Effect of weekend admission on geriatric hip fractures
Abstract
Key Words:Hip fracture; Weekend admission; Time to surgery; Morbidity; Mortality;Complication
INTRODUCTION
In the United States,more than 300000 people aged 65 and older are hospitalized for hip fractures annually[1].With the aging population in the United States,the incidence of hip fractures will continue to rise and further the burden on the medical system.Despite hip fractures accounting for less than 20% of all osteoporotic fractures,they cause the majority of fracture-related mortality in patients over the age of 50[2].The high mortality rate associated with hip fractures is often due to the pre-existing medical comorbidities of the patients that sustain these injuries.
Over 98% of patients with hip fractures receive surgical treatment to stabilize the fracture and allow for early mobilization[3].A multitude of studies have found predictive factors for mortality after surgery.Most risk factors,such as age and the presence of various medical comorbidities,are non-modifiable in the perioperative period.Optimization of medical conditions and a multi-disciplinary approach to perioperative care are thus incredibly important in the geriatric patient who sustains a hip fracture.
Another potential non-modifiable risk factor for geriatric hip fractures is day of presentation.The care discrepancy for patients presenting to a hospital on the weekend relative to the work week is well documented[4,5].With respect to hip fractures,however,the literature is not so clear.There is no consensus regarding the presence of a so-called “weekend effect” for geriatric hip fractures[6-9].Much of the literature on this topic involves large database studies.While these studies allow for a large number of patients,they are accompanied by all of the inherent limitations of database studies.
This study sought to determine the effects,if any,of weekend admission on care of geriatric hip fractures treated operatively at a large tertiary care hospital.Its findings would contribute to the debate that exists in the literature and allow orthopaedic surgeons to have frank discussions with patients and their family members with respect to risk and prognosis of operative intervention for hip fractures.
MATERIALS AND METHODS
Data acquisition
A retrospective chart review of geriatric hip fractures treated operatively at our large,tertiary care institution from 2015-2017 was performed.Patients who presented to the hospital from 12:00 AM Monday to 11:59 PM Thursday comprised the weekday cohort.Patients who presented to the hospital from 12:00 AM Friday to 11:59 PM Sunday comprised the weekend cohort.Holidays were considered weekend days,and thus patients who presented to the hospital on a holiday were included in the weekend cohort.Due to the lack of availability of both unscheduled operating room time and peri-operative services (such an echocardiography),Friday was included as a weekend day.On weekends and holidays,staffing levels at the study hospital are decreased relative to weekdays.There is one on-call orthopaedic surgeon,a medical optimization physician,and two physical therapists that cover the orthopaedic service on these days.Because the focus of this study was geriatric hip fractures,patients below 50 years of age were excluded from the study.Only pathologic fractures that were due to a malignancy were excluded.Only the hospital admission in which the hip fracture treatment occurred was reviewed.
Outcome measures
Primary outcome measures were length of stay (LOS),blood transfusion rate,complication rate,and mortality rate.Secondary outcome measures were time from emergency department (ED) arrival to medical optimization,time from medical optimization to surgery,and time from ED arrival to surgery.Medical optimization refers to the process in which an internal medicine physician evaluates pre-operative patients.He or she determines if patients require additional workup/interventions prior to surgical intervention.Complications reviewed can be viewed in Table 1.
Statistical analysis
Age between cohorts was compared using a Wilcoxon rank sum test.Sex,American Society for Anesthesiologists (ASA) classification distributions,surgical procedure distributions,LOS,time from ED arrival to medical optimization,time from medical optimization to surgery,time from ED arrival to surgery,transfusion rate,complication rate,and mortality were analyzed using a Fisher’s exact test.For complication rate and mortality rate,comorbidities were analyzed with logistic regression models.Comorbidities analyzed were diabetes mellitus,hyperlipidemia,chronic kidney disease,cardiac disease,respiratory disease,depression,dementia,and cancer.Multivariate logistic regression was then performed with the comorbidities that demonstrated association with the outcome measure in question.An alpha level of 0.05 was utilized as the cutoff point for significance for all data analysis.All statistics were performed by Michael Silver from Maimonides Medical Center,who is the institution’s biostatistician.
RESULTS
A total of 690 geriatric hip fractures were identified from 2015-2017.Three hundred and eighty-eight (56.2%) of the patients presented to the hospital from 12:00 AM Monday to 11:59 PM Thursday,and comprised the weekday cohort.Three hundred and two (43.8%) of the patients presented to the hospital from 12:00 AM Friday to 11:59 PM Sunday or on a holiday,and comprised the weekend cohort.Demographic information can be viewed in Table 2.There was no difference in age,gender,or ASA distribution between the two cohorts.There was no difference in medical comorbidities between the two cohorts,with the exception of hyperlipidemia being more prevalent in the weekday cohort (P= 0.0014) and respiratory disease being more prevalent in the weekend cohort (P= 0.0257).Procedures performed for hip fracture were hemiarthroplasty,total hip arthroplasty,long cephalomedullary nail,short cephalomedullary nail,cannulated screw fixation,and sliding hip screw.There was no difference in the distribution of procedures performed between the two cohorts(Table 3;P =0.8309).
Comparison of primary and secondary outcome measures between the weekday and weekend cohorts is shown in Table 4.Median LOS was the same in the weekend cohort (5 d) as in the weekday cohort (5 d;P =0.2734).Transfusion rate was also similar between the two cohorts (P =0.9325).Mortality rate was not different between the cohorts either (P =0.3460).This remained true when multivariate logisticregression was performed,taking medical comorbidities into account (P =0.4530).Complication rate was significantly higher in the weekend cohort (13.3%) compared to the weekday cohort (8.3%;P =0.044).This,too,remained true when multivariate logistic regression was performed,taking medical comorbidities into account (P =0.0273).In terms of secondary outcome measures,median time from ED arrival to medical optimization was significantly longer in the weekend cohort (22.7 h) than the weekday cohort (20.0 h;P =0.0015).Likewise,median time from medical optimization to surgery was significantly longer in the weekend cohort (13.9 h) than in the weekday cohort (10.8 h;P =0.0172).Finally,median time from ED arrival to surgery was significantly longer in the weekend cohort (42.7 h) than the weekday cohort (32.5 h;P< 0.0001).
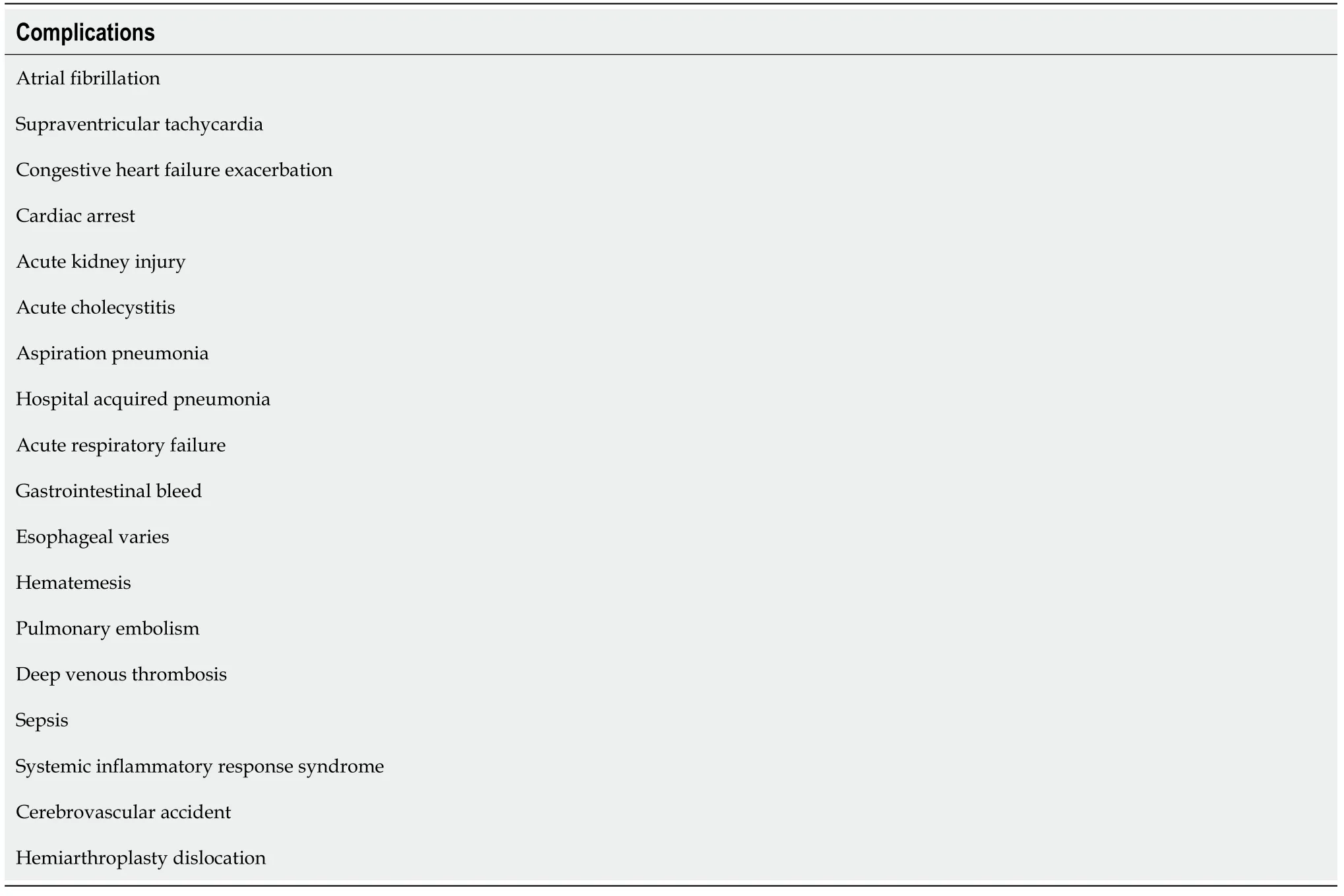
Table1 Complications included in the analysis of complication rate for hip fracture patients
DISCUSSION
This study found that the weekend effect is a real phenomenon with respect to geriatric hip fractures at a large,tertiary care center.Complication rate was significantly higher for hip fracture patients presenting to the hospital on the weekend.Time from ED arrival to medical optimization,time from medical optimization to surgery,and time from ED arrival to surgery were all significantly longer for patients presenting to the hospital on a weekend relative to a weekday.LOS,transfusion rate,and mortality rate,however,were not affected by day of presentation.
The difference in median time from ED arrival to surgery between the weekday and weekend cohorts was 10.2 h.Both time from ED arrival to medical optimization (2.7 h difference) and time from medical optimization to surgery (3.1 h difference)contributed to this delay,and all three differences between the weekend and weekday cohorts were statistically significant.Both medical and surgical physicians should therefore be cognizant of potential delays that may occur on the weekends,and should aim for expedient medical optimization and subsequent surgical intervention for hip fracture patients.
数据无声,却胜于雄辩。改革开放40年来,我国实现了从高度集中的计划经济体制到充满活力的社会主义市场经济体制的伟大历史转折,经济前行既快、又稳、更好。
The disparity in outcomes for patients presenting to the hospital on a weekend day relative to a weekday has been thoroughly described.Diagnoses associated with increased mortality rates in the presence of weekend admissions include acutecerebrovascular accident,ruptured abdominal aortic aneurysm,pulmonary embolism,duodenal ulcer,and ischemic heart disease[5,10-13].There are multiple theories as to why the “weekend effect” occurs,including on-call staff being less familiar with treatment protocols,decreased staffing levels,reduced resources,surgical technicians covering cases outside of their expertise,and unavailability of specific implants.These variables differ across health care systems and across institutions.

Table2 Demographics and comorbidities for the weekday and weekend cohorts.Median and interquartile range are given for age
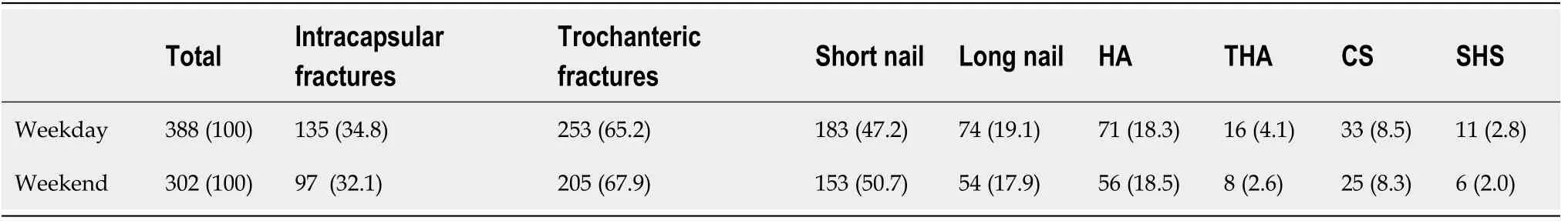
Table3 Breakdown of procedures performed for the weekday and weekend cohorts,n (%)
With respect to hip fractures specifically,there is no consensus about the presence of a “weekend effect”.It has been reported that weekend admission of isolated hip fractures has no effect on medical complications,surgical complications,delay to surgery,length of stay,re-operation rate,or mortality rate[10,14-18].A study conducted using the National Inpatient Sample Database to determine predictors of inpatient mortality following surgical treatment for hip fracture found that day of admission was not a predictor,but that having surgery on day 2 or later was[19].Another National Inpatient Sample Database study found that weekend admission of hip fractures was associated with lower mortality rates and shorter hospital stays,but no difference was noted in complication rates[9].A Norwegian study of over 61000 hip fractures found that day of admission did not affect 30 d mortality rate,but that early morning admissions and weekend discharges were associated with an increased 30 d mortality rate[20].A single-institution retrospective review of femoral neck fractures found thatsurgeries performed on weekends were associated with an increased in-hospital mortality rate,but not an increased complication rate[21].Another retrospective study from a single institution found that weekend admission of intracapsular femoral neck fractures was not associated with an increased complication rate[22].Extracapsular fractures,however,have been shown to be associated with an increased complication rate when patients present on a weekend[9].A variety of studies have found that weekend or holiday admission is associated with increased mortality rates of geriatric hip fractures[7,8].Specifically,Clague and colleagues found that Friday admission was associated with an increase in 90 d mortality after fixation of hip fracture[23].Additionally,weekend admission of hip fractures has been associated with delays to surgery by a number of authors[24-27].

Table4 Comparison of the primary and secondary outcome measures between the weekday and weekend cohorts
The findings presented here are impactful for a variety of reasons.Time to surgery has been shown to have a significant impact on complication rate for operative hip fractures[28].Here,the oft-quoted ideal time to surgery for hip fractures of 48 h was achieved in both the weekday and weekend cohorts (viathe median values).A decrease in time to surgery of over 10 h,however,can be clinically significant in terms of patient pain management and early mobilization.Additionally,the weekend cohort had an increased in-hospital complication rate.Post-operative complications have been found to increase one-year-mortality in hip fracture patients[29].Surgeons must be aware of the increased morbidity that may accompany their hip fracture patients simply by virtue of the day they arrive to the hospital.Furthermore,interventions to reduce this increased morbidity (such as increased staffing or changes in hospital protocols) should be undertaken where possible.
This study is not without limitations.It was a retrospective study,and only the hospital stay in which operative intervention occurred was reviewed.Additionally,it was a single-institution study and thus the findings here may not be entirely generalizable to the population of hip fracture patients nationwide.Differences in institutional staffing schemes,operating room organization,and protocols may have substantial impacts on the effects of weekend hip fracture admission.These factors also likely account for the variety of findings reported in the literature.
CONCLUSION
We have found that,at a single tertiary-care institution,weekend hip fracture admission is associated with an increased complication rate,and increased times from ED arrival to medical optimization,medical optimization to surgery,and ED arrival to surgery.This information is of utility to surgeons,optimization physicians,and patients alike.Additionally,it may be of use to hospitals and their administrators to guide resource and personnel allocation,so that delays to surgery and in-hospital complications can be minimized.
ARTICLE HIGHLIGHTS
Research background
In the United States,more than 300000 people aged 65 and older are hospitalized for hip fractures annually.Despite hip fractures accounting for less than 20% of all osteoporotic fractures,they cause the majority of fracture-related mortality in patients over the age of 50.A potential non-modifiable risk factor for geriatric hip fractures is day of presentation.The care discrepancy for patients presenting to a hospital on the weekend relative to the work week is well documented.With respect to hip fractures,however,the literature is not so clear.The purpose of this study was to determine the effects,if any,of weekend admission on care of geriatric hip fractures treated operatively at a large tertiary care hospital.
Research motivation
There is currently no consensus regarding the presence of a so-called “weekend effect”for geriatric hip fractures.Much of the literature on this topic involves large database studies.While these studies include a large number of patients,they are accompanied by all of the inherent limitations of database studies.This study sought to determine the effects of weekend admission on the morbidity,mortality,and times to medical optimization and surgery for geriatric hip fractures at a single,tertiary care institution.
Research objectives
In this study,we compared length of stay,blood transfusion rate,complication rate,mortality rate,time from emergency department arrival to medical optimization,time from medical optimization to surgery,and time from emergency department arrival to surgery between hip fracture patients who presented to the hospital on a weekday and those who presented on a weekend.
Research methods
A retrospective chart review of geriatric hip fractures treated operatively at our large,tertiary care institution from 2015-2017 was performed.Patients who presented to the hospital from 12:00 AM Monday to 11:59 PM Thursday comprised the weekday cohort.Patients who presented to the hospital from 12:00 AM Friday to 11:59 PM Sunday comprised the weekend cohort.Holidays were considered weekend days,and thus patients who presented to the hospital on a holiday were included in the weekend cohort.
Research results
There were no statistically significant differences in length of stay (P =0.2734),transfusion rate (P =0.9325),or mortality rate (P =0.3460) between the weekend and weekday cohorts.Complication rate was higher in patients who presented on a weekend compared to patients who presented on a weekday (13.3%vs8.3%;P =0.044).Time from emergency department arrival to medical optimization (22.7 hvs20.0 h;P =0.0015),time from medical optimization to surgery (13.9 hvs10.8 h;P =0.0172),and time from emergency department arrival to surgery (42.7 hvs32.5 h;P<0.0001) were all significantly longer in patients who presented to the hospital on a weekend compared to patients who presented to the hospital on a weekday.
Research conclusions
Geriatric hip fracture patients that presented to the hospital on a weekend experienced a higher complication rate and longer times from emergency department arrival to medical optimization,from medical optimization to surgery,and from emergency department arrival to surgery.
Research perspectives
The findings of this study are of utility to Orthopaedic surgeons,optimization physicians,and patients alike.Additionally,they may be of use to hospitals and their administrators to guide resource and personnel allocation,so that delays to surgery and in-hospital complications can be minimized.
 World Journal of Orthopedics2020年9期
World Journal of Orthopedics2020年9期
- World Journal of Orthopedics的其它文章
- Supernumerary brachioradialis - Anatomical variation with magnetic resonance imaging findings:A case report
- Factors predisposing to thrombosis after major joint arthroplasty
- Length unstable femoral fractures:A misnomer?
- Screening for scoliosis - New recommendations,old dilemmas,no straight solutions
