Isolated metachronous splenic multiple metastases after colon cancer surgery:A case report and literature review
Li Hu, Ji-Yun Zhu, Lei Fang, Xiu-Chong Yu, Zhi-Long Yan
Li Hu, Ji-Yun Zhu, Lei Fang, Xiu-Chong Yu, Zhi-Long Yan, Department of Gastrointestinal Surgery, Ningbo First Hospital, Ningbo 315000, Zhejiang Province, China
Abstract
Key words:Colon cancer;Isolated;Metachronous;Splenic metastasis;Literature review;Case report
INTRODUCTION
Splenic metastases in patients with malignant tumors generally indicate multiple metastases[1,2].Isolated splenic metastasis after radical colon adenocarcinoma resection is a rare clinical entity[3].The mechanism of their rarity is unknown and many theories have focused on anatomical and histological aspects.We report a case of isolated splenic metastasis 21 mo after radical colon adenocarcinoma resection, which was successfully treated by totally laparoscopic splenectomy.We discuss the clinical and pathological aspects of the case, and consider the diagnostic and therapeutic options based on our observation of the case.We also reviewed the literature and identified 34 relevant papers, including 28 cases of metachronous metastasis and 6 cases of simultaneous metastasis.
CASE PRESENTATION
Chief complaints
A 48-year-old female patient was admitted to our hospital with elevated serum carcinoembryonic antigen (CEA).The patient had no symptoms of abdominal pain,diarrhea or bloody stools.
History of present illness
The patient underwent laparoscopic radical colon resection 14 mo previously and subsequently underwent a second local resection due to local recurrence detected by elevated serum CEA and positron emission tomography (PET).However, multiple metastases in the spleen were found 7 mo later by elevated serum CEA and PETmagnetic resonance imaging.The patient then underwent a totally laparoscopic splenectomy.Local tumor recurrence and splenic metastasis from the colorectal cancer(CRC) were found by postoperative pathology.
History of past illness
The patient denied a history of hypertension, diabetes, and other relevant illnesses.
Family history
The patient did not have a family history of cancer.
Physical examination upon admission
Physical examination was normal.
Laboratory examinations
Complete blood count, liver and renal function tests, and alpha fetoprotein,carbohydrate antigen 19-9 (CA19-9), cancer antigen 125 (CA125), and CA153 were within normal limits, except for CEA which was 12.41 ng/mL (normal range 0-5.0 ng/mL), 51.49 ng/mL and 206.89 ng/mL, respectively.
Endoscopy
The first endoscopy revealed a sigmoid colon mass.The second and third endoscopies were normal.
Imaging examinations
A sigmoid colon mass was found by abdomen enhanced computed tomography (CT)(Figure 1A).Local recurrence in the descending colon was found by positron emission tomography (PET)-CT (Figure 1B) and lymph nodes showed no high metabolic shadow.Isolated splenic metastasis was found by PET-magnetic resonance imaging(MRI) (Figure 1C) and lymph nodes also showed no high metabolic shadow.
Interventions
The clinical stage assessed by enhanced CT before surgery was cT4aN0M0 and postoperative pathological stage was pT4aN2M0 after laparoscopic radical resection of sigmoid adenocarcinoma and one-stage anastomosis.The patient received chemotherapy (Xelox regimen, capecitabine 1000 mg/m2) for 3 wk with a total of 8 treatment courses.However, the CEA level gradually increased 14 mo after surgery,and PET-CT showing a high metabolic shadow in the descending colon.Following MDT consultation, a second laparoscopic exploration was performed.The extent of local resection based on a laparoscopic exploration and no other recurrences were found.Local resection of the recurrence in the intestinal tract and one-stage anastomosis were carried out during surgery.The tumor edge is 5 cm away from the proximal and distal margin.Postoperative pathology confirmed a poorly differentiated colon adenocarcinoma (with extra-serosal and muscular is invasion).The circumferential, proximal, and distal margins were negative.Xelox chemotherapy was again administered for 3 wk per treatment course for almost 3 mo.At a subsequent examination, the CEA level had gradually increased over the 7-mo period after the second operation.After the second MDT consultation, laparoscopic exploration was performed, and no peritoneal metastases were observed and the spleen was removedvialaparoscopy.The surgical specimen displayed multiple metastases (Figure 2).Chemotherapy with FOLFIRI (irinotecan 180 mg/m2+ 5-FU 400 mg/m2d1, injection,+2400 mg/m2, injection, every 2 wk) and bevacizumab (5 mg/kg drop every 2 wk) was administered for 2 wk following the suggestions by a third MDT consultation.
Pathology
The first postoperative pathology indicated a poorly differentiated adenocarcinoma;4 of 15 perirectal lymph nodes harvested were positive;and circumferential, proximal,and distal margins were negative.The second postoperative pathology showed the same results.The last postoperative pathology indicated multiple metastatic moderately differentiated adenocarcinoma of the spleen, with tumor sizes ranging from 0.4 to 3.0 cm, and originating from CRCviahematoxylin and eosin staining and immunohistochemistry (Figure 3).Genetic analysis of local recurrence and splenic metastasis showed KRAS exon2, APC exon16, and TP53 exon6 missense mutations,while no mutations ofNRAS, KRAF, EGFR, ERBB2, MET, MLH1, MSH2andMSH6were detected.
FINAL DIAGNOSIS
The diagnosis of postoperative isolated metachronous splenic metastasis of CRC requires clear imaging, which can be obtained by CT examinations, and sometimes ultrasonography and PET are required.In our case, PET-CT was performed due to an elevated CEA level, which only revealed local colon cancer and not splenic metastasis(Figure 1B), and subsequent PET-MRI detected isolated splenic metastasis (Figure 1C).Pathological stage I was found in the primary focus in only 1 case (3.4%), stage II in 7 cases (24.1%), stage III in 18 cases (62.1%), and the stage in 3 cases (10.4%) could not be determined.Higher pathological staging suggests the possibility of splenic metastasis.However, stage I CRC can also metastasize to the spleen.Pathological biopsy was needed for the final diagnosis of postoperative splenic metastasis of CRC, 2 cases were confirmed by fine needle biopsy, and the others by postoperative pathology.
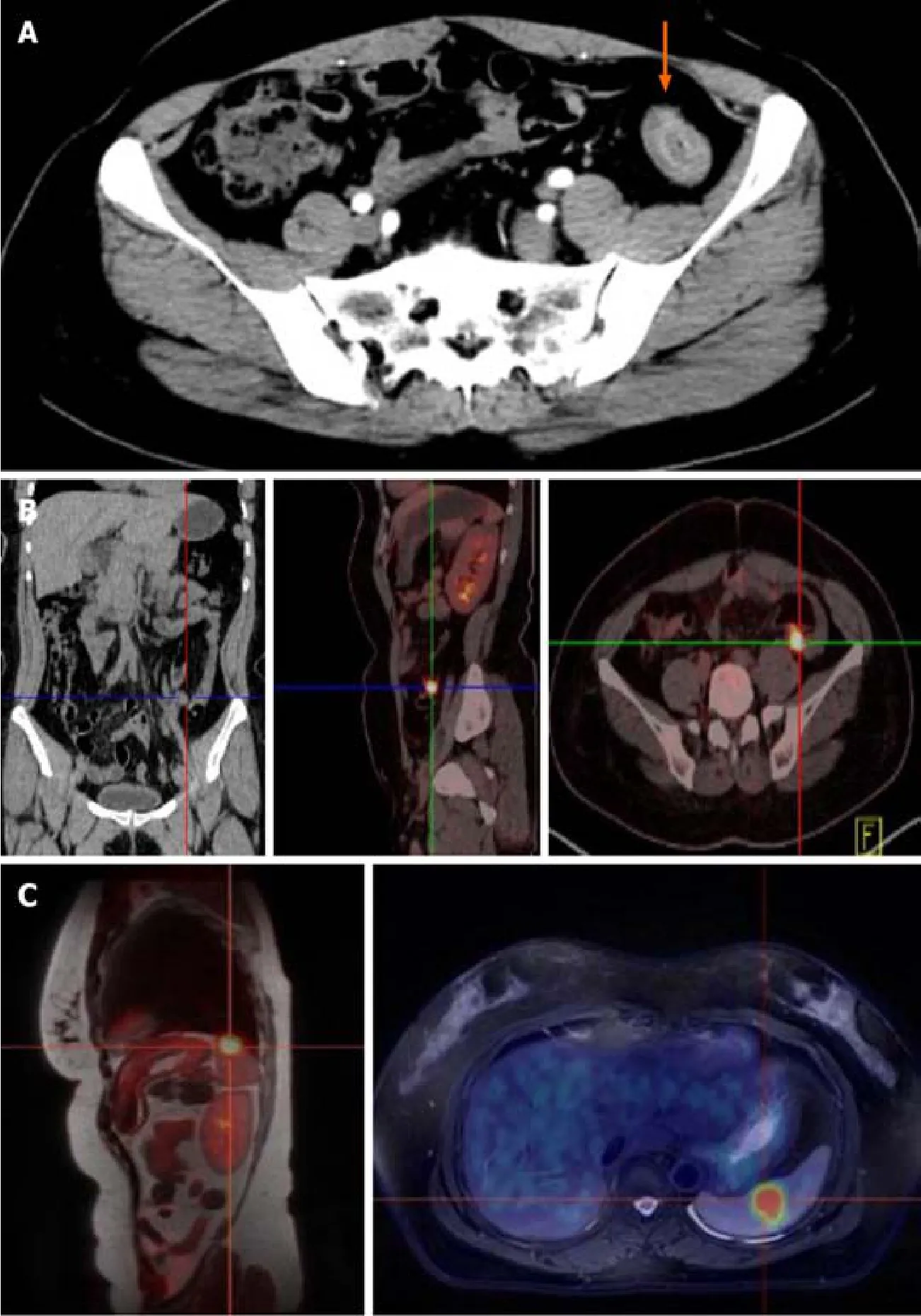
Figure 1 Imaging examinations of the colon.
TREATMENT
The treatment of postoperative isolated metachronous splenic metastasis of CRC includes surgery, chemotherapy combined with targeted therapy or radiotherapy.Surgery was performed in all cases, 2 cases underwent totally laparoscopic splenectomy (including our case), and the remaining cases underwent open total splenectomy.Laparoscopic resection of a splenic malignancy is controversial due to potential cancer cell implantation during laparoscopic surgery.Lopez Monclovaet al[4]reported 6 cases of laparoscopic metastasis splenectomy, all of which had no postoperative complication sand the total survival time ranged from 2 mo to 11 years[4,5].In terms of abdominal organ malignancy, laparoscopic surgery does not result in higher surgical complications than traditional laparotomy[6].Therefore,laparoscopic total splenectomy is safe, reproducible and results in a faster postoperative recovery than traditional surgery.Our patient underwent three surgeries, all conducted under laparoscopy, and no postoperative complications were observed.Chemotherapy is considered a priority treatment for distant metastasis.However, only 4 patients received perioperative chemotherapy and 1 received targeted therapy after splenectomy of metastatic tumors, as shown in Table 1.It is possible to reach a state of No Evidence of Disease after excision of an isolated metastasis and most cases require continuous observation.The time to disease recurrence after splenectomy ranged from 3 to 84 mo (median time 18.0 mo) in these patients.Although few patients were treated with chemotherapy and targeted therapy, systemic chemotherapy still provides an essential contribution to the overall survival rate in the presence of distant metastasis.No relevant literature was identified on the use of radiotherapy in combination with chemotherapy.In our case, patient received chemotherapy combined with targeted therapy after splenectomy, following the suggestions of the MDT.The time without disease recurrence remains to be defined in this patient.

Figure 2 The surgical specimen displayed multiple metastases (A-C).
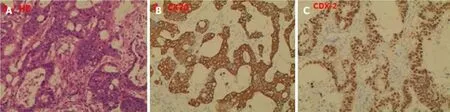
Figure 3 The postoperative pathology (100 ×).
FOLLOW-UP AND OUTCOME
No sign of tumor recurrence or metastasis was observed 7 mo after totally laparoscopic splenectomy.
DISCUSSION
The most common metastatic organ of CRC is the liver, and it has been reported that almost 50% of patients diagnosed with CRC experienced simultaneous orheterogeneous liver metastases[3,7].Splenic metastases in patients with malignant tumors generally indicate multiple metastases[1,2].A splenic primary tumor or metastasis a rare disease, and the most common sources of splenic metastasis are melanoma (34%), breast cancer (12%), ovarian cancer (12%), CRC (10%), and lung cancer (9%)[8,9].However, isolated splenic metastasis is even rarer.Bergeet al[1]found that the splenic metastases accounted for 4.4% in 7165 cadaver reports, of which 1.6%were from colon cancer, and isolated splenic metastases in colon cancer was not mentioned in their paper[1,10].Another global study showed that up to 2012, less than 100 cases of isolated splenic metastases from colon cancer had been recorded[11].
微博是一个有很大网络力量的平台,身边有不少人会玩微博。因为微博能够及时地为你更新出最受欢迎的热点和最新的时政热点或是火热的话题。正因为这样,微博就是一个很好的平台,它的信息量大,流传的速度也够快。那商务英语翻译课程便可以根据微博的这一特点,将自己的有关商务英语翻译课程放到这个平台上边,然后扩散信息,让更多对商务英语翻译课程有兴趣的同学来了解。同样这个方法也可以增强同学们对商务英语翻译课程的兴趣和培养出更多的商务英语翻译人才。我们的商务英语翻译课程视频也可以与当时的时政热点联系到一起,更加吸引阅读者的眼球,从而引起他们对商务英语翻译课程的注意。

Table 1 Cases of isolated splenic metastasis after colorectal cancer surgery from PubMed
Splenic metastases are clinically infrequent;thus, the mechanism of their formation is unknown and many theories have focused on anatomical and histological aspects.With regard to the anatomy of the metachronous metastasis pathway, the splenic artery and abdominal cavity are formed at acute angles and the rhythmic contraction of the spleen[12]prevents tumor cells from remaining and growing in the spleen.Other researchers have proposed that tumor cells from the inferior mesenteric vein flow back into the splenic vein and reverse flow into the spleen, resulting in intra-splenic metastasis.With regard to lymphatic metastasis, there is no direct lymphatic input to the spleen, but there are lymphatic systems in the portal vein, subcapsule and trabeculae of the spleen.Tumor cells entering the spleen through these lymphatic systems may also explain the fact that these tumor cells are limited to the subcapsular membrane and thus form isolated lesions.Histologically, the spleen is the second largest lymphatic reticuloendothelial organ in the body.It is composed of a large number of monocytes, Kupffer cells, immunoglobulins and opsonins, which have a high phagocytic activity.In addition, studies have shown that tumor cells entering the spleen will be destroyed by splenic lymphatic reticuloendothelial cells, preventing tumor implantation.Research has also determined that adenocarcinoma cells flow into the liver faster than they flow into the spleen[1,2,9].This might indicate that the spleen may generate anti-tumor fixations and reproductive factors.Possible causes of rare metastatic tumors of the spleen are summarized in Table 2.
We identified 34 cases of isolated splenic metastasis after CRC surgery from the PubMed database (28 cases of metachronous metastasis and 6 cases of simultaneous metastasis, shown in Table 1).We report the 28thcase of solitary metachronous splenic metastasis in this study.Our case was characterized by a solitary splenic metastasis during the second surgical procedure, followed by multiple metastases in the spleen,which was different from previous reports.It can be seen from Table 1 that the 15 male and 14 female cases were aged between 33 years and 81 years, with a median age of 63.5 years.The majority of cases presented with an increased CEA level (85.7%) and plasma CEA level ranged from 7.2 to 223 ng/mL, while the CEA level in our case reached a maximum of 206.8 ng/mL.The first disease-free interval in these cases ranged from 3 to 144 mo and the first local colon recurrence in our case was observed 14 mo after the first surgery, and the second splenic metastasis was observed 7 mo later.The diameter of the tumors ranged from 1.5 to 18 cm, all of which were a single metastasis, including 6 cases not mentioned in the reports, and our patient had multiple metastases, which ranged from 0.4 to 3.0 cm in diameter (Figure 2).Primary lesions were found in the right hemi-colon in 8 cases (3 cases in the cecum, 4 cases in the ascending colon and 1 case in the colonic liver curvature), accounting for 27.6%.The primary tumor was found in the transverse colon in 1 patient (3.4%), and in 18 cases the tumor was found in the left hemi-colon (1 case in the colonic splenic curvature, 4 cases in the descending colon, 9 cases in the sigmoid colon and 3 cases in the rectum), accounting for 62.1%.The tumor site was not mentioned in 2 cases.The high proportion originating from the left hemi-colon also supports the hypothesis that tumor cells have the trait of a counter current to the spleenviathe inferior mesenteric vein.
CONCLUSION
We report, for the first time, the occurrence of multiple metastases in the spleen during the second postoperative progression of colon cancer.Our findings enrich the data on metastases of the spleen and provide experience in the management of this disease.Close monitoring of serum CEA levels plays a crucial role in the postoperative followup of these patients (Figure 4).Otherwise, the patient may have multiple organ metastases and lose the opportunity of a second or third operation.Surgical removal of the tumor is just part of the treatment regimen, and postoperative chemotherapy,radiation therapy, targeted therapy, immune therapy and follow-up are also important.Appropriate treatment strategies based on MDT consultation is conducive to improving cancer patients’ overall survival and progression-free survival.
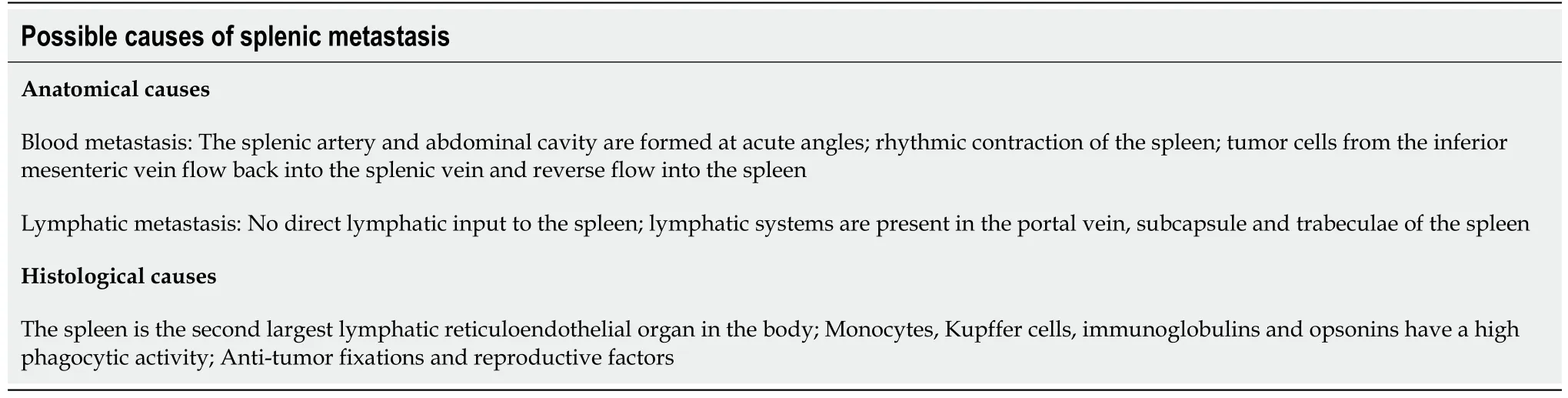
Table 2 Possible causes of splenic metastasis
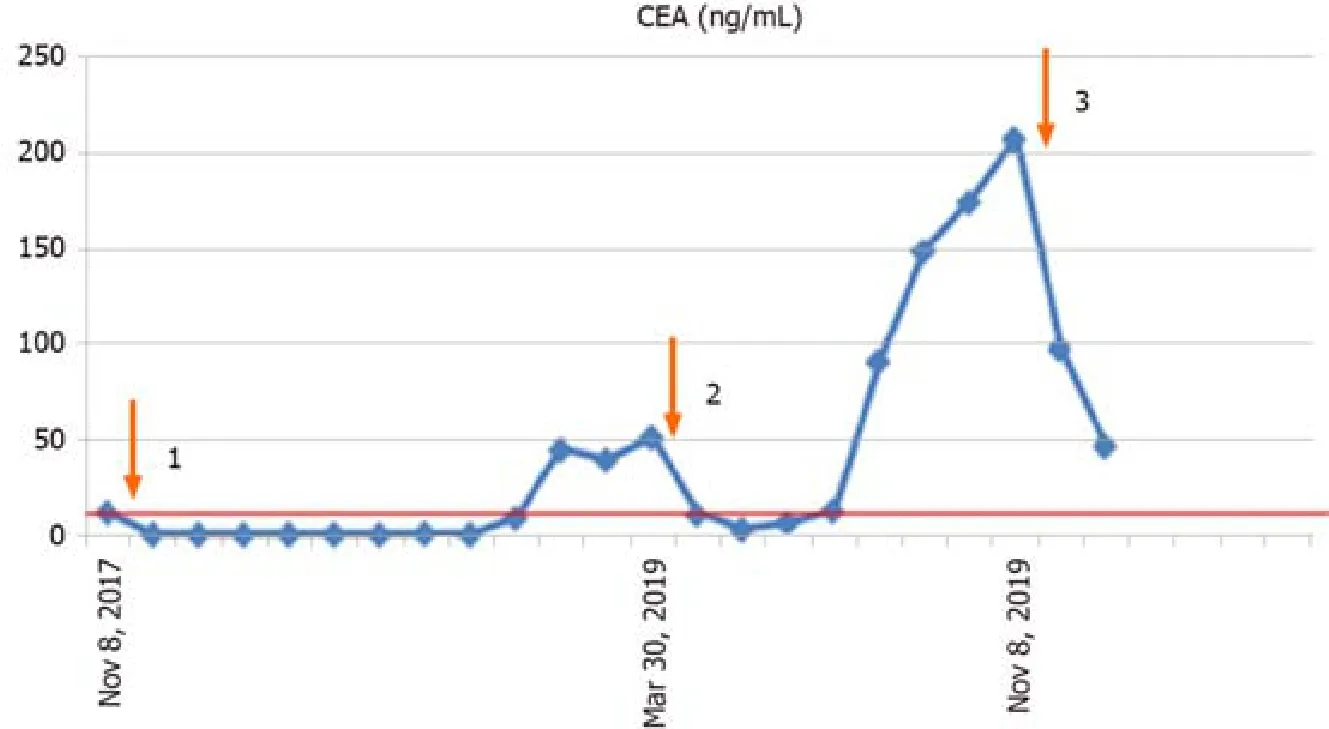
Figure 4 Changes in carcinoembryonic antigen level in the reported patients.
ACKNOWLEDGEMENTS
We thank the patient for permitting us to use her data to complete this article.
 World Journal of Clinical Cases2020年15期
World Journal of Clinical Cases2020年15期
- World Journal of Clinical Cases的其它文章
- Facial and bilateral lower extremity edema due to drug-drug interactions in a patient with hepatitis C virus infection and benign prostate hypertrophy:A case report
- Total laparoscopic segmental gastrectomy for gastrointestinal stromal tumors:A case report
- COVID-19 with asthma:A case report
- Computed tomography, magnetic resonance imaging, and Fdeoxyglucose positron emission computed tomography/computed tomography findings of alveolar soft part sarcoma with calcification in the thigh:A case report
- Acute suppurative oesophagitis with fever and cough:A case report
- Coexistence of ovarian serous papillary cystadenofibroma and type A insulin resistance syndrome in a 14-year-old girl:A case report
