Evaluate the effects of metabolic syndrome in adolescents and children
Rui-Min Ji*, Xio-Ning Yn, Jing Sun
aNursing College, Shanxi University of Chinese Medicine, Jinzhong, Shanxi 030619, China
bClinical Practice of the Fourth College, Shanxi University of Chinese Medicine, Jinzhong, Shanxi 030619, China
Abstract: The metabolic syndrome (MS) in adolescents and children can cause serious consequences that lead researchers to pay efforts to study in such area. Presently, MS de finition is still not standardized. Different versions of MS de finition have been used by numerous studies, which may be a problem to identify MS and then to predict and prevent clinical diseases. The pediatric literature shows that insulin resistance and obesity might be the key underlying pathophysiology of MS to cause many related diseases. High prevalence of MS is in overweight and obese children and adolescents. This article focuses on such above issues and also effects of MS on two main disease outcomes: cardiovascular disease and type 2 diabetes.
Keywords: metabolic syndrome · children/adolescents · type 2 diabetes · cardiovascular disease · metabolic syndrome de finition · insulin resistance · obesity
1. Introduction
The interest of metabolic syndrome (MS) has been increased since the last century. This concept was first exposed in the 1920s and the publication indicated that MS was associated with hypertension, gout, and diabetes. Following, in the 1940s, some ground-breaking research by Vague were conducted on the correlation between central body fat distribution and several risk factors of cardiovascular disease (CVD). Later, in the 1990s, the lecture of Reaven’s Banting started the modern era of MS. He drew new attention to the correlation between insulin resistance and many metabolic abnormalities linked to MS also named as “syndrome X.”1Recently, the de finition of MS is a cluster of risk factors for atherosclerotic CVD and type 2 diabetes mellitus(T2DM) which consist of obesity, glucose intolerance,abnormal lipid pro file, and hypertension.2In the Ozanne and Hales’ study, the possible mechanisms of developing T2DM and MS in regard to fetal development were reviewed.3It indicated that MS development may be associated with early growth restriction in utero which might lead to onset of the pathological processes of T2DM in early childhood. Childhood MS might raise the risk of T2DM, CVD, and other related diseases,for instance, nonalcoholic fatty liver disease and polycystic ovary syndrome in life.4Additionally, MS in childhood may likely track into adulthood, but the evidence is limited, owing to limited studies that track participants during childhood to adulthood period and always use secondary data that may not be strong enough to reveal such tracking. Until at present, little has been known how well MS in children can predict adult disease.5
Recently, the common recognitions about the components of pediatric MS and its important predictability in the risk of T2DM and CVD development have been made during the accumulation of research evidence.This article aims to discuss those two diseases as the consequence of MS through MS de finition and the major underlying pathophysiology.
2. MS de finitions in adolescents and children
The de finition of MS in children and adolescents has not been uni fied, and it is usually based on the adult standards (such as the International Diabetes Federation(IDF) guidelines) and varies with different ethnic populations by different criteria and cutoff points.6Five similar studies were chosen and examined their MS de finition,among which some criteria for de fining MS were used in later studies. Those studies were conducted among the American adolescents to predict the prevalence of MS.Four of them used the modi fied adults version to de fine MS (the National Cholesterol Education Programme—Adult Treatment Panel III) (NCEP-ATP III) (see Table 1 for speci fic criteria of NCEP-ATP III).7-11Another study used MS de finition derived from the 2007 child IDF.11,12Findings showed that several cutoff points of variables are different and ambiguous, even using the same resource to classify MS.
Speci fically, for de fining variables with varied levels,fasting triglyceride (TG) was de fined as ≥150 mg/dL by Park et al.8; however, de fined as ≥100 mg/dL by de Ferranti et al.7and Cook et al.9; and de fined as ≥110 mg/dL by Duncan et al.10For de fining variables whether considering gender’s difference, waist circumference (WC)was de fined as >75th percentile by de Ferranti et al.7and de fined as ≥90th percentile by Cook et al.,9Duncan et al.,10and Ford et al.,11but de fined separately in genders: >102 cm for male and >88 cm for female in Park et al.8
Furthermore, some studies de fined MS by using speci fic ethnic or race criteria. However, which level should be selected as criteria for MS in children does not have a universal agreement.5Different thresholds for some of the essential variables are used by studies,which may lead to the dif ficulty of diagnosing MS, estimating MS prevalence and the clinical consequences.According to those studies, a standardized de finition of children may be needed even though they had a common disadvantage that was measured body mass index(BMI) instead of WC. Tables 2 and 3 show the speci fic range of characteristics and measures used commonly for diagnosing MS in children.

Table 1. NCEP-ATP III de finition of MS in adults.
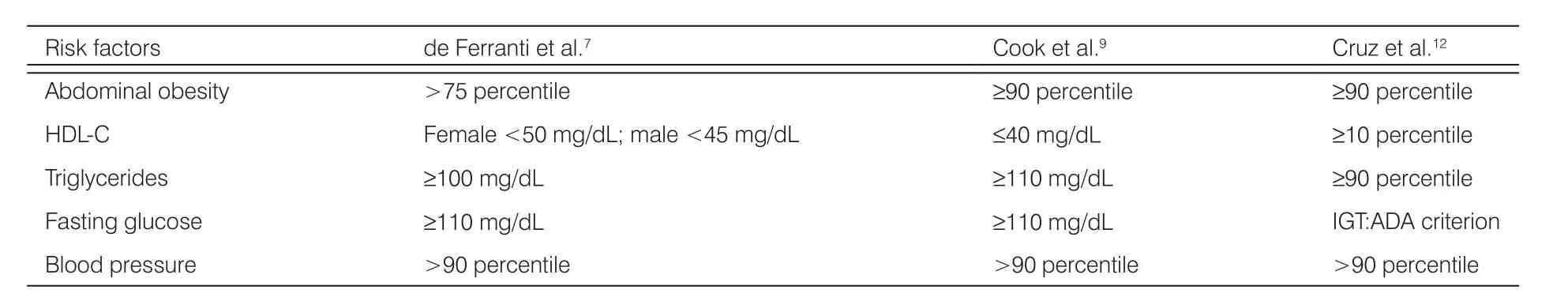
Table 2. Published de finitions of MS in pediatrics.
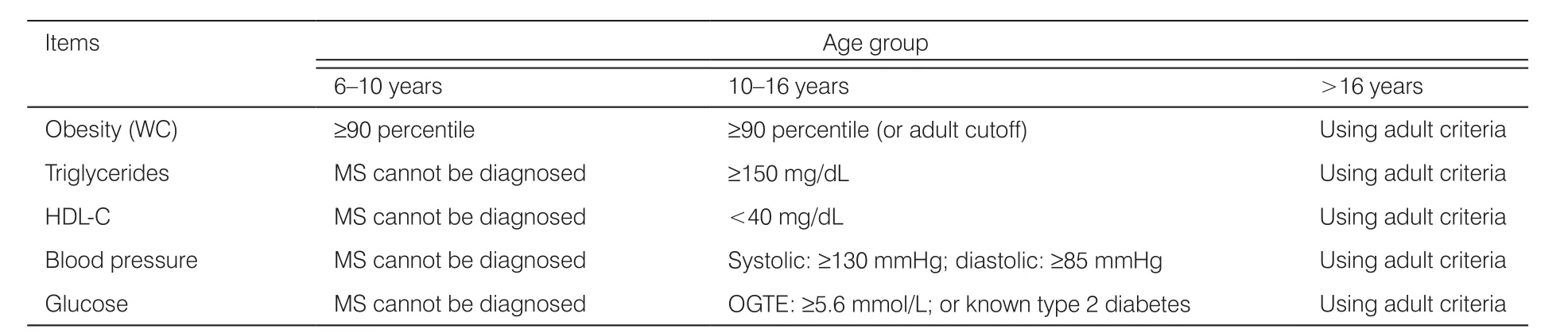
Table 3. IDF de finition of MS in adolescents and children
However, a single MS de finition to adolescents and children might not be proper to show problems in this age, owing to the unique physical development during childhood.10Endocrine levels may be in fluenced by pubertal development and genders. A typical previous study indicated that the adverse association existed among puberty, body fat, age, insulin resistance, and adiponectin. Compared with prepubertal children, pubertal children had apparently lower adiponectin level (P < 0.001). Especially, adiponectin was shown to be at lower level in pubertal girls, and no difference of adiponectin had been found between prepubertal girls and boys. The negative association had been observed among body fat (r = 0.44; P = 0.002),age (r = 0.41; P = 0.003), insulin resistance (r = 0.33;P = 0.016), and adiponectin.13Hence, for adolescents and children, to de fine abnormalities by using single cutoff point might not be suitable. A recent study combined clinical indicators and diseases as criteria. Speci fically, five criteria were: TG serum concentration≥150 mg/dL/treating TG; in male high-density lipoprotein cholesterol (HDL-C) <40 mg/dL/in female <50 mg/dL/treating HDL-C; BMI > age and 95th percentile;glucose concentration ≥100 mg/dL/treating hyperglycemia; systolic blood pressure (SBP) ≥130 mmHg or/and diastolic blood pressure (DBP) ≥85 mmHg/treating hypertension.12
Additionally, there are also some other dif ficulties in determining a standardized de finition of MS in children.For example, ethnic differences exist in developing MS.14MS criteria may need consider ethnic variations and immigrant population.
3. Impact of MS on CVD and T2DM
MS is de fined as a cluster of high TGs, obesity, low HDL cholesterol, high blood pressure, and insulin resistance which associate with the early progress of coronary atherosclerosis and T2DM.2,3In the pediatric literature,lot of effort has been made to explore the relationship among CVD, T2DM, and MS. MS in children may be an indicator of CVD and T2DM in their adult period, but limited data directly explore the impact of MS on disease outcomes in adolescents and children. The consistent finding was that there is a strong positive relationship between children with MS and the development of CVD in their later life. Youth with MS were at two- to threefold risk of having subclinical atherosclerosis (carotid intima-media thickness) and T2DM compared with healthy youth.15
However, the correlation between the severity of MS and the level of adiponectin and fasting insulin has been not clear enough. One recent study pointed that childhood MS Z-scores had a positive association with insulin levels in adult (P < 0.001) and a negative association with levels of adiponectin (P = 0.01). For individual analyses, greater levels of insulin and MS Z-score during adulthood were signi ficantly related to greater odds of occurrence CVD and diabetes over the following 11.2 years (P < 0.001).
Therefore, MS severity had a long-term link to the level of adiponectin and insulin, and it independently and consistently correlated with T2DM and CVD,which may be owing to the potential, environmental,and genetic in fluence over time. So, in the future,MS severity may be used as a risk predictor of these diseases.16
The correlation among MS, T2DM, and CVD varied with ethnicity and race. The black population with MS has a greater risk of CVD than the white population with MS. The reason may be that MS induces some nontraditional risk factors of CVD including C-reactive protein, high level of low-density homocysteine, lipoprotein oxidation, adiponectin, lipoprotein a, and plasminogen activator inhibitor-1, and so on. Therefore, to predict and examine CVD and T2DM caused by MS should consider ethnicity/race and also nontraditional and traditional risk factors. Researchers suggested that nontraditional risk factors need to be added in the de finition of MS.17
4. Major pathophysiology of MS contributing to consequences of CVD and T2DM
4.1. Insulin resistance
Insulin resistance may be a core abnormality of a clustering of CVD and T2DM risk factors.15Higher baseline insulin concentration in youth gradually develops MS,which provides the evidence that insulin resistance might precede and enhance the development of MS in childhood. Increased insulin levels had greatly adverse levels of other risk factors that subsequently led to MS,regardless of race, age, and sex. According to the report of WHO, in 2017 about 425 million people had diabetes worldwide, and by 2040 the number will increase to 642 million. Among diabetes, there will be about 70% people with MS, mainly at puberty age.18
Normally people with higher insulin concentration had lower level of HDL-C and higher level of DBP and SBP, very low-density lipoprotein (VLDL) cholesterol,low-density lipoprotein (LDL) cholesterol, total cholesterol, TGs, and glucose, compared with people with lower insulin level.19Obesity (WC > 90 cm), triacylglycerol level >150 mg/dL, blood glucose >100 mg/dL,HDL-C <40 mg/dL, and blood pressure >130/85 mg/dL had a strong association with insulin resistance.20
4.2. Obesity
According to a recent report study, approximately 44.3%of obese children have characteristics of MS, and lower percentage of normal weight children have only one risk factor of MS.21Another study even showed a higher prevalence (70% obesity with SM) through modi fied guidelines of WHO.22
Obesity, particularly, abdominal obesity may directly contribute to the progress of MS and cardiovascular risk.It has been known that childhood obesity is related to increased blood pressure, low HDL-C, increased TGs,abnormal glucose levels, reduced vascular function,and insulin resistance.17Central obesity (WC > 90 cm)is strongly associated with MS, on which genetic variants may have an effect. Obese genes and lipid metabolism can drive genetic predisposition to MS. Examining genetic variants in MS polygenic scores may be a way to identify the child and subsequently the adult belonging to a high-risk group to early targeting interventions.20
Central obesity induces MS that may also be due to modulating particular signaling pathways, the growth hormone/insulin-like growth factor-1 and ghrelin signaling axis, through which it regulates metabolic homeostasis and energy balance.23
4.3. Both insulin resistance and obesity
Either in the adult or pediatric literature, insulin resistance and obesity are pointed to be always tightly connected with each other and to be as underlying etiological factors to develop MS that may then give rise to CVD and T2DM. The degree of body fat was signi ficantly related to reverting impaired glucose tolerance to normal glucose tolerance and T2DM development. Change in body weight was negatively associated with changes in glucose level and insulin sensitivity. Further reduction of insulin sensitivity exists in youth with a developed T2DM, which was related to a continued weight gain and abnormal body composition pro files such as truncal subcutaneous fat, excess body fat, and abdominal adiposity.24According to a recent study, 53% obese children and adolescents have insulin resistance.22Another study showed that MS with high triacylglycerol and central obesity were correlated with high risk of insulin resistance (OR: 24.4; 95% CI: 5.19e114.42) and (OR: 9.4;95% CI: 3.09e28.68), respectively.25
However, not all obese children or adolescents with impaired metabolism of carbohydrate develop MS and even CVD or T2DM. Probably, other elements such as pathological and metabolic factors and lifestyle factors are involved. Currently, it has been reported that the lead of urinary level was positively correlated to MS.26Unhealthy lifestyle (including smoking, low income, low physical activity, and alcohol intake) has a negative effect on diseases development.27Overall, the interaction between the elements of MS and between other metabolic factors may ultimately lead to disease.
5. Conclusions
There are several points that may need to be emphasized for the future study. First, the de finition of MS may need to be standardized. Number of studies have been attempted to characterize MS in children. However, to date, there has been no universally accepted MS de finition in children, which may lead to the situation where it is hard to diagnose MS and to estimate its clinical consequences, and subsequently hard to take early treatment. To de fine the standardized concept of MS may need complete understanding of the underlying pathophysiology and consideration of variations concerning related factors including age, ethnicity, sex, family history, and lifestyle behaviors. Second, the true picture of diabetic and cardiometabolic risk may be due to overweight/obesity and insulin resistance, but that may not mean that other traditional components of MS, pathological and metabolic factors, and genetic factors can be ignored to predict CVD and T2DM.
Ethical approval
Ethical issues are not involved in this paper.
Conflicts of interest
All contributing authors declare no con flicts of interest.
- Frontiers of Nursing的其它文章
- Concept analysis of nurse burnout
- The ethical dilemma of placebo use in clinical practice
- From an aging person to an elegant senior: a humanistic approach to viewing older adults
- Nursing decision support system:application in electronic health records†
- A review of the research on music therapy in hospice care†
- Adherence to medication behavior among tuberculosis patients and their affecting factors: a cross-sectional study at Public Health Center of Wonogiri District, Indonesia

