Adherence to medication behavior among tuberculosis patients and their affecting factors: a cross-sectional study at Public Health Center of Wonogiri District, Indonesia
Nit Yuninti Rtnsri, Putri Hlimu Husn, Mrni Mrni, Susn Nurtnti,Tntut Susnto*
aDepartment of Nursing, Giri Husada Nursing Academy, Wonogiri, Jawa Tengah, Indonesia
bDepartment of Community, Family, and Gerontic Health Nursing, Faculty of Nursing, University of Jember, Jember, Indonesia
Abstract: Objective: This study aimed to identify the in fluence of predisposing, enabling, and reinforcing factors and the adherence to medication behavior among tuberculosis patients in Selogiri Wonogiri Public Health Center.
Methods: This study employed a descriptive cross-sectional research design. A questionnaire was used to collect primary data.Secondary data were obtained from patient treatment cards (Form TB 01). This research was carried out at Selogiri Health Center from November to December 2017. The participants were patients, both new and old patients, who had completed their treatment in the last 2 months or more, recorded from January 2016 to December 2017. A total sampling technique was used in this study.Logistic regression analysis was used to analyze the in fluence of predisposing, enabling, and reinforcing factors and the adherence to medication among tuberculosis patients.
Results: The results of logistic regression analysis indicated that there were four independent variables that have a signi ficant relationship with treatment variables, namely education (odds ratio (OR) = 0.025; 95% con fidence interval (CI) = 0.001-0.039);knowledge (OR = 3.37; 95% CI = 0.19-57.71); type of drug (OR = 0.448; 95% CI = 0.012-16.07), and means of transportation(OR = 25.77; 95% CI = 1.33-500.47).
Conclusions: Education, knowledge, type of drug, and means of transportation in fluence medication compliance among tuberculosis patients. Therefore, supporting patients during medication program of tuberculosis is needed to improve their adherence medication during multidrug therapy.
Keywords: tuberculosis · adherence to medication · predisposing · enabling · reinforcing
1. Introduction
Tuberculosis remains a major health problem in the world. It caused 9.6 million new cases and 1.5 million deaths worldwide in 2014.1Similarly, tuberculosis is also a serious health problem in Korea with an incidence rate of 77 per 100,000 population in 2016. This lists Korea one of the countries with a high incidence of tuberculosis.2In Iran, tuberculosis was also reported as a serious health problem, especially in Tehran which is the most populous city in Iran.3The country that has the highest number or tuberculosis cases in the world is India, followed by Indonesia as the second largest contributor.4
The duration of treatment has an impact on the risk of treatment failure of the disease.5Inhibiting factors for treatment success that can cause multidrug resistance(MDR) of tuberculosis include incomplete and inadequate treatment of patients, interruption of availability of anti-tuberculosis drugs (OAT), and low quality of drugs that can cause recurrence of the disease.6Efforts have been made to use OAT and Bacillus Calmette Guerin(BCG) vaccination; however, tuberculosis cannot be still eradicated.7Adherence to treatment is one of the potential factors to improve healing.8Factors that in fluence the level of medication adherence are age, occupation, free time, supervision, type of drug, the dose of medication, counseling from health workers, knowledge, and attitudes of patients. Knowledge about this disease is one of the important factors in preventing transmission.9,10
The total number of tuberculosis cases in Wonogiri District until the third trimester (July to September 2017) reached 602 new cases. The range of crude death rate (CDR) was approximately 30%, while the standard for finding new cases of tuberculosis at the national level of CDR is >90%. So, the discovery of new cases of tuberculosis in Wonogiri is still relatively low. According to data from Selogiri Wonogiri Health Center, there were 15 new cases and 13 old cases from 2016 to 2017.
As tuberculosis is an infectious disease, patients’adherence to treatment is important and it has to be analyzed. There has been no evaluation of the level of compliance with treatment for tuberculosis patients and the affecting factors. Therefore, it is necessary to conduct research on this issue. The purpose of this study was to determine the in fluence of predisposing factors(sociodemographic data, knowledge, and drug side effects), enabling factors (availability of transportation and drug), reinforcing factors (family role and role of health care providers), and the adherence of medication among tuberculosis patients at Selogiri Public Health Center, Wonogiri District in Indonesia.
2. Methods
2.1. Design
This study employed a descriptive cross-sectional design.
2.2. Participants
This study was conducted at Selogiri Public Health Center from November to December 2017 involving tuberculosis patients who had completed their treatment in the last 2 months or more. The sampling technique used was total sampling because the population is less than 100 people. Therefore, the entire population was sampled. The number of patients recorded at Selogiri Health Center in 2016 and 2017 were 15 and 13, respectively.
The inclusion criteria were tuberculosis patients who were seeking treatment at Selogiri Health Center and registered in the period of January 2016 to December 2017. The exclusion criteria were tuberculosis patients who died, wandering outside the city, moving house, and whose names and addresses were not found. Finally, 23 tuberculosis patients participated in this study.
2.3. Measurement
Data collection was done by visiting the respondents’house. Primary data were collected using a questionnaire and secondary data were obtained from patient treatment cards (Form TB 01).
A self-administered questionnaire and patient treatment cards (Form TB 01) were used to collect data.Questionnaire was included age, gender, education level, work/occupation, monthly income, knowledge level, side effects of drugs, availability of drug and transportation, family role, and role of of ficer. Those variables included were predisposing factors (sociodemographic data, knowledge and drug side effects), enabling factors(availability of transportation and drug), and reinforcing factors (family role and of ficer role). The adherence to medication behaviors was performed using patient treatment cards (Form TB 01) in Supplementary 1.
2.4. Ethical consideration
This study was approved by Institutional Review Boards of Ethical Committee from Diploma of Nursing Schools of Wonogiri. Written inform consent was provided voluntarily from all of patients.
2.5. Data analysis
Descriptive analysis was used to analyze of sociodemographic data, knowledge, drug side effects, history of other diseases, availability of drug and transportation, family roles, the role of of ficers, and medication compliance. Chi-square test was employed to determine the relationship between these independent variables and adherence to medication behavior. Then, a logistic regression analysis was used to analyze the in fluence of predisposing, enabling, and reinforcing factors and the adherence to medication among tuberculosis patients. Data were analyzed by using SPSS Statistics program with signi ficance level p < 0.05.
3. Results
3.1. Description of the characteristics of the respondent
A total of 23 respondents were enrolled in this study, consisting of 14 (60.9%) men and 9 (39.1%)women. In terms of the age distribution, 5 participants (21.7%) were <35 years and 18 participants(78.3%) were >35 years. With regard to the education level, 19 participants (82%) had low education background, while 4 participants (17.4%) had high education background. Fifteen respondents (65.2%) stated that they worked, and eight (34.8%) stated that they did not work. In terms of knowledge about tuberculosis, 17 participants (73.9%) had good knowledge,while 6 respondents (26.1%) had less knowledge.Table 1 shows the distribution of the respondents based on predisposing factors (sociodemographic data, knowledge, and side effects of drugs), enabling factors (availability of transportation and drug), and reinforcing factors (family roles and roles of health care providers).
3.2. Relationship between predisposing,enabling, and reinforcing factors and adherence to medication
Table 2 presents the results of the correlation between predisposing factor and the adherence of medication behavior among tuberculosis patients. The results indicated that there was a signi ficant relationship between education level (p = 0.025) and knowledge level(p = 0.013) and the adherence to medication behavior among tuberculosis patients.

Table 1. Distribution of characteristics of participants (n = 23).
Of note, 21 (91.30%) stated that OATs were always available, while 2 (8.70%) respondents stated that drugs were not always available at Selogiri Public Health Center (p = 0.030). There is a signi ficant relationship between the availability of transportation and adherence to medication among tuberculosis patients(p = 0.025). Among 23 respondents, 16 (69.56%) stated that transportation facilities were always available, while 7 (30.44%) stated that transportation facilities were not always available.
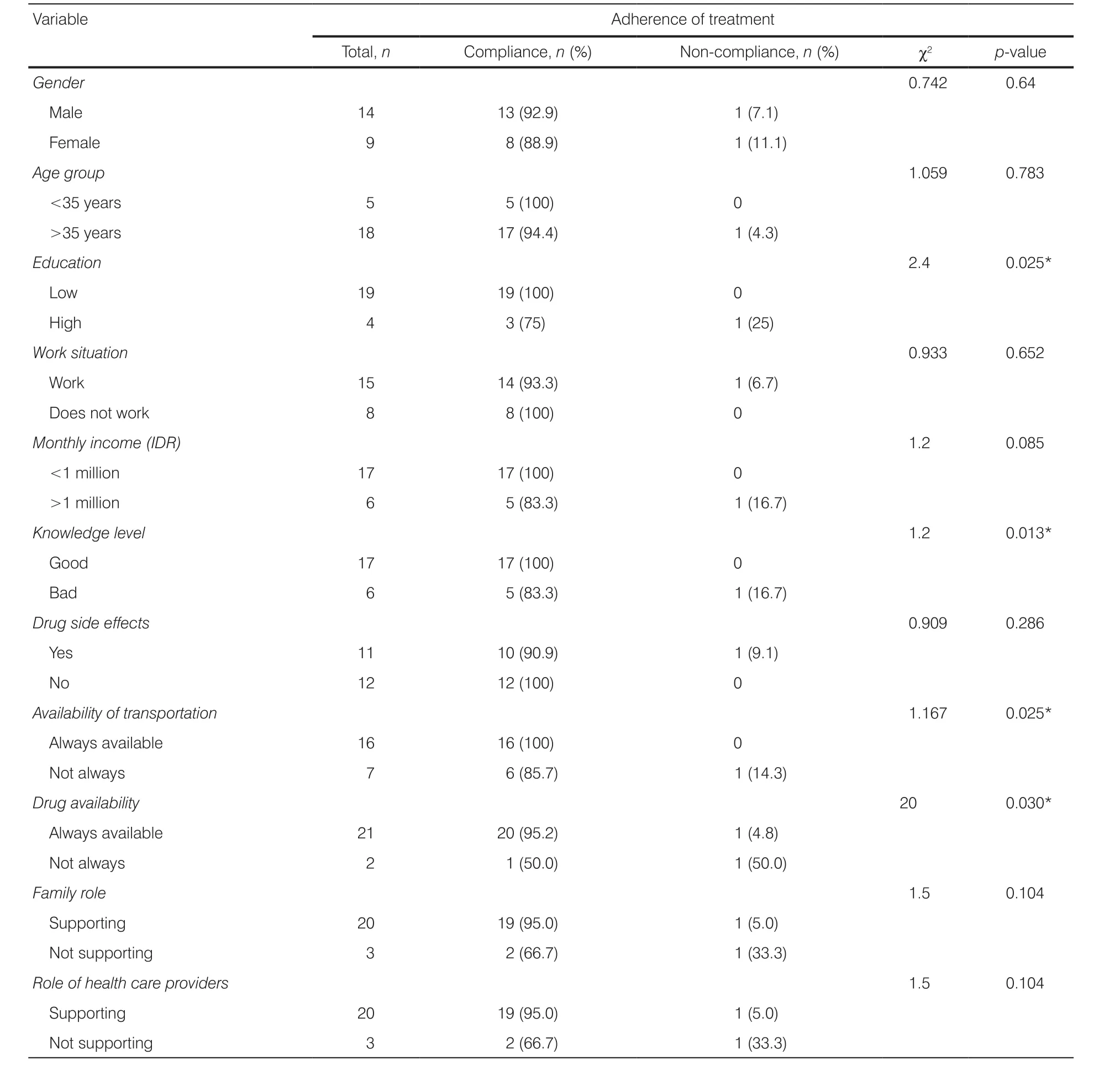
Table 2. Correlation between characteristics of participants and adherence to treatment among tuberculosis patients (n = 23).
There was no signi ficant relationship between the role of the family, the role of health care providers,and the adherence to medication among tuberculosis patients (p > 0.05). The results showed that 20 respondents (86.96%) stated that they had family support,while 3 (13.04%) stated that they did not receive support from the family. The role of tuberculosis health care providers was also felt by 20 (86.96%) respondents, while 3(13.04%) respondents claimed that they did not receive support from of ficers.
3.3. In fluence of predisposing, enabling, and reinforcing factors and adherence of medication
Table 3 presents the in fluence of predisposing,enabling, and reinforcing factors and the adherence of medication. Four variables were identi fied which in fluenced the adherence to medication among tuberculosis patients, including education (odds ratio (OR) = 0.025;95% con fidence interval (CI) = 0.001-0.039);knowledge (OR = 3.37; 95% CI = 0.19-57.71); type of drug (OR = 0.448; 95% CI, 0.012-16.07), and transportation (OR = 25.77; 95% CI = 1.33-500.47).

Table 3. Logistics regression analysis of factors that in fluence adherence to treatment among tuberculosis patients (n = 23).
4. Discussion
4.1. Relationship between predisposing factors and adherence to medication among tuberculosis patients
The results showed that there was a signi ficant relationship between knowledge and adherence to medication among tuberculosis patients. In the knowledge factor,the respondents were asked to answer eight questions about tuberculosis, which included causes, symptoms,mode of transmission, length of treatment, reason for not taking medication regularly, the number of drug items each time, time, and how to take medication. The results of the analysis showed that 17 (73.91%) respondents had good knowledge and 6 (26.08%) respondents had less knowledge. These results indicate that most respondents know about the disease and how to treat it. Based on the direct observation, it was found that the patients had received health counseling from the of ficers when they were first diagnosed with tuberculosis. If the patients had understood about the illness and the treatment that would be given, it is expected that they will regularly carry out the treatment. This is consistent with the results of research conducted in Sragen which indicated that there is a signi ficant relationship between knowledge and the level of medication adherence in patients with pulmonary tuberculosis in RSUD Dr. Soehadi Prijonegoro Sragen with a signi ficant value of 0.009.11Knowledge of factors that can predict treatment outcomes is bene ficial for of ficers so that they can take appropriate corrective actions for better treatment outcomes.12As previously mentioned, knowledge about tuberculosis is important in health promotion so that individuals can maintain their health and avoid the disease.13
The results showed that there was a signi ficant relationship between the level of education and adherence to medication among tuberculosis patients. The level of education in this study comprises five categories,namely not graduating from elementary school, graduating from elementary school, graduating from junior high school, graduating from high school, and graduate.The higher their level of education, the more likely they will be obedient in treatment.14Low education level can cause patients to face dif ficulties in understanding the explanation of health workers about tuberculosis and its treatment. Their lack of understanding can affect the treatment compliance. In this case, health workers face the challenge of behavioral change in the community by ensuring that patients with symptoms arriving early for screening and patients diagnosed with tuberculosis must have medication adherence behavior. It is necessary to consider the perception of ordinary people in determining why they seek treatment or stop treatment.15
The results of this study showed that 11 (47.82%)respondents felt the side effects of treatment in the form of nausea, dizziness, lack of appetite, and reddish and itchy skin. Drug side effects are the most common problem, accounting for 75% of all problems related to treating tuberculosis patients in Turkey.12A study in Korea involving 655 respondents revealed that the main side effects often arise are digestive disorders (53 patients),joint muscle pain disorders (22 patients), psychic disorders (10 patients), visual disturbances (9 patients), and neurological disorders (8 patients). These side effects occur more frequently in patients undergoing secondline therapy, while the first-line types of drugs that often cause side effects are pyrazinamide, generally occurring in more than 1 in 6 respondents; isoniazid, generally occurring in 5 patients (3 with reddish skin, 1 with hepatitis, and 1 with neurological disorder); ethambutol,causing visual disturbance in 9 patients; pyrazinamide,causing joint muscle pain in 22 patients and digestive disorders in 2 patients (nausea, vomiting, diarrhea, and abdominal pain), and hepatitis in 2 patients.16
4.2. Relationship between enabling factors and adherence to medication among tuberculosis patients
The results indicated that there was a signi ficant relationship between the availability of OATs and adherence to medication among tuberculosis patients. Tuberculosis prevention programs are expected to prevent the spread of this disease and to detect new cases of tuberculosis earlier. Therefore, it is necessary to support the distribution of OATs from the government to Health Center.Problems in the process of storing and distributing OATs can result in reduced drug quality and incompatibility between drug needs and availability.17The existence of drugs that must be taken at the health center also determines the continuity of treatment. If the patient does not take the medicine at a speci fied time or the patient does not take medication regularly (non-compliant), the risk of dropping out can occur. Therefore, if the patient cannot take the drug himself because of work or physical conditions, family members or relatives help the patients.Meanwhile, patient disobedience in running a treatment program can be caused by several things, namely forgetting to take medication, laziness to take medication,going out of town, busy working, dif ficult to get sputum,and so on. Poor treatment compliance is a major cause of drug recurrence and resistance.18
The results showed that 16 (69.56%) participants mentioned that transportation for treatment was always available. The finding shows that there is a signi ficant relationship between the availability of transportation and adherence of medication among tuberculosis patients. This proves that transportation is a factor that determines the success of tuberculosis treatment.The means of transportation used by tuberculosis patients to go to public health centers is a motorcycle (96.1%).19The availability of transportation facilities can improve medication adherence. Furthermore,compliance can be increased if socioeconomic problems, such as transportation facilities, are solved. One of the causes of non-compliance is that the patients do not have money for paying the transportation cost although the transportation to the service is always available. Due to this issue, the patients do not come for the treatment.20
4.3. Relationship between reinforcing factors and adherence to medication among tuberculosis patients
The results showed that there was no correlation between the strengthening factors that include role of family and role of health care providers and adherence to medication among tuberculosis patients. The existence and role of the family are very important to monitor the treatment of patients. So, it can be assumed that the absence of family who observation drug consumption can be the cause of tuberculosis patients stopping their treatment.13
The roles of the public health center of ficers are related to their attitudes when providing health services, providing information about the importance of regular treatment, explaining the rules of taking the right medication and symptoms of side effects that may be experienced by patient, the willingness of the of ficers to listen to the patient’s complaints and provide solutions,and the role of health care providers in providing health counseling to the families of the patients. Similar results also indicated that health workers, in this case, a group of doctors, had a good level of knowledge and experience related to tuberculosis, although special training for this disease was low.12
5. Conclusions
The predisposing factors (education and knowledge)and enabling factors (availability of drug and transportation) in fluence the adherence to medication among tuberculosis patients in Wonogiri Public Health Centers. Those are the key important factors for supporting the compliance of patient during their multidrug treatment. The treatment compliance will determine the success rate of tuberculosis treatment. Therefore,it is necessary to empower the patient through health education and to access of public health centers for improving their adherence to treatment. Then, a crossprogram and a cross-sector collaboration program in public health centers should improve to support government programs in tackling tuberculosis, so that the spread of the disease and bacterial resistance can be prevented.
Acknowledgments
The authors would like to thank the Head of Selogiri Health Center in Wonogiri Regency and his staff for allowing the implementation of this research. They are also grateful to the participants of this study. The authors would like to thank Akademi Keperawatan Giri Satria Husada Wonogiri and Faculty of Nursing, University of Jember.
Ethical approval
This study was approved by the ethics committee of Akademi Keperawatan Giri Satria Husada No. 68/A/AKPER/X/2017.
Conflicts of interest
All contributing authors declare no con flicts of interest.
- Frontiers of Nursing的其它文章
- Concept analysis of nurse burnout
- The ethical dilemma of placebo use in clinical practice
- From an aging person to an elegant senior: a humanistic approach to viewing older adults
- Nursing decision support system:application in electronic health records†
- A review of the research on music therapy in hospice care†
- Evaluate the effects of metabolic syndrome in adolescents and children

