populations, such as PWID, homeless people, and prisoners, is resource intensive and poses particular monitoring and linkage to care-related challenges attributable to inaccessibility of those infected, lack of HCV knowledge, impaired mental health, drug-phobia, financial constraints, and a lack of motivation to be screened and treated. Moreover, these programs require multiple visits and follow-up steps, which require additional staff. In some contexts, this may also require new or different models of service delivery[54,55]. Microelimination programs need to utilize existing resources and services to overcome these challenges.
Micro-elimination plans should incorporate realistic, annual goals for screening and treatment. As with national action plans, multiple stakeholders, including government officials, health service providers, and civil society groups, should be involved in the design of the micro-elimination programs. Progress should be monitored and reported on a regular basis[37]. Where national action plans are hampered by political and logistical challenges, micro-elimination programs can help to build momentum by delivering tangible results quickly and efficiently[56].
Overall, the micro-elimination of HCV in high-risk populations in Kuwait should be considered as an essential component of the overall elimination strategy. Involvement of multiple stakeholders, volunteers, and healthcare practitioners is essential. Microelimination efforts should be monitored closely to ensure they are contributing to the boarder goal of HCV elimination in the general population.
Expanding the prescriber-base to achieve HCV elimination
Evidence supports the expansion of the HCV treatment prescriber base, which in Kuwait is currently restricted to gastroenterologists and hepatologists, to include primary care providers and nurse practitioners. A non-randomized, open-label clinical study from the US District of Columbia determined that HCV treatment provided by non-specialists (nurse practitioners and primary care physicians) was as safe and effective as treatment provided by specialists[56]. Nazarethet al[17]also support the use of nurse practitioners to increase the prescriber-base to support HCV elimination efforts. Furthermore, to increase treatment capacity Korenet al[57]reported utilizing clinical pharmacists for HCV treatment, which resulted in high rates of sustained virologic response (95.1%).
Evidence suggests that with adequate planning, training, and capacity building, non-specialists can provide treatment comparable to that given by specialists. Kuwait can consider expanding the prescriber base to accelerate HCV elimination efforts. Such a decision will require careful consideration which should be taken in consultation with all relevant stakeholders within the country.
Increased awareness and education on HCV will help to accelerate eradication efforts
Lack of awareness around HCV is one of the major challenges in achieving elimination. A significant number of people living with HCV are unaware of the viral infection and global knowledge of the disease in the general population is low[58,59]. Training and educational courses for health care providers are essential to ensure they have the most up to date knowledge on standards of care and novel approaches for HCV elimination[17,55]. Public information and awareness campaigns are key to address misconceptions about HCV, its modes of transmission, and the treatment options[60].
Georgia and Egypt, which have both agreed specific targets for the elimination of HCV, have implemented advocacy, awareness, and education activities as part of their elimination programs[59]. Such efforts can focus on the general population or specific population groups such as potential targets for micro-elimination. Novel approaches to HCV awareness creation and education may be required for specific population groups, such as PWID. Integration of awareness creation efforts with other social services or through civil society groups working with the affected population may be beneficial[61,62].
Development and implementation of a national HCV registry is key for guiding elimination efforts
HCV registries provide vital information to monitor programs and to track progress towards national and international goals[63]. Several countries, including Taiwan and the US, have conducted clinical trials to develop national HCV registries[64,65]. In the US, the Clinical Case Registries (CCR) consist of two registries, CCR: HIV and CCR: HCV. Both are designed to provide population-based data on Veterans Affairs patients infected with HIV or HCV, which share common risk factors[66]. Rizket al[67](2019) highlight how disease registries enable follow-up and allow identification of barriers to care, with innovative solutions such as co-located HIV and HCV clinics being developed as a result.
A national HCV registry can guide strategic decision making at national and local levels. Registries support the monitoring of programs and allows stakeholders to review and revise strategies and plans based on the evolving context (e.g., changes in HCV epidemiology) and changing priorities (e.g., transition from micro-elimination to a national program)[7]. They play a vital role in the treatment of hard to reach population groups that present additional challenges related to tracking and followup[68]and assist in assessing the rate of diagnosis for HCV. Central disease registries also provide opportunities for assessing screening efforts and identifying future opportunities for expansion[69].
In the Middle East, there is a lack of reliable information regarding the prevalence of HCV infection. In Kuwait, determining an accurate HCV prevalence is further complicated by the constant migration of expatriates, a proportion of whom are from HCV-endemic regions[10]. To address this challenge, the Ministry of Health can seek to upgrade the medical record systems to capture adequate information and recruit specialists for processing and analyzing data. Registries can also be used to support real word studies, as done in Germany, to determine the effectiveness and safety of different HCV treatments[70].
An HCV registry is an essential source of information to guide strategic decision making and track the implementation of action plans. The data can also be used to review and revise strategies and plans as the context evolves or new opportunities or challenges emerge. The HCV registry should be designed to incorporate relevant indicators in line with the WHO HCV elimination strategy.
CONCLUSION
Concerted action can substantially reduce the high prevalence of HCV in Kuwait. To eliminate HCV in the country, key stakeholders have followed the WHO strategy and identified the major challenges and opportunities for advancing progress. Informed by these challenges, an expert panel developed seven recommendations to accelerate the elimination of HCV as a public health threat in Kuwait: (1) Developing and implementing a national strategy and action plan; (2) Establishing a coordination mechanism between viral hepatitis working committees; (3) Following a microelimination approach; 4) Enhancing screening and linkage to care; (5) Expanding the prescriber base; (6) Raising awareness and educating the population; and (7) Developing a national HCV registry.
ACKNOWLEDGEMENTS
The authors would like to thank all the experts who participated in the meeting.
 World Journal of Gastroenterology2020年30期
World Journal of Gastroenterology2020年30期
- World Journal of Gastroenterology的其它文章
- Comment on pediatric living donor liver transplantation decade progress in Shanghai: Characteristics and risks factors of mortality
- Risk prediction platform for pancreatic fistula after pancreatoduodenectomy using artificial intelligence
- Predictive model for acute abdominal pain after transarterial chemoembolization for liver cancer
- Vedolizumab for ulcerative colitis: Real world outcomes from a multicenter observational cohort of Australia and Oxford
- Role of minimally invasive surgery for rectal cancer
- Differential diagnosis of diarrhoea in patients with neuroendocrine tumours: A systematic review
