肝硬化食管胃静脉曲张出血风险预测中AIMS65评分的应用分析
郭回希

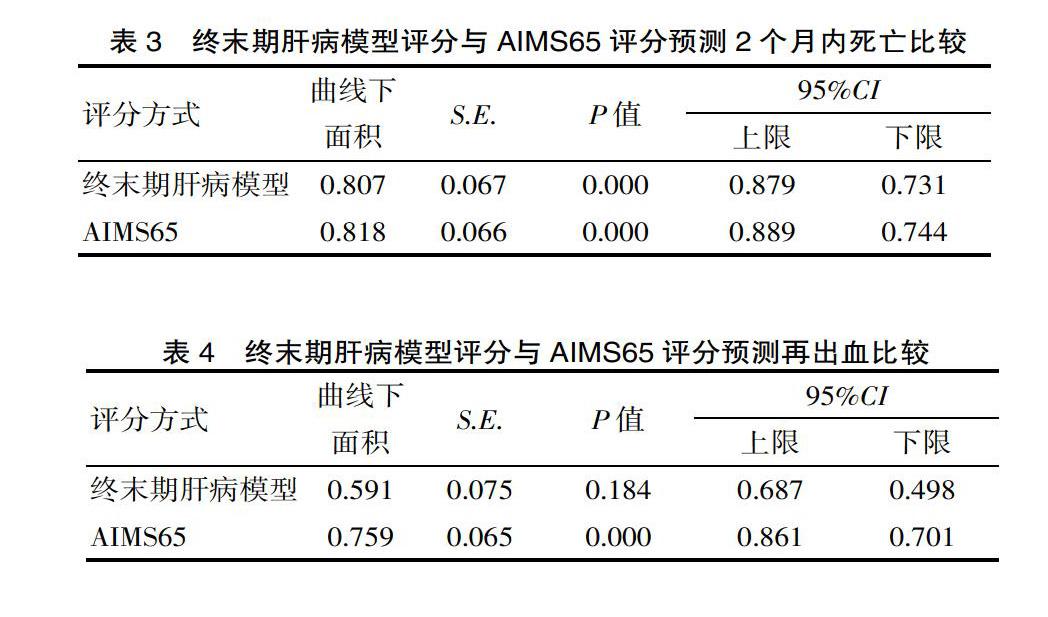
[摘要] 目的 研究肝硬化食管胃靜脉曲张出血风险预测中AIMS65评分的应用效果。方法 研究对象为方便选取2017年1月—2019年6月入院的82例肝硬化食管胃静脉曲张出血患者,所有患者均选用AIMS65评分与终末期肝病模型进行评估,统计2个月内再出血发生率及病死率,两种评估方式对肝硬化食管胃静脉曲张出血患者短期内预后状况及再出血的预测价值选取受试者工作特征及曲线下面积予以评价。结果 82例肝硬化食管胃静脉曲张出血患者的再出血率、病死率分别为15.85%(13/82)、12.19%(10/82)。生存组终末期肝病模型评分、AIMS65评分分别为(14.57±5.51)分、(1.31±1.14)分,死亡组终末期肝病模型评分、AIMS65评分分别为(21.03±6.44)分、(2.75±1.09)分;对比生存组,死亡组终末期肝病模型评分(t=3.409,P=0.002)、AIMS65评分(t=4.083,P=0.000)更高。终末期肝病模型评分预测死亡的曲线下面积为0.807,AIMS65评分预测死亡的曲线下面积为0.818,差异无统计学意义(Z=0.133,P=0.887)。非再出血组终末期肝病模型评分、AIMS65评分分别为(14.03±5.94)分、(1.28±1.18)分,再出血组终末期肝病模型评分、AIMS65评分分别为(18.49±7.16)分、(2.51±1.12)分;对比非再出血组,再出血组终末期肝病模型评分(t=2.144,P=0.038)、AIMS65评分(t=3.381,P=0.002)更高。终末期肝病模型评分预测再出血的曲线下面积为0.591,AIMS65评分预测再出血的曲线下面积为0.759,差异有统计学意义(Z=20.51,P=0.038)。结论 肝硬化食管胃静脉曲张出血患者短期预后及再出血风险预测中AIMS65评分的应用效果显著。
[关键词] 肝硬化;食管胃静脉曲张出血;AIMS65评分;终末期肝病模型
[中图分类号] R575 [文献标识码] A [文章编号] 1674-0742(2020)07(c)-0026-03
[Abstract] Objective To study the application effect of AIMS65 score in the risk prediction of esophagogastric varices bleeding in liver cirrhosis. Methods The study subjects were 82 patients with cirrhosis and esophagogastric varices bleeding admitted from January 2017 to June 2019. All patients were evaluated using the AIMS65 score and end-stage liver disease model, two evaluation methods were used to convenient selection evaluate the prognostic status and predictive value of rebleeding in patients with hepatic cirrhosis and esophagogastric varices bleeding in short time. Results The rebleeding rate and mortality rate of 82 patients with liver cirrhosis and esophagogastric varices bleeding were 15.85% (13/82) and 12.19% (10/82), respectively. The end-stage liver disease model score and AIMS65 score of the survival group were (14.57±5.51)points and (1.31±1.14) points respectively, and the end-stage liver disease model score and AIMS65 score of the death group were (21.03±6.44) points and (2.75±1.09) points, respectively; Compared with the survival group, the end-stage liver disease model score (t=3.409, P=0.002) and AIMS65 score (t=4.083, P=0.000) in the death group were higher. The end-stage liver disease model score predicts the area under the curve of death at 0.807, and the AIMS65 score predicts the area under the curve at 0.818. The difference is not statistically significant (Z=0.133, P=0.887). The end-stage liver disease model score and AIMS65 score of the non-rebleeding group were (14.03±5.94) points and (1.28±1.18) points respectively, and the end-stage liver disease model score and AIMS65 score of the rebleeding group were (18.49±7.16) points and (2.51±1.12) points; compared with the non-rebleeding group, the end-stage liver disease model score (t=2.1439, P= 0.038) and AIMS65 score (t=3.381, P=0.002) were higher in the rebleeding group. The end-stage liver disease model score predicts the area under the curve of rebleeding was 0.591, and the AIMS65 score predicts the area under the curve of rebleeding was 0.759, the difference is statistically significant (Z=5.051, P=0.038). Conclusion The application of AIMS65 score in short-term prognosis and risk prediction of rebleeding in patients with cirrhosis and esophagogastric varices bleeding is significant.

