Demyelinating polyneuropathy and lymphoplasmacytic lymphoma coexisting in 36-year-old man:A case report
Lesia Rozłucka,Department of Internal Medicine,Allergology and Clinical Immunology,Faculty of Medical Sciences in Zabrze,Medical University of Silesia,Katowice 40-752,Poland
Elżbieta Semik-Grabarczyk,Marta Pietrukaniec,Agnieszka Żak-Gołąb,Michał Holecki,Department of Internal Medicine,Autoimmune and Metabolic Diseases,Faculty of Medical Sciences in Katowice,Medical University of Silesia,Katowice 40-752,Poland
Małgorzata Grabarczyk,Student Scientific Society at the Department of Internal Medicine,Autoimmune and Metabolic Diseases,Faculty of Medical Sciences in Katowice,Medical University of Silesia,Katowice 40-752,Poland
Sebastian Grosicki,Department of Hematology and Cancer Prevention,Faculty of Health Sciences in Bytom,Medical University of Silesia,Bytom,41-902,Poland
Abstract
Key words:Lymphoplasmacytic lymphoma;Chronic inflammatory demyelinating polyneuropathy;Polyneuropathy;Paraneoplastic neuropathy;Autoimmunity;Case report
INTRODUCTION
Chronic inflammatory demyelinating polyneuropathy (CIDP),the most common chronic autoimmune polyneuropathy,is a rare neuromuscular disorder of spinal nerve roots,major plexuses,and the proximal nerve trunks.Its incidence is estimated to be 1.6/100000 per year with a prevalence of 8.9/100000[1].CIDP mainly occurs between the 3thand 6thdecade,slightly more often in men[2,3].It may be associated with viral infections (e.g.,hepatitis C,human immune deficiency virus),connective tissue disease,hyperthyroidism,diabetes mellitus,but also with hematological diseases,the diagnosis of which may often be preceded by CIDP[4].The clinical manifestations of CIDP include progressive,symmetric paresis and weakness of the proximal and distal parts of upper and lower limbs.Paresis effects roots,plexuses or nerve trunks,which results in general paresthesia,sensation (touch,pain,temperature) loss and balance problems.Cranial nerves are occasionally affected.The complete clinical symptoms develop gradually within two months[5].The course of the disease can be:(1)Monophasic;(2) Chronic and progressive;and (3) Variant with periods of remission and relapses.Due to the similar clinical and pathological course,the differential diagnosis of CIDP should include Guillaine-Barré (GB) syndrome[2,6].Lymphoplasmacytic lymphoma (LPL) is a rare B-cell type of non-Hodgkin’s lymphoma.It originates from small mature B cells,that can differentiate into plasma cells[7,8].The prevalence is about 2% of blood cancers,and the annual incidence is six per million people.The disease usually affects older adults (the average age at the moment of diagnosis is 63-68),it develops slowly and leads to malignant proliferation of lymphoid line cells in the bone marrow[9,10].Approximately 30% of patients develop symmetrical sensorimotor polyneuropathy (multifocal or mononeuropathy),which may precede general symptoms of lymphoma[11].
CIDP has been described in association with different malignancies.The most common are lymphomas.Thirteen patients with lymphoma described by Vialaet al[12]suffered from CIDP.Seven of them had non-Hodgkin B-cell lymphoma,two non-Hodgkin T-cell lymphoma and remaining four Hodgkin Lymphoma[12].Another study analyzed fifty-three patients with lymphoma and various paraneoplastic neurologic symptoms.While cerebral degeneration was mainly associated with Hodgkin lymphomas,in patients with non-Hodgkin lymphomas (all B-cell) the most common manifestation of neurologic symptoms was acute or chronic demyelinating polyradiculoneuropathy[13].
CASE PRESENTATION
Chief complaints
A 36-year-old man diagnosed with CIDP and hypothyroidism seven years ago,was admitted in April 2019 to the Department of Internal Medicine,Autoimmune and Metabolic Diseases due to progressive weakness,peripheral edema,weight loss(approximately 10 kg within the previous four months,31 kg in total since CIDP diagnosis),deterioration of appetite and impairment of the muscular system (the patient moved around the house with the help of others).On admission,the patient complained of "stiffness of the torso",sensory disturbances affecting hands and feet in a glove and stocking distribution.
History of present illness
The patient’s condition deteriorated significantly a bout five months before admittance,with particular aggravation of symptoms during the last month.In December 2018 patient was hospitalized due to concomitant edema,protein deficiency and heart failure.Despite intensive diuretic treatment,the improvement was temporary.In the meantime,due to increasing abdominal pain,patient underwent gastroscopy and was diagnosed with gastritis.Proton pomp inhibitors treatment resulted in only partial improvement.The patient’s neurological condition continued to deteriorate despite intravenous immunoglobulin and glucocorticosteroid treatment leading to his necessity of hospitalization.
History of past illness
Patient was diagnosed with CIDP and hypothyroidism in 2012.Since then he was treated using INN-human normal immunoglobulin (Kiovig 60 mg),with the last administration one month before current hospitalization and methylprednisolone (in intravenous pulses followed by an oral therapy).Hypothyroidism was treated with Levothyroxine (50 μg/d).
Personal and family history
Patients’ grandfather died of cancer of unknown localization and mother was treated in the past due to thyroid cancer.
Physical examination upon admission
Physical examination revealed dry,thickened,slightly flaky skin of the whole body and swelling of the lower limbs was also noticeable.Peripheral lymph nodes were not palpable.His body weight was 55 kg,height 178 cm (BMI 17.3 kg/m2).Neurological examination revealed disturbances of deep sensation and vibration sense in the lower limbs,reduction of muscle tone in the limbs except for the hands,symmetrical muscle wasting in the face,upper and lower limbs.
Laboratory examinations
The results of laboratory tests are presented in Table1.The overall clinical picture,as well as the results of laboratory and imaging studies suggested a secondary nature of polyradiculoneuropathy.Despite the negative opinion of a neurologist,the patient underwent a bone marrow aspiration.Bone marrow cytology showed an increased percentage of plasmocytes,which strongly suggested a hematological background.
Imaging examinations
The abdomen ultrasonography revealed abdominal lymphadenopathy and accumulated pericardial and peritoneal fluid.Computed tomography (CT) scan of the chest,abdomen and pelvis revealed streaky fibrous changes at the base of the left lung,and numerous enlarged mesenteric lymph nodes (up to 14 mm × 29 mm,Figure1).
MULTIDISCIPLINARY EXPERT CONSULTATION
Sebastian Grosicki,MD,PhD,Professor and Chief of Hematology Department,Medical University of Silesia,Poland
In the course of diagnostics,an increased pool of lymphoid cells in the myelogram was found and the patient was referred for further diagnosis in the Hematology Department.Fifty-five percent infiltration with clonal plasma,lymphoplasmic and B cells was confirmed in immunophenotype and bone marrow morphology (Figure2).Increased concentration of free kappa light chains in peripheral blood serum and urine,and the presence of M protein in the IgM kappa class in serum was confirmed.In peripheral blood counts,leukocytosis 21.9 × 103/μL (normal range 4.0 × 103/μL-10.0 × 103/μL) with granulocytosis,microcytic,sideropenic anemia and reactive thrombocytosis have been noted.
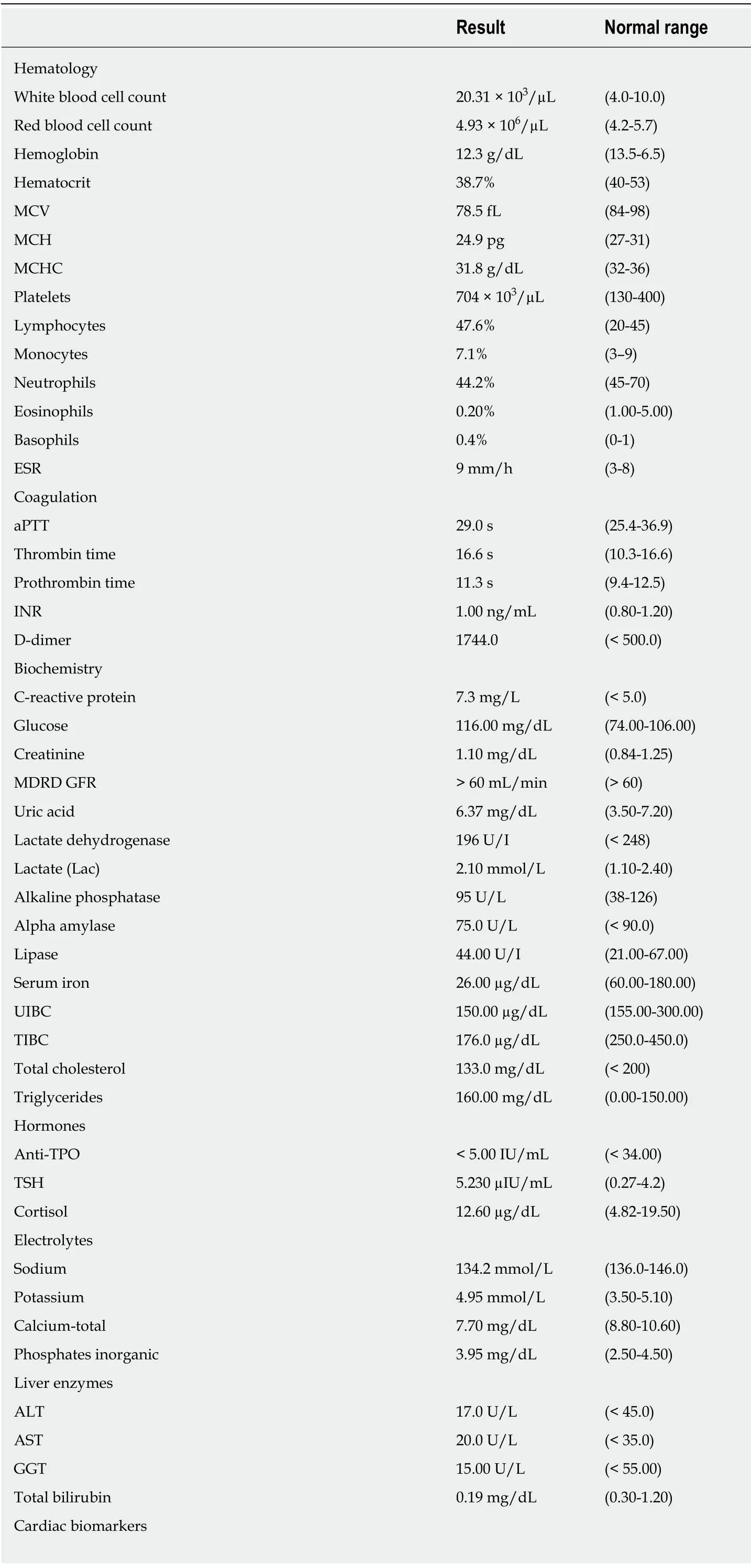
Table1 Laboratory blood test results at hospital admission

MCV:Mean corpuscular volume;MCH:Mean corpuscular hemoglobin;MCHC:Mean corpuscular hemoglobin concentration;ESR:Erythrocyte sedimentation rate;MDRD GFR:Modification of diet in renal disease glomerular filtration rate;UIBC:Unsaturated iron binding capacity;TIBC:Total iron binding capacity;anti-TPO:Anti thyroid peroxidase;TSH:Thyroid stimulating hormone;aPTT:Activated partial thromboplastin time;INR:International normalized ratio;ALT:Alanine aminotransferase;AST:Aspartate aminotransferase;GGT:Gamma-glutamyl transferase;pro-BNP:B type natriuretic peptide;A/G:Albumin/globulin;HbsAg:Surface antigen of hepatitis B virus;anti-CCP:Anti cyclic citrullinated peptide;anti-dsDNA:Anti double stranded DNA;p-ANCA:Perinuclear antineutrophil cytoplasmic antibody;c-ANCA:Cytoplasmic antineutrophil cytoplasmic antibody.
FINAL DIAGNOSIS
Taking into account all the symptoms,a diagnosis of LPL was stated.
TREATMENT
Given the rapidly worsening clinical condition of the patient,R-COP (rituximab 600 mg iv 1 d,vincristin 2 mg iv 1 d,cyclophosphamide 1200 mg iv 1-5 d,methylprednisolone 125 mg iv 1-5 d,) immunochemotherapy as an emergency treatment was started.Unfortunately,despite intensive supportive treatment the general clinical and neurological condition of the patient deteriorated.

Figure1 Computed tomography scan revealing enlarged lymph nodes (marked by arrows) in abdominal cavity.
OUTCOME AND FOLLOW-UP
The patient died on the fifth day of treatment in the Hematology Department.
DISCUSSION
Lymphomas,more commonly B-cell lymphomas including LPL may cause axonal damage or infiltrate peripheral nerves and cause asymmetric mononeuropathy or CIDP[14].Therefore,there are a number of reports regarding occurrence of CIDP in the course of lymphoma,but only a few describing paraneoplastic CIDP,which precede the lymphoma diagnosis[15-17].Vialet al[12]presented nine cases in which CIDP symptoms preceded lymphomas,but none of them where LPL.However,they described a case of 39-year-old man with axonal multiple mononeuropathy which occurs six months before LPL diagnosis and 79-year-old woman with radiculopathy,in whom LPL was diagnosed five months after the first symptoms of radiculopathy.In the first case treatment included doxorubicin-based therapy,intrathecal methotrexate/cyclophosphamide and fludarabine.The second patient was treated with doxorubicin,intrathecal methotrexate and prednisone.In both cases hematological remission and neurological improvement were observed[12].
The patient described by us is an example of paraneoplastic polyradiculoneuropathy and lymphoplasmacytic lymphoma.CIDP was initially diagnosed in 2012,since when remissions and relapses were observed alternately.The patient was treated monthly with intravenous immunoglobulins (Kiovig),and with intermittent intravenous pulses of methylprednisolone sodium succinate (Solu-Medrol).This treatment was initially effective - the patient was able to function normally in everyday life (he worked as a mechanic in the workshop,often travelled abroad,actively spending his spare-time).However,in December 2018 his general health condition (especially neurological) deteriorated.The rapid weight loss was attributed to the intensive diuretic treatment due to concomitant edema,which in turn were caused by protein deficiency and heart failure (not typical for such a young man).Due to increasing abdominal pain,patient underwent gastroscopy and was diagnosed with gastritis.Proton pomp inhibitors treatment resulted in only partial improvement.The patient’s neurological condition continued to deteriorate despite intravenous immunoglobulin and glucocorticosteroid treatment leading to his necessity of hospitalization.
The overall clinical symptoms,the results of laboratory tests and CT scan suggested the secondary background of polyradiculoneuropathy.Despite the different opinion of the neurologists,we stayed with our suspicion of a diagnosis of lymphoma,which was finally confirmed.It seems that the lack of typical symptoms,such as peripheral lymphadenopathy,splenomegaly or low-grade fever,resulted in delaying the diagnosis of lymphoma and worsening its’ prognosis.Disturbing symptoms reported by the patient were not considered to have paraneoplastic origin.It seems reasonable,that such asymptomatic patients should have regular basic laboratory tests such as blood count,blood biochemistry and proteinogram,as well as chest X-ray and an abdominal ultrasound.In case of any abnormalities bone marrow biopsy and hematologist consultation should be done.Polyradiculoneuropathy,while mostly primary,may also by secondary to LPL.Such a situation,when symmetrical sensorimotor polyneuropathy (multifocal or mononeuropathy) precedes the diagnosis of lymphoma,is observed even in 30% of patients.This case should be a reminder to consider an oncological diagnosis in patients with CIDP,especially those with an atypical or rapidly progressive course of the disease.

Figure2 Microscopic view of patients’ bone marrow-lymphoplasmatic lymphoma infiltration.1:Plasmatic cell;2:B cell;3:Lymphoplasmatic cell.
CONCLUSION
CIDP and malignant diseases co-occurrence is ra re,nevertheless patients with atypical symptoms of neuropathy should have extended diagnostics and remain under constant supervision of specialists.
 World Journal of Clinical Cases2020年12期
World Journal of Clinical Cases2020年12期
- World Journal of Clinical Cases的其它文章
- Elevated serum growth differentiation factor 15 in multiple system atrophy patients:A case control study
- Clinical outcomes of sacral neuromodulation in non-neurogenic,non-obstructive dysuria:A 5-year retrospective,multicentre study in China
- Magnetic resonance imaging features of minimal-fat angiomyolipoma and causes of preoperative misdiagnosis
- Recovery from prolonged disorders of consciousness:A dual-center prospective cohort study in China
- Gene testing for osteonecrosis of the femoral head in systemic lupus erythematosus using targeted next-generation sequencing:A pilot study
- Epidemiological and clinical characteristics of COVID-19 patients in Hengyang,Hunan Province,China
