Diagnosis and treatment of mixed infection of hepatic cystic and alveolar echinococcosis:Four case reports
Ji-De A,Jin-Ping Chai,Hao Wang,Wei Gao,Zhe Peng,Shun-Yun Zhao,Xiang-Ren A
Ji-De A,Wei Gao,Zhe Peng,Shun-Yun Zhao,General Surgery,Provincial People's Hospital,Xining 810000,Qinghai Province,China
Jin-Ping Chai,Internal Medicine-Cardiovascular,Provincial People's Hospital,Xining 810000,Qinghai Province,China
Hao Wang,ICU,Provincial People's Hospital,Xining 810000,Qinghai Province,China
Xiang-Ren A,Department of Clinical Laboratory,Provincial People's Hospital,Xining 810007,Qinghai Province,China
Xiang-Ren A,Department of Clinical Laboratory,Qinghai Province Key Laboratory of Laboratory Medicine,Xining 810007,Qinghai Province,China
Xiang-Ren A,Department of Clinical Laboratory,Qinghai Clinical Medical Research Center,Xining 810007,Qinghai Province,China
Abstract
Key words:Cystic and alveolar echinococcosis;Mixed infection;Case report
INTRODUCTION
Echinococcosisis a zoonotic parasitic disease caused by larvae ofechinococcusand is mainly caused by the following five types ofechinococcus:Echinococcosis granulosus,E.multilocularis,E.oligarthrus,E.vogli,andE.shqucus[1].Cysticechinococcosiscaused byE.granulosusis distributed globally.Alveolarechinococcosiscaused byE.multilocularisis only distributed in the northern hemisphere.The two populations are the main causes of humanechinococcosis[2].In China,echinococcosisis usually cystic or alveolar.Cysticechinococcosisaccounts for approximately 95% of allechinococcosis,while hepatic cysticechinococcosisaccounts for approximately 75% of all cysticechinococcosis[3].To date,there are numerous reports about single infections of cystic or alveolarechinococcosisin different organs[4,5],but there reports about mixed infections of cystic and alveolarechinococcosisin the same organ are rare.In this study,a typical case was chosen from the 4 patients with mixed infection of hepatic cystic and alveolarechinococcosiswho were treated in the Division of General Surgery of Qinghai Provincial People's Hospital.The cases were reported in detail as follows.
CASE PRESENTATION
Chief complaints
The typical case was a 56-year-old Tibetan man who was admitted to our hospital on March 5,2019,due to “swelling and pain in the right upper abdomen for over 2 years,and yellow skin for 2 mo.” The other 3 cases were all Tibetan women,and their ages were 26-,42- and 49-years-old.They were admitted to our hospital due to “right upper abdominal distension and pain discontinuity for more than 1 year,” “right upper abdominal distension and pain discontinuity for more than 2 years,” and “physical examination found hepatic hydatidosis for more than 10 years.”
Life history in an epidemic area
The 4 patients all lived in a pastoral area in southern Qinghai Province for a long time,and they had a history of close contact with cattle,sheep,and dogs.
Physical examination
The patient with a typical case suffered from severe yellow skin and yellow sclera,and the palpebral conjunctiva was not pale.The abdomen of the patient was flat,there was tenderness and rebound tenderness of the whole abdomen,muscular tension was positive,there was no abnormal mass by touching,no swelling was appreciated in the liver and spleen,and shifting dullness was negative.However,no positive physical signs were found in the other 3 patients.
Laboratory examinations
Enzyme-linked immunosorbent assay forechinococcosiswas positive for all patients.Indicators of liver functions in the typical case suggested that the synthesis and reserve functions of the liver were severely impaired.The specific data were as follows:alanine transaminase was 227 U/L (normal range,7 to 45 U/L),aspartate aminotransferase was 242 U/L (normal range,13 to 40 U/L),total bilirubin was 379.6 μmol/L (normal range,5.0 to 21.0 μmol/L),direct bilirubin was 199.5 μmol/L (normal range,0 to 3.4 μmol/L),indirect bilirubin was 180.1 μmol/L (normal range,1.3 to 18.7 μmol/L),albumin was 25.2 g/L (normal range,40 to 55 g/L),and serum cholinesterase was 2920 U/L (normal range,5300 to 11300 U/L).The indicators of liver functions in the other 3 cases were normal.
Imaging examinations
The typical case of abdominal enhanced CT (Figure 1) and preoperative threedimensional reconstruction (Figure 2) showed that there were multiple lesions ofechinococcosisin the liver,approximately 13.2 cm × 7.0 cm in size in the S4 segment and approximately 13.9 cm × 12.2 cm in size in the S5-8 segments.The other 3 cases of abdominal enhancement CT are shown in Figure 3,Figure 4,and Figure 5.
Preoperative assessment
Preoperative assessment of the typical case showed Child-Pugh classification of liver functions of grade C,PNM standard classification[6]of P4N1M0,and PIVM classification[7]of PI,IV-VIII I1V1M1.The preoperative assessments of the other 3 showed Child-Pugh classifications of liver functions that were respectively grade B,grade A,and grade A;PNM standard classifications that were respectively P4N1M0,P3N0M0,and P3N0M0;and PIVM classifications that were respectively PI,VI,VIII I1V1M1,PV-VIII I1V1M1,and PV-VIII I1V1M1.
FINAL DIAGNOSIS
The final diagnoses of the 4 cases were mixed infection of hepatic cystic and alveolarechinococcosis,but the supplementary diagnoses of the typical case were obstructive jaundice,liver function impairment,and hypoproteinemia.
TREATMENT
The typical case had clear surgical contraindications;thus,the complications of hepaticechinococcosiswere treated first.On March 12,2019,the patient underwent percutaneous transhepatic cholangial drainage guided by ultrasound for biliary drainage.Preoperative assessment was performed once again on the 26thday after admission,and the results showed that cardiopulmonary functions were normal,and the Child-Pugh classification was grade B.We decided to perform surgical resection after preoperative discussion.On April 8,2019,extended right hepatectomy was performed (Figure 6).The surgery took approximately 11 h.Intraoperative bleeding was approximately 3000 mL,1600 mL suspended red blood cells and 740 mL plasma were infused,and the hepatic portal was blocked for 55 min during the operation using the Pringle maneuver.After the operation,the patient was transferred to the intensive care unit for life support,and the next day,was transferred to a specialized ward for rehabilitation treatment.Postoperative pathology showed that the patients suffered from hepatic cystic and alveolarechinococcosis(Figure 7).However,1 of the other 3 cases showed hepatic hydatid lesions invading the blood vessels of the second hepatic hilum after entering the abdomen,and the patient could not undergo routine radical resection of the lesions.The liver was enlarged and heavily congested.Considering the establishment of collateral circulation,it was decided that onlyhepatic cystic hydatid cystectomy should be performed.The other 2 patients underwent radical excision.After the operation,drainage of abdominal abscesses guided by ultrasound was performed,antibiotic was replaced by vancomycin,and fresh plasma was infused.On the postoperative 30thday,all drainage tubes were removed,and the patient was discharged after recovery.The patients started to take oral albendazole after discharge,with the daily dose of 15 mg/kg.The medicine was discontinued after 2-3 wk,and indicators of liver functions were tested.If indicators ofliver functions were normal,then the medicine was continued after 2-3 d,but if the liver damage was severe,it was recommended to start hepatoprotective therapy after discontinuing the medicine.The next cycle of drug-assisted therapy continued after all indicators of liver functions had recovered to normal levels.The first review was performed once every 6 mo,and abdominal color Doppler ultrasound or abnormal CT was repeated once 1 year later and every year thereafter.
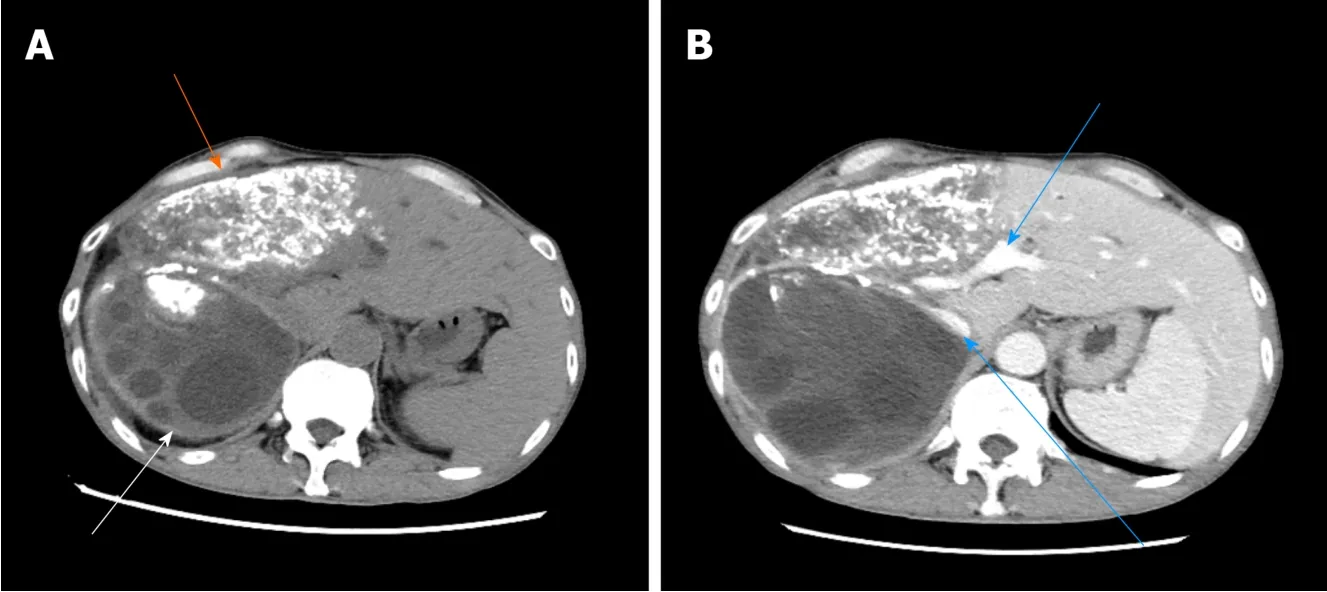
Figure 1 The typical case of abdominal enhanced computed tomography.A:The low-density shadow indicated by the white arrow is cystic echinococcosis with multiple different sizes of subcysts inside,while the high-density shadow indicated by the orange arrow is alveolar echinococcosis,which exhibited patchy calcification;B:The high-density shadows indicated by the blue arrows are the retrohepatic inferior vena cava and portal vein.

Figure 2 The typical case of preoperative 3D reconstruction.A:In the three-dimensional reconstruction system,red represents the abdominal aorta,dark blue represents the inferior vena cava,purple represents the portal vein,orange represents cystic echinococcosis,while light blue and green represent alveolar echinococcosis;B:In the three-dimensional reconstruction system,red represents the abdominal aorta,dark blue represents the inferior vena cava,purple represents the portal vein,orange represents cystic echinococcosis,while light blue and yellow represent alveolar echinococcosis.

Figure 3 The second case of abdominal enhancement computed tomography.A:The low-density shadow indicated by the white arrow is a cystic hydatid lesion,while the high-density shadow indicated by the orange arrow is an alveolar hydatid lesion;B:The blue arrow indicates the retrohepatic inferior vena cava.
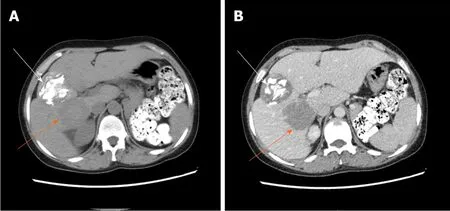
Figure 4 The third case of abdominal enhancement computed tomography.A:The high-density shadow indicated by the white arrow is a cystic hydatid lesion,while the low-density shadow indicated by the orange arrow is an alveolar hydatid lesion;B:The blue arrow indicates the retrohepatic inferior vena cava.
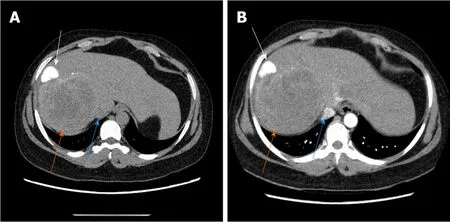
Figure 5 The fourth case of abdominal enhancement computed tomography.A,B:The white arrow shows cystic hydatid foci in high density,the orange arrow shows alveolar hydatid foci in low density,and the blue arrow shows posterior inferior vena cava in equal density.
OUTCOME AND FOLLOW-UP
The 4 patients had different types of postoperative complications such as septic shock,hemorrhagic shock,gastrointestinal hemorrhage,abdominal infection,abdominal abscess,postoperative biliary fistula,hepatic insufficiency,pulmonary infection,pleural effusion,and hypoproteinemia.After symptomatic treatment,such as abdominal drainage,adjustment of antibiotic use and diuresis,all patients recovered or were discharged.For the typical case,almost all of these complications occurred,and after the operation,drainage of abdominal abscesses guided by ultrasound was performed,antibiotic was replaced by vancomycin,and fresh plasma was infused.The patient was discharged after complete recovery on the 30thday after treatments,such as drainage of abdominal abscess guided by ultrasound,replacement of advanced antibiotics (meropenem) and enhanced intravenous nutrition.At the follow-up visit.The typical case patient’s follow-up was conducted 2 mo after discharge,and review of the abdominal CT showed that there was residual liver compensation and hyperplasia,with no recurrence ofechinococcosis(Figure 8).Moreover,this patient reported that he had good recovery,he could take care of himself,and there was no discomfort such as abdominal pain.The follow-up is still in progress.The other 3 patients were followed up for a period of 1 mo to 1.5 years.One of the 3 patients underwent hepatic hydatid lesion resection again at 1.5 years after operation becauseshe did not have a radical resection (Figure 9).The prognoses of the remaining 2 patients were good.CT examination of the abdomen showed (Figures 10 and 11)compensatory and proliferative remnants in the liver and no recurrence of hydatid cysts.
买回豆腐,均由舒曼来做。他是学烹饪的,又有多年独立生活的能力,这个活儿非他莫属,他也是这方面的行家里手。
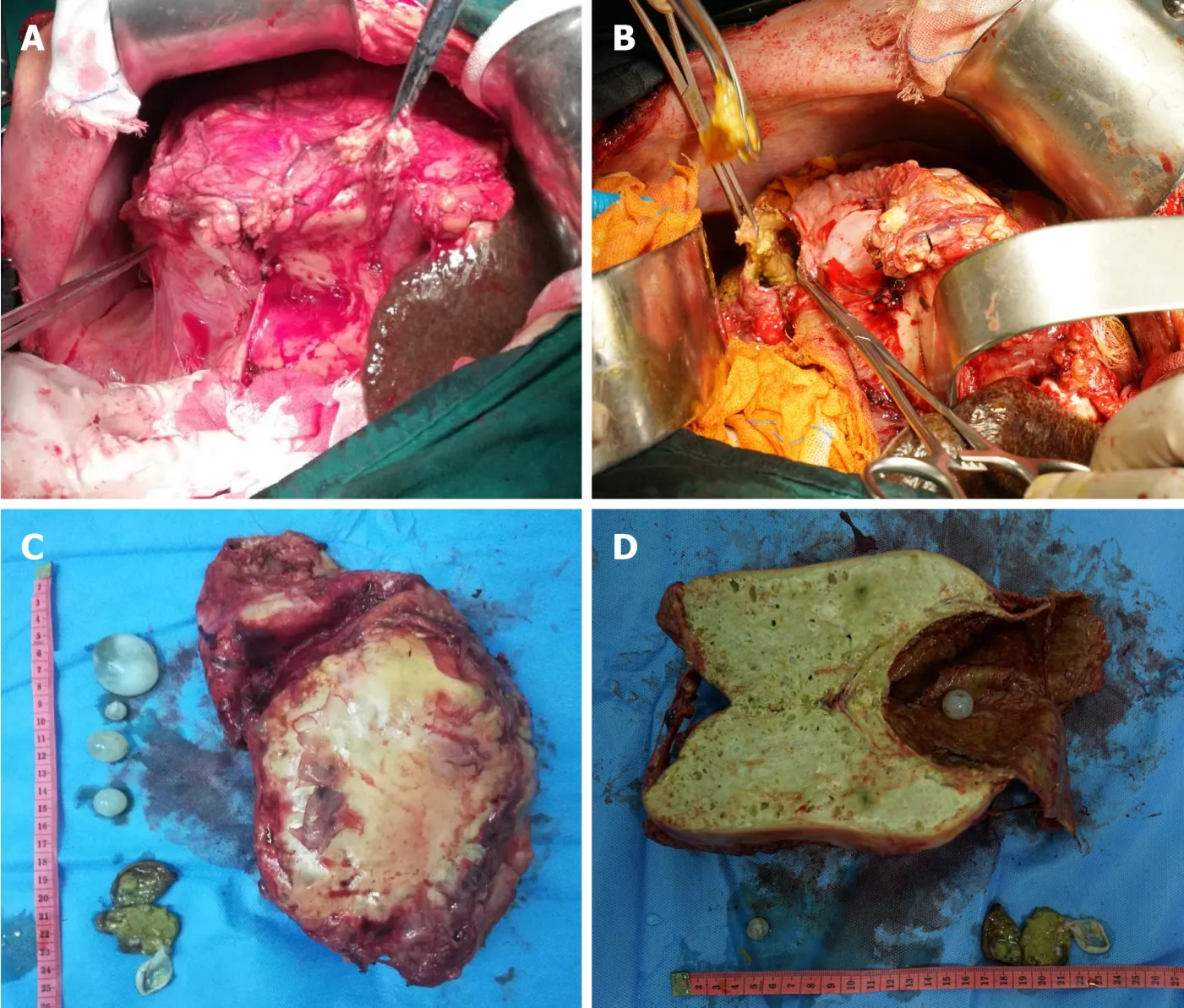
Figure 6 Extended right hepatectomy.A:The structure indicated by the general tweezers is cystic echinococcosis,and the structure indicated by hemostatic forceps is alveolar echinococcosis;B:Since the operating space was narrow,vesiclectomy was performed for the cystic echinococcosis,and cystectomy was then performed after decompression;C:The front view of the specimen,which showed that there were cysts and cystic tissue;D:There were small cysts and cystic tissue of echinococcosis after opening the lesion.
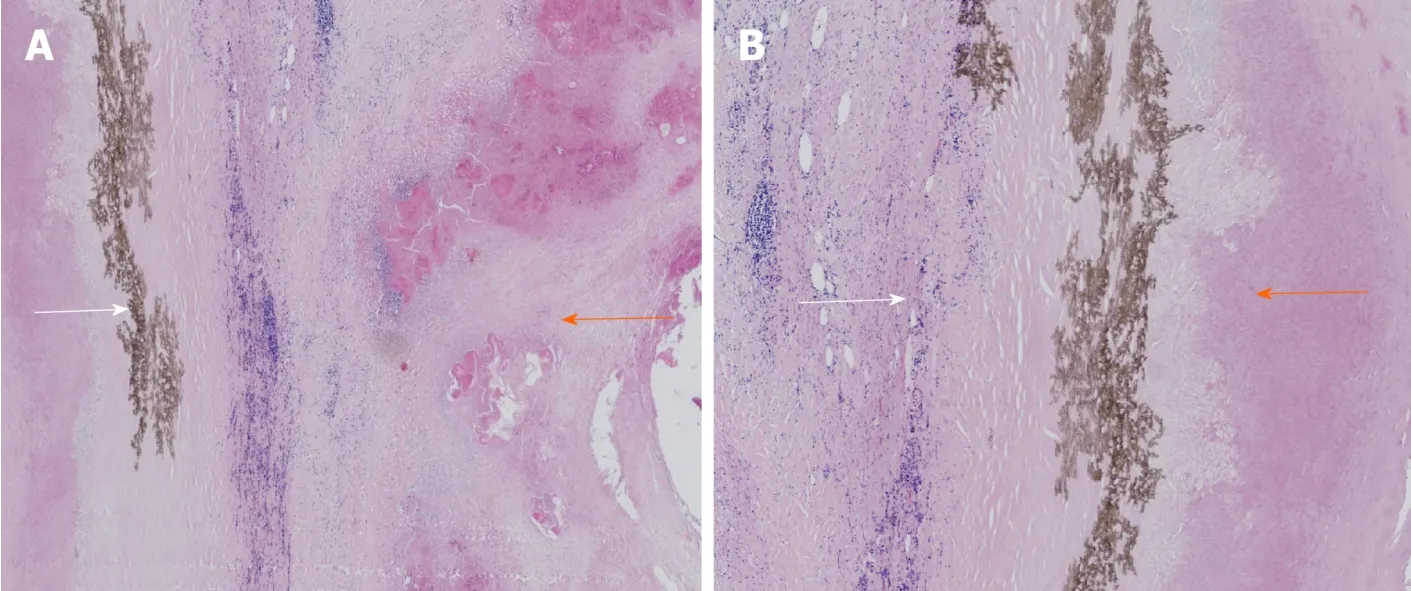
Figure 7 Postoperative pathology.A:The purple tissues indicated by the orange arrows are alveolar echinococcosis,the brown tissues indicated by the white arrows are necrotic cystic tissues that represent cystic echinococcosis;B:The purple tissues indicated by the orange arrows are alveolar echinococcosis,and the brown tissues indicated by the white arrows are necrotic cystic tissues that represent cystic echinococcosis.
DISCUSSION
Mixed infection of hepatic cystic and alveolar echinococcosis is extremely rare,but based on the four aspects,including major symptoms,living history in the pastoral area,manifestations of abdominal CT and enzyme-linked immunosorbent assay evidence ofechinococcosis[8,9],there were essentially no problems in diagnosing this disease.The difficult problems occurred during surgical treatment of this disease,including during the preoperative evaluation and treatment of surgical complications[10,11].First,preoperative evaluation is the key of the whole surgery,as it could determine the involved vessels and bile ducts,as well as prediction of the resectability of the lesion.For instance,for 1 of the other 3 patients in this study,even if a systemic evaluation of the lesion from multiple aspects and multiple perspectives was performed before the operation,the fact that theechinococcosishad invaded the second hepatic hilum so severely was not found.Furthermore,we also had not observed carefully that the three haptic venous outflows were completely obstructed,hepatic congestion was severe,collateral circulation was rich,and there was spongy tortuosityin the portal veins.In addition,radical resection of the lesion was difficult,and the intraoperative bleeding was heavy.We finally decided that only hepatic cystic hydatid cystectomy should be performed.It has been reported that[12]even for patients withechinococcosisinvading the vessels and bile ducts and who were at an advanced stage,radical resection of the lesions and biliary duct reconstruction should be performed if there are no heart and pulmonary dysfunctions or other contraindications.However,it was found in our clinical practice that if radical resection or reconstruction of the outflow tracts could not be ensured for these patients,and perihepatic ligaments containing an abundance of collateral vessels were separated,then the compensatory mechanism of the human body was broken,thus leading to severe postoperative complications,such as intractable ascites and gastrointestinal bleeding.Therefore,routine hepatectomy is difficult for patients with severe hepatic congestion,and allogeneic liver transplantation may be the only choice.Second,there were numerous problems in treating postoperative complications.For instance,our typical case had many complications after the operation,such as biliary leakage,abdominal infection,massive ascites and hepatic insufficiency.Moreover,the case also developed severe complications,such as massive gastrointestinal hemorrhage,hemorrhagic shock and septic shock on the 7thday after the operation.The causes for these complications may include the following:(1) The physique of the patient was poor,and his surgical tolerance was poor;(2) The patient was combined with complications such as obstructive jaundice,liver damage and hypoproteinemia before the surgery,and the first-time Child-Pugh liver function grade was C,which was improved to grade B after the surgery;(3) The surgical method was extended right hepatectomy,which had a large range in radical resection,a small volume of the residual liver,and severe impairment of the synthesis function of the liver after the surgery;and (4) The patient had capillary biliary fistula of the hepatic section.Finally,such cases should be followed in centers with hepatobiliary surgery experience.

Figure 8 Review of abdominal computed tomography.A:The high-density shadow indicated by the white arrow represents metal titanic clips;B:Hyperplasia of the residual liver was good,and there was no recurrence of echinococcosis.
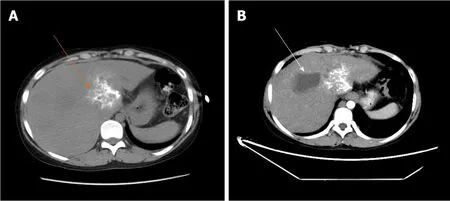
Figure 9 One of the three patients who underwent hepatic hydatid lesion resection again.A,B:Computed tomography scan 1.5 yr after the operation showed that the lesion of the hepatic S1 segment alveolar echinococcosis still existed,as indicated by the orange arrow.Segments S7 and 8 are the residual cystic cavity of the hydatid cyst,which is indicated by the white arrow;B:The S1 segment of the alveolar hydatid lesions invaded the retrohepatic inferior vena cava.The liver showed congestion-like changes.The blue arrow indicates the retrohepatic inferior vena cava.
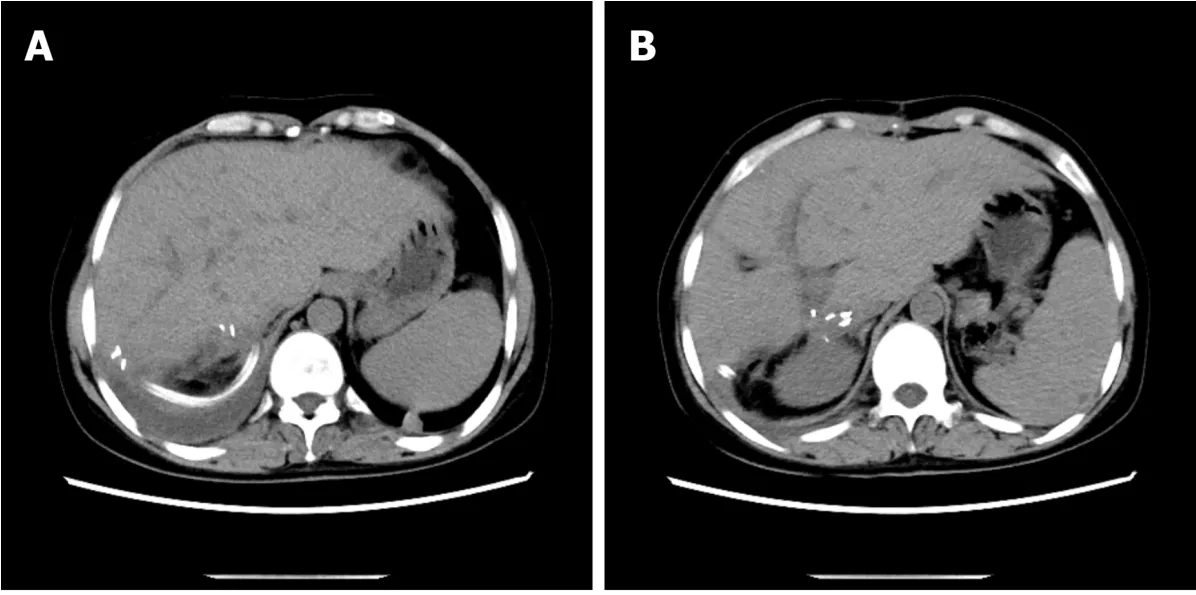
Figure 10 At 1 mo after operation,there was no fluid in the abdominal drainage tube,and there was no hydrocele in the abdominal cavity and good liver hyperplasia (A,B).The high-density image in the picture is a metal titanium clip.

Figure 11 At 3 mo after operation,a small amount of yellowish pus (10-20 mL/24 h) still remained in the abdominal drainage tube (A and B).Abdominal computed tomography showed that the compensatory increase of the left lobe of liver and the absorption of the peritoneal effusion were obvious.The high-density image in the picture is a metal titanium clip.
CONCLUSION
In summary,diagnosis of hepatic cystic and alveolarechinococcosisis easy;the difficulties include preoperative evaluation and treatment of surgical complications,especially the precise prediction of hepatic congestion or outflow tract obstruction.Some dilemmas in the surgery may be avoided if surgeons can thoroughly complete the above two points.In this study,the sample size was small,and there was a lack of multicenter communication.Therefore,if there are similar cases in the future,we should expand the sample size to follow up the long-term efficacies of the patients and strengthen the multicenter communication and data sharing.
Patients in this study were willing to share their medical data,and they tried their best to provide informed consent.
 World Journal of Clinical Cases2020年17期
World Journal of Clinical Cases2020年17期
- World Journal of Clinical Cases的其它文章
- Diagnosis and treatment of an elderly patient with 2019-nCoV pneumonia and acute exacerbation of chronic obstructive pulmonary disease in Gansu Province:A case report
- Active surveillance in metastatic pancreatic neuroendocrine tumors:A 20-year single-institutional experience
- Shear wave elastography may be sensitive and more precise than transient elastography in predicting significant fibrosis
- Surgical strategy used in multilevel cervical disc replacement and cervical hybrid surgery:Four case reports
- Gallbladder sarcomatoid carcinoma:Seven case reports
- Diagnostic value of ultrasound in the spontaneous rupture of renal angiomyolipoma during pregnancy:A case report
