Effects of age and sex on clinical high-risk for psychosis in the community
Frauke Schultze-Lutter, Benno G Schimmelmann, Rahel Flückiger, Chantal Michel
Frauke Schultze-Lutter, Department of Psychiatry and Psychotherapy, Medical Faculty,Heinrich-Heine University, Düsseldorf 40692, Germany
Benno G Schimmelmann, Rahel Flückiger, Chantal Michel, University Hospital of Child and Adolescent Psychiatry and Psychotherapy, University of Bern, Bern 3000, Switzerland
Benno G Schimmelmann, University Hospital of Child and Adolescent Psychiatry, University Hospital Hamburg-Eppendorf, Hamburg 20246, Germany
Abstract
Key words:Psychosis;Clinical high-risk;Attenuated psychotic symptoms;Basic symptoms;Community;Age;Sex;Interview assessment;Prevalence
INTRODUCTION
Psychoses, especially schizophrenia-spectrum psychoses, are severe mental disorders that tend to take an unfavorable course, in particular when the first episode occurs before age 18[1,2], and for this reason, incur immense costs and are a main cause of disability[1]already in adolescents[3].In adolescents, this is despite the fact that the majority of first episodes of psychoses have their onset in adulthood, mostly before age 24[4,5].Furthermore, psychoses affect more men than women[6], in particular after childhood and adolescence, and before age of 45 to 50[5,7].These age and sex effects on incidence rates, and their interaction, are considered to reflect the fundamentally neurodevelopmental nature of psychoses, whereby development involves two critical time windows - early (perinatal) brain development and adolescence - that together produce the symptomatic manifestations of the disorder[1].
Starting in the 1980s, it was increasingly demonstrated that the duration of untreated first-episode psychosis as well as of its prodrome of mostly several years duration is related to poorer outcome[8], especially in psychoses with an onset before age 18[2,9,10].Thus, it was concluded that an earlier detection and treatment of psychoses - preferably before their first episode - was needed[11].Subsequent studies on adult patients produced two complimentary approaches to detect psychosis early,in its clinical high-risk (CHR) state[12,13]:The ultra-high risk (UHR) and the basic symptom (BS) approach, together consisting of five alternatively employed criteria(Table 1).
However, following the increasing involvement of younger age groups in the early detection of psychotic disorders, concerns were raised about the likely impact of age,i.e., developmental aspects on the prevalence, clinical relevance, and psychosispredictive value of CHR symptoms and criteria[17].These concerns were corroborated by significantly lower conversion-to-psychosis rates in UHR samples comprising exclusively children and adolescents compared to adult or mixed adult-adolescent samples[13], and by predominately negative associations between age and CHR criteria and symptoms in both clinical[18-23]and community studies[24,25].Interestingly, when age effects were studied in child and adolescent samples only[22], older adolescents showed better functioning and lower depressive scores;and fewer adolescents than adults reported BS criteria in addition to the main UHR criterion,i.e., the attenuated psychotic symptoms (APS) syndrome (APSS)[21].Details on studies of age effects on CHR symptoms and criteria is provided in the supplementary text 1.As regards effects of sex, despite reported sex differences in prevalence of psychoses and psychosis-spectrum disorders, and their symptom distributions[6,26-29], sex effects on the clinical significance and psychosis-predictive value of CHR symptoms and criteria have been less studied and, apart from more negative symptoms in males, are frequently conflicting[30-43].Details on studies of sex effects on CHR symptoms and criteria is provided in the supplementary text 2.
Aims and hypotheses
It was speculated from findings on age thresholds in CHR symptoms in the community[24,25]that sex differences in brain and cognitive maturation[44-47]might lead to lower age thresholds in the clinical significance of BS and possibly APS in females compared to males.In addition, due to the lack of studies on both age and sex effects on CHR symptoms and criteria, we investigated the effect of both age and sex on the prevalence of CHR criteria and symptoms and on their association with psychosocial impairment and mental disorder in a large community sample of 8- to 40-year-olds.
MATERIALS AND METHODS
Recruitment and sample
The sample was composed of community participants in two studies:The “Bern Epidemiology At-Risk” (BEAR) study[48,49]and the “Binational Evaluation of At-Risk Symptoms in Children and Adolescents” (BEARS-Kid) study[24,25].Both studies used a stratified sampling method to obtain a representative sample of 7370 people aged 16-40 years, in the BEAR study (response rate:63.4%), and of 980 minors aged 8-17 years, in the BEARS-Kid study (response rate:32.6%), from the predominantly Caucasian people registered in the semi-rural Canton of Bern (approximately 1 Mill.)and the city of Bern and its urban hinterland (approximately 200000), respectively.The city of Bern is the largest city of the Canton Bern and has approximately 134000 citizens.In the Canton Bern, 21% of the population are non-Swiss;80% of these are from European countries.Potential participants were randomly drawn from the obligatory population register including their address, date of birth, sex, nationality,and parents’ names (for minors).Telephone numbers were subsequently searched in directories and the Internet.
In both studies, first contact was established by an information letter on the aims of the respective study, voluntariness of participation, and anonymous use of data in group statistics.For the BEAR study, participation in the telephone interview was equated with provision of informed consent;for the BEARS-Kid study, written informed assent/consent was obtained from participants and their parents.Both studies had been approved by the ethics committee of the University of Bern (KEK-BE 172/09 and 174/10).
In both studies, eligibility criteria included main residence in Canton Bern,appropriate age, and an available telephone number.Interviews were discontinued if participants had a past or current diagnosis of psychosis or insufficient understanding of German, French, or English.Recruitment and telephone assessments for the BEAR study were conducted over 3.5 years;recruitment and face-to-face assessments for the BEARS-Kid study over 3.3 years.Prior to merging data, a feasibility study examining the correspondence of telephone and face-to-face assessments of CHR had found excellent concordance rates (78%-100%) between these two assessment modes[50].This finding demonstrated that data of both studies could be merged and compared without danger of introducing a systematic assessment bias.

Table 1 Clinical high risk for psychosis criteria
According to the definitions of the American Association for Public Opinion Research[51], the contact rates of those eligible were 94.8% in the BEAR study, and 82.7% in the BEARS-Kid study;refusal rates were 30.2% and 49.2%.Main reasons for refusal were lack of interest in the topic or lack of time;these reasons were named in both studies by roughly every second and every third refuser, respectively.
Altogether 2683 persons between the ages 16-40 years (inclusive) participated in the BEAR study, 233 persons aged 8-17 years (inclusive) in the BEARS-Kid study.Thus,our final sample (n=2916) included 2539 (87.1%) adults and 377 (12.9%)children/adolescents.As in earlier studies[27,28,45,49], these were divided into seven age groups for the examination of simple age effects:8-12 years (n=117), 13-15 years (n=69), 16-17 years (n=191), 18-19 years (n=167), 20-24 years (n=493), 25-29 years (n=319), and 30-40 years (n=1560).
Assessments
Well-established semi-structured interview assessments were used to assess CHR criteria and symptoms[12,13].The Schizophrenia Proneness Instrument (SPI)[15,16]was used to assess the 14 BS included in the two BS CHR criteria and the criteria themselves (Table 1);in the BEAR study, the Adult version (SPI-A)[15]and, in the BEARS-Kid study, the Child and Youth version (SPI-CY)[16,52]was used.Both versions of the SPI do not differ in the definitions of corresponding BS and BS criteria.As in earlier studies[19,23-25], for the current analysis, cognitive and perceptual BS were distinguished rather than employ the partially overlapping criteria for BS (Table 1).Irrespective of their frequency of occurrence, perceptual BS included at least one visual or acoustic perception disturbance;and cognitive BS included thought interference, blockages, pressure, and perseveration, disturbances of receptive and expressive speech, of abstract thinking, and of discriminating between ideas and perceptions;captivation of attention by details of the visual field;inability to divide attention;unstable ideas of reference;and derealization.The SPI-CY requires a minimum age of 13 years for the assessment of three of the 14 BS included in COPER and COGDIS[16](Table 1).For this reason, main analyses were conducted on the eleven BS assessed across all age groups to avoid a negative selection bias in the youngest age group,i.e., the 8- to 12-year-olds.
Furthermore, the five positive (P) items of the Structured Interview for Psychosis-Risk Syndromes (SIPS)[14]were used to explore the presentation of APS and brief intermittent psychotic symptoms (BIPS), and of the symptomatic UHR criteria (Table 1).More specifically, the current presentation of any APS (any SIPS item from P1 to P5 with a score between 3 and 5) and any BIPS (any SIPS item from P1 to P5 with a score of 6) was assessed.Delusional (P1, P2, and P3), hallucinatory (P4) and speechdisorganization (P5) APS/BIPS were distinguished irrespective of their frequency of occurrence.Of the genetic risk and deterioration syndrome (GRDS), a genetic risk was estimated only by a first-degree relative of psychosis.A schizotypal personality disorder in the participant was not assessed because of the lack of an informant[53]and the non-assessment of the negative schizotypal symptoms, which are part of the negative scale of the SIPS, in the BEAR study, and because of the young age of participants in the BEARS-Kid study.
Symptom-independent current global level of psychosocial functioning was estimated using the Social and Occupational Functioning Assessment Scale(SOFAS)[54];a score ≤ 70 was considered indicative of low,i.e., clinically significant,impairment in functioning.The Mini-International Neuropsychiatric Interview(M.I.N.I.)[55]and its children’s version (M.I.N.I.Kid)[56]were used to assess current axis I disorders according to DSM-IV and to rule out past or present psychosis.Again for the lack of an informant in the BEAR study[53]and for the young age in the BEARS-Kid study, axis II disorders were not assessed.
In addition, as part of the sociodemographic assessment, participants (or a parent,in 8- to 15-year-olds) were asked about first- and second-degree biological family members with mental problems, treated or untreated, and the diagnosis or, if unknown or never seeking help, a description of these problems (and treatment, if applicable).
In both the BEAR and the BEARS-Kid study, interviewers were clinical psychologists who had received an intensive three-month training, especially in the semi-structured context-dependent personalized assessment of CHR symptoms and mental disorders, in order to achieve a ≥ 95% concordance rate with the trainers (in all instances the first or the last author) before the conduction of interviews.Weekly supervision of all symptom ratings performed by the first or last author further ensured excellent, reliable data quality in both studies.
Statistical analysis
Using SPSS 25.0., frequencies were compared by χ2tests, and non-normally distributed interval and ordinal data were evaluated by Mann-Whitney tests.In accordance with other studies of age effects in CHR symptoms and criteria[19,23-25],logistic regression analyses were used to calculate (1) Simple effects of the seven age groups on prevalence rates of CHR symptoms and criteria;(2) Simple effects of sex on prevalence rates of CHR symptoms and criteria;(3) Interaction effects of age and sex on prevalence rates of CHR symptoms and criteria;and (4) The interaction effect of age, sex and the single CHR symptoms or criteria on low psychosocial functioning,and the presentation of at least one axis I disorder as dependent variables.To test the simple effects, we used the enter method.To test the interaction effects, we entered the single variables as well as all of their possible combinations of interactions and employed stepwise logistic regression analyses using both the backward and the forward selection to control for the different suppressor effects associated with each selection mode.Significant predictors that were selected in both searches were reentered in a regression analysis using the enter method to estimate their model fit.Relevant interactions were inspected for their direction by interaction graphs.Throughout, goodness-of-fit was estimated by the Omnibus test.
In accordance with previous studies of age effects[19,23-25], the age group with a peak onset of first episode psychosis (20-24 years) served as a reference group in regression analyses of simple effects of age groups, while age rather than age group was entered in analyses of interactions because of the expected rather small numbers of low functioning and mental disorders per age group.Regarding sex, because of the reported higher incidence of psychotic disorders in men[6], females served as a reference group.There was no missing data.
RESULTS
Sample characteristics
The majority of our sample had a Swiss nationality, already concluded school education, good psychosocial functioning and a normal occupation (Table 2).The rare sex differences were of only small effect size (0.080-0.174), indicating a slight tendency of more men being single, and of more women working in temporary job, reporting a 1st- or 2nd-degree relative with mental disorder, mostly with an affective disorder, and meeting a current non-psychotic axis I disorder.
Prevalence of CHR symptoms and criteria
Altogether, 542 (18.6%) participants reported any CHR symptom;of these, 261 (9.0%)participants reported any one of the 11 BS and 381 (13.1%) any one of the five APS/BIPS, with only ten (0.35%) reporting BIPS (one delusional and nine hallucinatory) (Table 3).Speech-disorganization occurred only at APS-level and was extremely rare, not rated at all in 14- to 19-year-olds (Table 3).
Only 2.8% met criteria of any CHR criterion;mostly the BS criterion “Cognitive-Perceptive BS”, COPER (2.2%) (Table 4).Thus, when only the three criteria recommended within the Guidance project of the European Psychiatric Association(EPA)[13],i.e., APSS, the BIPS syndrome (BIPSS) and the BS criterion Cognitive Disturbances (COGDIS), were considered, only 1.3% met any EPA-recommended CHR criterion (henceforth:EPA criterion).Because of the lack of reporting a sufficient decline in functioning, despite some reports of a family history of psychotic disorders(Table 2), none of the participants met the GRDS (Table 4).Also, BIPSS was very rare,its requirements met by only one participant (Table 4).
Simple and combined effects of age and sex on CHR symptoms
Age effects indicated the same age thresholds for BS as reported earlier from a smaller subsample[25](Tables 5-7),i.e., a threshold of any BS and of cognitive BS in the first half of the twenties and of perceptual BS around age 18, whereby participants below these threshold had a higher likelihood to report BS and effects of age were most pronounced on cognitive BS.A newly emerging significant finding was the lower prevalence of perceptual BS in 30- to 40-year-olds.Overall, BS were significantly less frequent in males, with little differences between cognitive and perceptual BS (Tables 5-7).
Similar to earlier findings on a smaller subsample of the present sample[24], an age effect on the report of delusional APS/BIPS was hardly detectable, apart from a slightly increased prevalence in 30- to 40-year-olds (Table 8).In any APS/BIPS and in hallucinatory APS/BIPS (Tables 9 and 10), an age threshold around age 18 showed with an additional trend toward lesser hallucinatory APS/BIPS in 30- to 40-year-olds counteracting the age effect on delusional APS/BIPS in this age group;consequently,no age effect on any APS/BIPS emerged.Due to their rare occurrence (Table 3), no age effect was detectable on speech-disorganization APS (Table 11).Similar to the findings on BS, APS/BIPS were commonly less frequent in males (Tables 9-10);the only exception occurred in speech-disorganization APS that revealed a statistical trend towards being more frequent in males (Table 11).
Except for the age models on delusional and speech-disorganization APS/BIPS, all models indicated an improved model fit that, just like the explained variance, was commonly greater for the age group models compared to the sex models (Tables 5-11).
Except for delusional APS/BIPS that were only predicted by female sex (Table 8),both forward and backward selections indicated an effect of both age and sex on the report of CHR symptoms (Tables 12-17).In doing so, except for cognitive BS (Table 13), age and sex - if selected - were not only independent predictors but weakly interacted with each other (Tables 12, 14-17).Visual inspection of the interaction graphs revealed that, in case of any BS and perceptual BS, the likelihood of reporting these BS decreased with age in females, while it increased with age in males.Additionally, the presentation of both any and perceptual BS was generally more likely at a younger age and in females, with sex having a greater effect than age.A similar interaction was found for speech-disorganization APS, yet, with positives cases being generally older than negative cases.
In case of any APS/BIPS and hallucinatory APS/BIPS, interaction graphs revealed a contrary pattern with the likelihood of reporting these APS/BIPS increasing with age in females and decreasing in males, both against the background of younger age being an independent predictor.
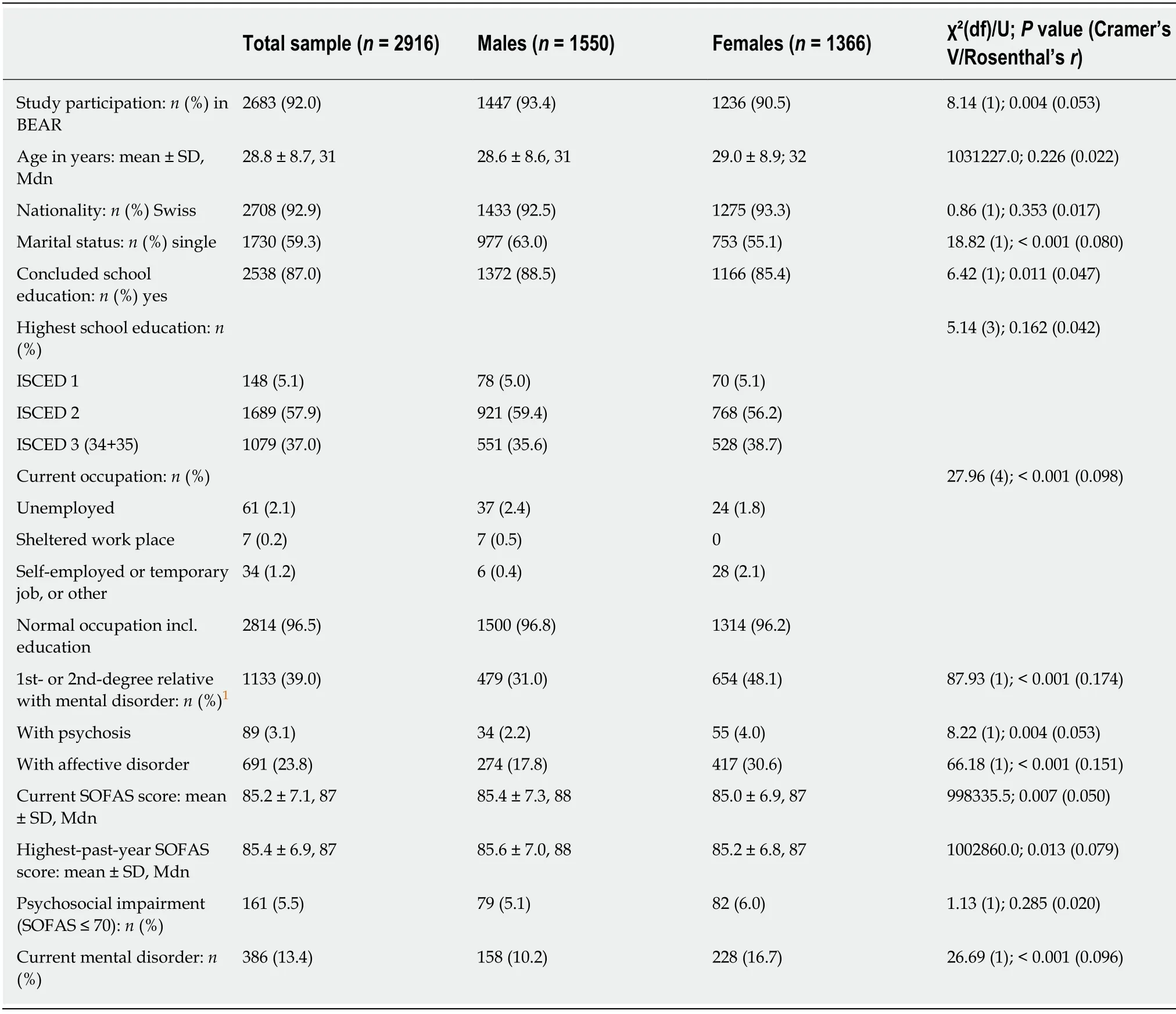
Table 2 Sociodemographic and clinical characteristics of the sample
Simple and combined effects of age and sex on CHR criteria
Contrary to in CHR symptoms, the simple age group effect on CHR and EPA criteria indicated a lower prevalence in those of age 25 and older rather than a higher frequency in the younger age groups (Tables 18-19).Similar to the findings on CHR symptoms, however, females were more likely to report CHR or EPA criteria, again with sex explaining less variance than age groups (Tables 18, 19).
In the combined models, however, and once more in contrast to CHR symptoms,age and sex entered as independent predictors only, with younger age and female gender being associated with a higher likelihood of meeting any CHR or any EPA criterion (Tables 20-21).In doing so, sex was a stronger predictor compared to age(Tables 20, 21).
Effects of age, sex, and CHR symptoms and criteria on psychosocial impairment
With the exception of speech-disorganisation APS, for which different predictors were selected in forward and backward selection (i.e., the APS in forward and the interaction of this APS with age in backward selection), age in interaction with the respective CHR symptom or criterion predicted psychosocial impairment (Tables 22-29).Only in case of perceptual BS, this interaction was further moderated by sex(Table 24).
Except for delusional APS/BIPS, the twofold interactions indicated that participants with no impairment were younger when they reported CHR symptoms or criteria compared to those not reporting these.This trend was similar but less pronounced for those with a psychosocial impairment in case of hallucinatory APS/BIPS, CHR criteria and EPA criteria, while it was opposite but less pronounced(i.e., higher age in those with both social impairment, and CHR symptoms and criteria compared to those with only psychosocial impairment) in case of any BS, any cognitive BS and any APS/BIPS.In case of delusional APS/BIPS, both participants with and without psychosocial impairment were older when they reported delusional APS/BIPS compared to when they did not report delusional APS/BIPS, with this interaction being more pronounced in those with an impairment.In case of perceptual BS, the interaction effect between age and symptoms on psychosocial impairment was more pronounced in males, in whom this interaction was similar to that of age and symptoms in case of any or cognitive BS.In females, however, both participants with and without a social impairment were younger in the presence of perceptual BS, yet without the perceivable difference in the strength of this effect that was displayed in case of hallucinatory APS/BIPS, CHR criteria and EPA criteria, indicating an absence of an age-by-perceptual BS interaction in females.
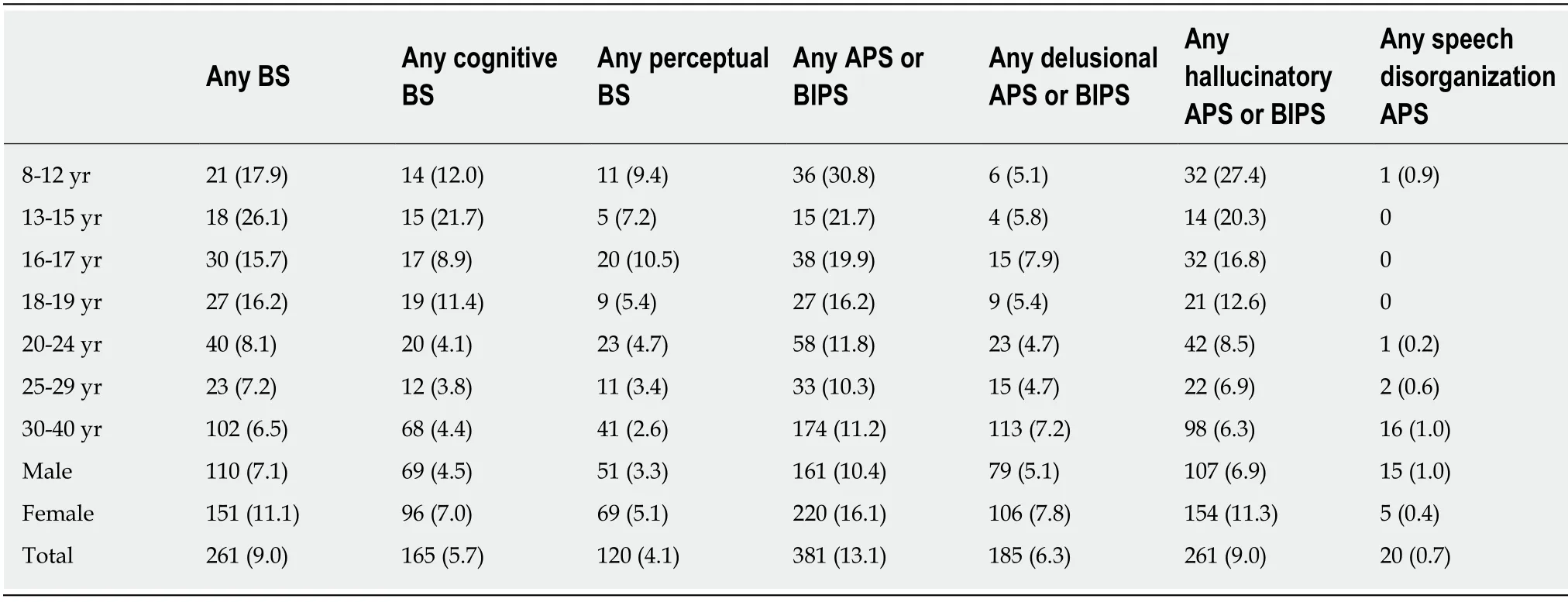
Table 3 Frequency of clinical high risk symptoms in age groups and sexes, n (% of group)
Effects of age, sex, and CHR symptoms and criteria on nonpsychotic mental disorder
Contrary to its minor role in respect to psychosocial impairment, sex was always an independent predictor of the presentation of any non-psychotic axis-I disorder according to DSM-IV (Tables 30-38).Mostly, sex was a predictor in addition to the CHR symptoms or criteria without interacting with them, in doing so, playing a lesser role (Tables 32-35, 37, 38).It was even the sole predictor of mental illness in case of any BS (Table 30), likely because the additional role of cognitive BS but not of perceptual BS was moderated by age (Table 31), indicating that mental disorder was less likely when participants with cognitive BS were younger, while in participants with mental disorder, age did not differ between those with and without cognitive BS.The additional role of speech-disorganization APS was also moderated by age (Table 36);yet, other than in case of cognitive BS, indicating that, irrespective of the presentation of mental disorder, participants without this APS were commonly younger than those with it;this age effect being more pronounced in those with mental disorder.In both models, the one with cognitive BS and the one with speechdisorganization APS, the effect of sex was greater than the effect of the age-symptom interaction (Tables 31, 36).
DISCUSSION
Differential age thresholds in CHR symptoms were reported from a much smaller subsample (n=689) of the present sample (n=2916) in the community[24,25],suggesting an age threshold of about 15/16 year-of-age for APS that was subsequently supported in clinical samples[18,19].An age threshold for perceptual BS around age of 18 years and an age threshold for cognitive BS within the first half of the twenties was found in the community[25].In any case, a higher prevalence and lesser clinical relevance of the respective CHR symptoms in the age groups below these thresholds were observed[18,19,24,25].In line with the BS concept[57,58]and current biological and cognitive behavioral models of psychosis[1,59,60], these age thresholds were interpreted as signaling a main relation of APS to the maturation of major cognitive skills and a main relation of BS to brain maturation[25].Furthermore, because of the sex differences in brain and cognitive maturation[44-47], and likely, in symptomatology associated with psychosis and the CHR states[30-39], it was anticipated that sex and age might interact, thus leading to lower age thresholds in the prevalence and clinical significance of BS and possibly APS in females compared to males[25].Hence, in our highly original study, we investigated the effects of age and sex on the prevalence of CHR criteria and symptoms and on their association with psychosocial impairment and mental ill-health in a large community sample of 8- to 40-year-olds.Overall, our results supported the influence of both age and sex on the presentation and clinical relevance of CHR symptoms and criteria;yet, these somewhat differed in their relation to CHR symptoms and criteria, and greatly differed in their interplay with CHR symptoms and criteria in relation to proxy measures of the clinical relevance,i.e., presentation of psychosocial functional impairment and non-psychotic axis I mental disorder according to DSM-IV.
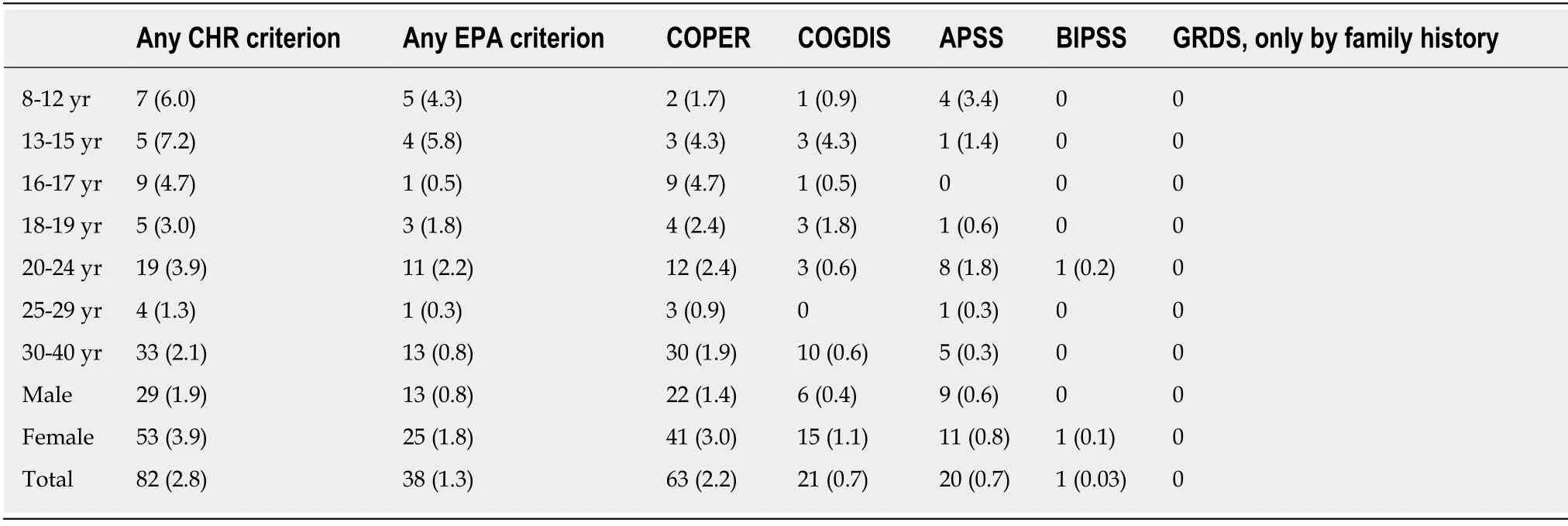
Table 4 Frequency of clinical high risk criteria in age groups and sexes, n (% of group)
Age, sex and perception-related CHR symptoms
With regard to the simple effects of age and sex, the age thresholds in BS reported from an earlier subsample[25], including the missing significance of perceptual BS in the smallest age group of 13- to 15-year-olds (n=69), was confirmed.Related to the higher power in the present much larger sample compared to the earlier smaller subsample, all reported age group effects now reached level of significance.Newly,this was also the case for a lower prevalence of perceptual BS in the largest age group of 30- to 40-year-olds (n=1560), which might indicate a continuous slow decrease with age rather than a strict age threshold in perceptual BS.Future community studies with larger samples of younger age groups or studies on clinical samples with a higher prevalence of perceptual BS are needed to decide between an age threshold related to brain maturation processes and a slow decrease in perceptual BS.A slow decrease might reflect continuously strengthened top-down processes in perception,which had been related to the longer duration of the schizophrenia prodrome with perceptual BS[61].
For hallucinatory APS/BIPS, similar age group effects showed but were more pronounced for the three young age groups and less pronounced for the 30- to 40-year-olds.Thus, in contrast to the earlier analyses of a smaller subsample of the present sample, no difference in age thresholds between perceptual BS and hallucinatory APS/BIPS was found.Symptom capture studies, in particular of auditory hallucinations, indicated a pattern of increased coupling among the auditory, language and striatal regions, while resting state studies suggest that the default mode network might be involved in both auditory and visual hallucinations[87].Further, next to these neurobiological findings, also unstable memories, impaired source monitoring, and poor top-down attention were suggested to play a role in the formation of hallucinations[62,63].
Thus, age group effects indicate that brain maturation processes, in particular of temporal and occipital regions, might play a role in the occurrence of both perceptual BS and hallucinatory BS, with sex-dependent maturation of cognitive abilities[45,64,65]such as memory, source monitoring and top-down attention further impacting on the appraisal, and thereby the severity of hallucinatory experiences.While this might explain the age group effects, it does not explain the simple sex findings, with higher prevalence rates in females.However, the interaction of age and sex in perceptual BS and hallucinatory APS/BIPS indicated that, in line with our initial assumption, in particular younger females were prone to report perceptual BS, whereas, contrary to our expectations, hallucinatory APS/BIPS were more frequently reported by females with advancing age.Thus, brain maturation processes might be more pronounced in perceptual BS that, for this reason, are also independently influenced by sex, while sex differences in neurocognitive mechanisms might further moderate hallucinatory experiences, thereby protecting hallucination-prone females for some time.However,to better understand age and sex effects in perception-related CHR symptoms more research employing both sophisticated neurobiological and psychopathological assessments are needed[66].
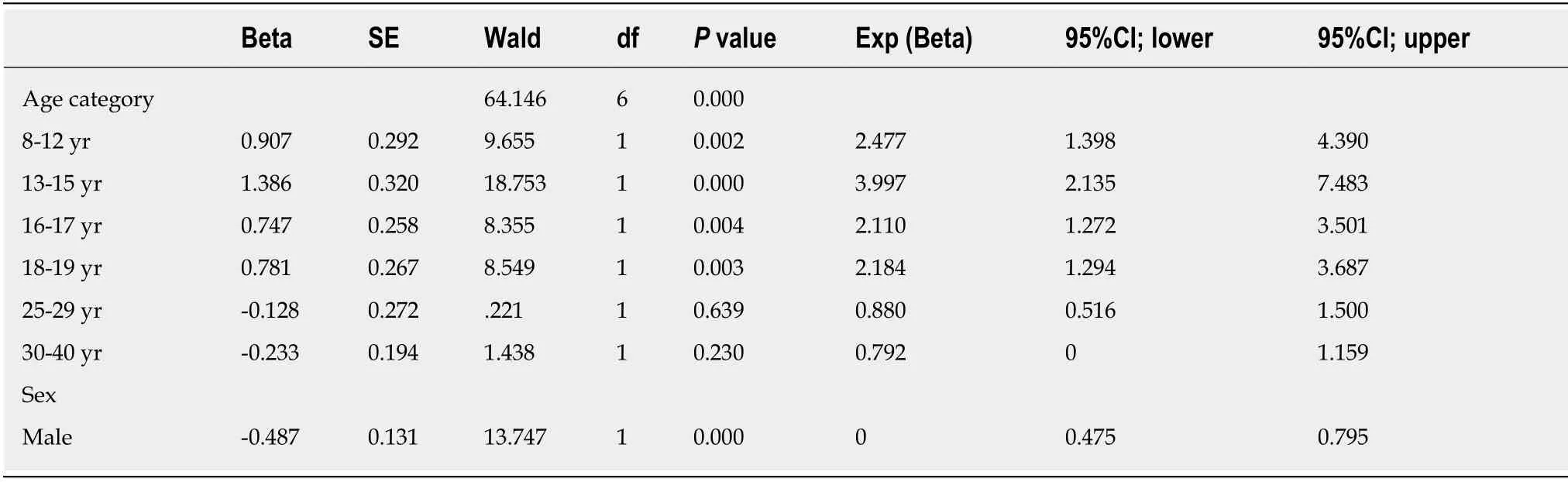
Table 5 Simple effects of age group and sex on presence of ≥ 1 of the 11 basic symptoms
Age, sex and cognition-related CHR symptoms
Compared to perceptual BS, more pronounced effects of age group and, relatedly, a more distinct age threshold showed for cognitive BS, which was also indicated by a higher amount of explained variance (39% for perceptualvs47% for cognitive BS).This supports the earlier notion of cognitive BS being related to brain maturation processes, particularly of frontal regions[28].As in earlier studies[24,19], the regression model of delusional APS/BIPS was not significant and revealed little effects of age on prevalence of delusional APS/BIPS, except for a newly detectable marginally significant effect in 30- to 40-year-olds, indicating a higher prevalence [Exp[Beta]=1.57(1.01-2.53)].In the earlier less powered study[24], however, an increased prevalence was also indicated in this age group by exhibiting the smallestPvalue that, however,had not even approached a statistical trend (P=0.19;Exp[Beta]=1.82 (0.74-4.48))[24].
Interestingly, although no significant age model was detected for the newly separately considered speech-disorganization APS, the result also pointed towards a slightly higher prevalence in the 30- to 40-year-olds [P=0.114;Exp[Beta]=5.10 (0.67-38.54)], despite the low number of altogether only 20 participants scoring positively on it.This age effect was again apparent in the mental disorder model including speech-disorganization APS;in which, in addition to female sex being related to mental disorders, older age was associated with the presence of speechdisorganization APS, in particular in those with mental disorder.Thus the interaction of age and speech-disorganization APS contributed to the prediction of mental disorders, though less than sex alone.Accordingly, contrary to all other associations between CHR symptoms and criteria, males were more likely to display speechdisorganization APS.These findings are somewhat in line with brain studies on cognitive and language functions, and their brain structure and function that reported a larger effect of sex compared to age[64,67-69]with little interaction between the two.A link of disturbed white matter in the cerebral language pathways with disorganized speech and formal thought disorder, respectively, in schizophrenia was suggested by findings of structural abnormalities predominantly in the left superior temporal gyrus, angular gyrus, inferior operculum and orbitofrontal cortex, and of functional abnormalities in the left superior and middle temporal gyrus[70-75].These studies on clinical samples used clinical ratings or speech-samples to evaluate degree of disorganized speech, while the studies of age and sex effects on brain structures and functions in non-clinical samples commonly used objective neurocognitive measures[64,69].These neurocognitive assessments commonly correlate to a small-tomoderate degree with speech disorganization[76];thus, the age and sex effects reported in non-clinical samples might apply as well - an assumption further supported by our findings.
Other than observable speech disorganization, cognitive BS did not correlate to neurocognitive measures[77].And contrary to speech-disorganization APS but similar to all other CHR symptoms and criteria, cognitive BS were related to female sex and most prevalent in younger age groups, in which age and sex acted independent of each other, with sex having a more pronounced impact on the report of cognitive BS.Furthermore, report of cognitive BS was increasingly related to functional impairment and presentation of a mental disorder with advancing age, in doing so exhibiting a divergent model for mental disorders compared to speech-disorganization APS,although female sex was related to mental disorders in both models.By definition,cognitive BS are spontaneously and immediately recognized as disturbances of one’s own cognitive processes that differ from what is considered to be the “normal”mental self, and are not necessarily observable by others in terms of odd thinking,disturbed speech, or formal thought disorder[15,16,57,58].For these phenomenological differences, cognitive BS formed a single factor in a recent dimensional analysis, while speech-disorganization APS joined other disorganization symptoms in a different factor;in doing so, the cognitive BS factor was positively linked to the disorganized factor and possibly acted as a facilitator[78].With regards to the neurobiological underpinnings of cognitive BS, targeted studies are still missing[58]but, for the described differences to speech-disorganization APS, can be assumed to partly differ from those on formal thought disorders, especially with regard to the languageunrelated cognitive BS.
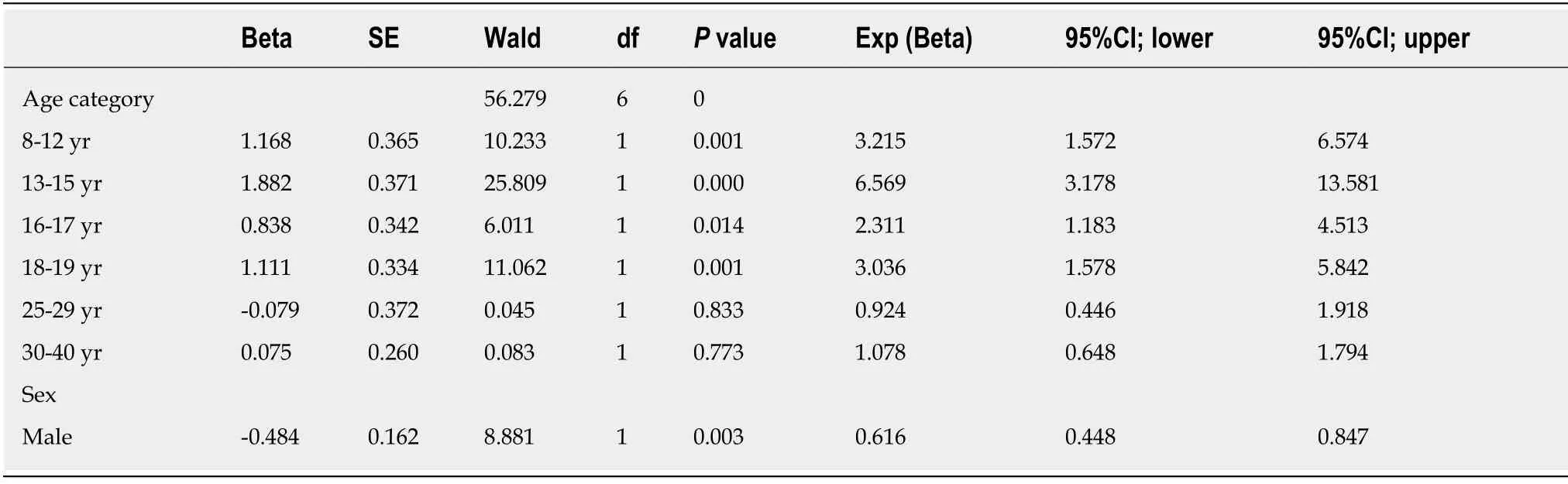
Table 6 Simple effects of age group and sex on presence of ≥ 1 of the 9 cognitive basic symptoms
Sex and prevalence of APS/BIPS
With regard to sex, based on prevalence data on psychoses, we had expected more males to report CHR symptoms, in particular APS/BIPS, yet, this only showed at statistical trend level for speech-disorganization APS that were almost three times more frequent in men compared to females.In line with the literature on CHR samples and samples referred to specialized early detection services[20,31,34,36,38], more severe APS/BIPS, and more cognitive and perceptual BS were reported in females.This difference between more males within our studied age range presenting with frank psychotic disorder and more females presenting with CHR symptoms, might be related to differences in symptomatic sex effects in referral and converter samples of early detection services, and relatedly, in psychosis-specificity of sex effects[65].Sex effects in referral or baseline APS/BIPS samples, both with an assumable high rate of non-conversion of at least 60%[13], were argued to reflect more general sex effects on psychopathology that included more frequent and/or severe positive psychotic symptoms (especially paranoid) in females[26,28,29].This was also reported for some CHR samples[31], though rather with respect to hallucinatory than to delusional APS/BIPS[34,38].The working of more general sex effects - that impacts on the prevalence rates of mental disorders and their age of first presentation and is considered important for the understanding of causal mechanisms[79,80]- also has to be expected in our community sample and, consequently, might explain the higher prevalence of CHR symptoms in females.
A higher prevalence of APS in females with a very similar Exp[Beta] (or Odds Ratio) as found in our study [0.63 (0.42-0.93)vs0.60 (0.49-0.75)] was recently reported from a Brazilian convenience sample of 6- to 14-year-olds from the community[39].Yet,in this study, the prevalence rate of APS as assessed with Comprehensive Assessment of At-Rik Mental States (CAARMS)[81]was only 5.7%, and thus, much lower than our 13.1%-rate.In the Brazilian study, however, clinical relevance defined as “would raise concern about the child’s mental health status in a clinical setting”[39]was emphasized,and more than three quarters of children fulfilled this criterion.While the CAARMS differs from the SIPS in the frequency and onset criteria, APS/BIPS cover largely the same phenomena in both assessments that both rate symptom severity at a 7-point scale with APS/BIPS being rated with a score of “≥ 3”[82].In the CAARMS, a score of“5” requires “may result in some change in behaviour, but minor” for delusional APS,which is not required in scores of “3” and “4”.A score of “4” only requires “Able to give plausible explanation for experience.May be associated with mild distress.” For hallucinatory APS/BIPS, scoring thresholds are similarly high for impact on behaviour and conviction.Thus milder, easily dismissed, non-distressing experiences at the level of APS that did not impact on behaviour, and, consequently, likely would not raise concerns about the mental state (i.e., lower CAARMS scores and, likewise,lower SIPS scores[82]), might not have been rated in the Brazilian study[39].Except for the rarely rated grandiose ideas (n=8), a score of “3” in the SIPS accounted for 60.0%to 72.3% of APS/BIPS-ratings in the remaining four P-items of the SIPS in our sample.Thus, this possible difference in scoring might account for some of the difference in prevalence rates of these two community studies.Furthermore, for developmental reasons, hallucinatory experiences that had the highest prevalence of APS in our sample might not be reliable assessable in 6- and 7-year-old children[17,83], and consequently, not rated in the Brazilian sample, this further decreasing the overall prevalence rate of APS.
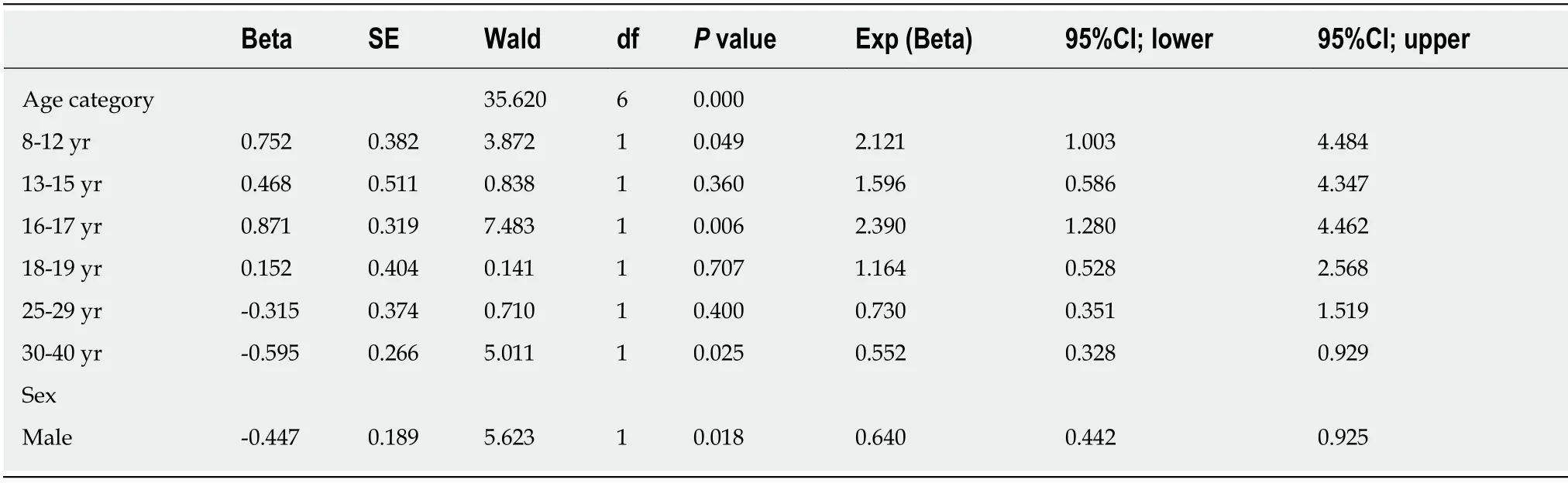
Table 7 Simple effects of age group and sex on presence of ≥ 1 of the 2 perceptual basic symptoms
Age, sex and CHR criteria
CHR criteria, at prevalence rates of 2.8% for any CHR and 1.3% for any EPA criterion,were far more infrequent compared to CHR symptoms, indicating that CHR symptoms are frequently not meeting onset and frequency requirements of CHR criteria (Table 1), mostly by infrequent occurrence[24,26,48,49].Similar to the majority of CHR symptoms, CHR and EPA-recommended CHR criteria exhibited effects of both age and sex, with age group effects explaining more variance than sex effects.Different to most CHR symptoms, however, the age thresholds for CHR and EPA criteria around age of 24/25 years were higher and indicated a significantly lower prevalence above this age rather than a higher prevalence below it.In line with these effects of age groups, the combined analyses of age and sex indicated independent effects of these with younger age and, more pronounced, female sex being associated with meeting the criteria.This slightly higher age threshold might indicate that, in case of the above discussed aberrant processes in both neurocognitive and neurobiological maturation, maturation disturbances underlying CHR symptoms have to persist and possibly increase before impacting sufficiently on psychopathology to meet CHR criteria[25,46,84].
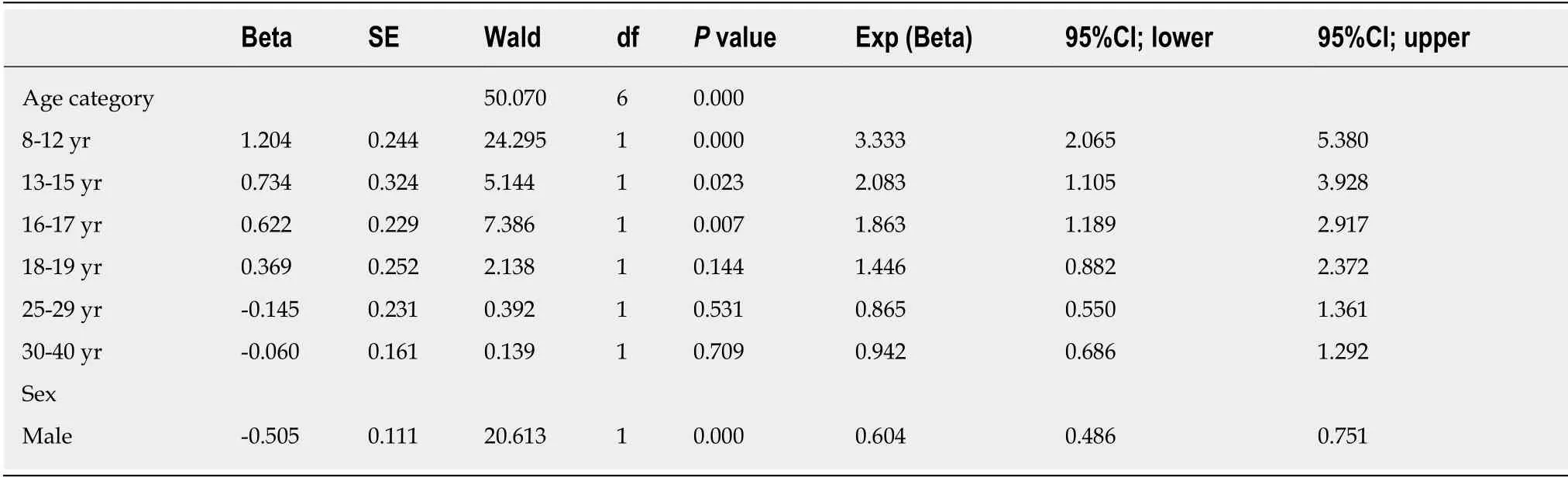
Table 8 Simple effects of age group and sex on presence of ≥ 1 of the 5 attenuated psychotic symptoms or brief intermittent psychotic symptoms
Age, sex and clinical relevance of CHR symptoms and criteria
Our study confirmed the clinical relevance of CHR symptoms and criteria in terms of being selected as a predictor of both functional impairment and mental disorder,which were used as proxy measures of clinical relevance.Furthermore, it confirmed the earlier reported stronger association of CHR symptoms and criteria with functional impairment in comparison to mental disorder[49], in terms of larger explained variance of the functional impairment models compared to the corresponding mental disorder models.This indicates that CHR symptoms and criteria possess clinical relevance in themselves and are not merely a global indicator of mental ill-health[49,85].
A most striking global difference emerged with respect to the interplay of sex, age,and CHR symptoms and criteria in association to these two proxy measures of clinical relevance.Social impairment was commonly predicted by the interaction between age, and CHR symptoms and criteria, with only perceptual BS being additionally moderated by sex.In doing so, in all CHR symptoms but delusional APS/BIPS as well as in CHR/EPA criteria, younger age in the presence of CHR symptoms and criteria was associated with good psychosocial functioning.With regard to the mental disorder models, CHR symptoms and criteria and, to a lesser degree, sex were commonly independent predictors of mental disorders, with only cognitive BS and speech-disorganization APS being additionally moderated by age;in doing so, the interaction was a weaker predictor compared to sex.The role of sex indicated in all instances more females with current non-psychotic mental disorders.This sex effect in point-prevalence of mental disorders is in line with higher 12-month point but not lifetime prevalence rates of mental disorders in females[86], and is very likely independent of the effects of CHR symptoms and criteria.Follow-up of the sample will demonstrate in future to what degree CHR symptoms and, more importantly,CHR and EPA criteria are related to the development of psychotic and psychosisspectrum disorders.
Strengths and limitations
Our study has several strengths and limitations.A clear strength of our study is the large sample size - albeit the disproportionate subsample sizes with lesser children and adolescents compared to adults, that must be considered a limitation.Another strength is the assessment of CHR symptoms and criteria in a way as done in clinical samples,i.e., using standard instruments for the assessment of CHR states, carried out by well-trained and supervised clinical psychologists in clinical semi-structured interviews.Although this was done via the telephone in the BEAR study and face-toface in the BEAR-Kid study, an earlier feasibility study that had compared telephone and face-to-face assessment of CHR symptoms and criteria in a fully crossed design reported good correspondence between this two assessment modes, especially when only focussing on presentation of CHR symptoms and criteria[50]as done in the present study.Thus, the reported differences between children and adolescents and adults,i.e., the effects of age, are likely genuine and not only caused by an assessment bias.
Albeit the similar recruitment procedure in the BEAR and the BEARS-Kid study that was based on random sampling from the population register, the lower response rate in the BEARS-Kid study might limit its representativeness.The BEAR sample,however, was already reported to be well-representative[49].
Despite the large sample size, however, some CHR symptoms and criteria occurred in too small numbers to meet the minimum of five outcome events per predictor variable in all regression analyses[87].Regression analyses were consequently affected by this, in particular, simple age group effects as well as combined effects of age, sex,and CHR symptoms and criteria on the presentation of psychosocial impairment and of mental disorders in case of speech-disorganization APS, and also regression analyses on simple age effects in case of EPA criteria.Thus, these results might be of limited reliability and should be considered only with caution.
Earlier studies had only distinguished hallucinatory APS/BIPS from delusional and speech-disorganization APS/BIPS[19,23,24].Thus, in light of the unique findings on speech-disorganization APS that fit well to the findings on cognitive BS, the separate consideration of delusional and speech-disorganization APS/BIPS can be regarded as another strength of our study.
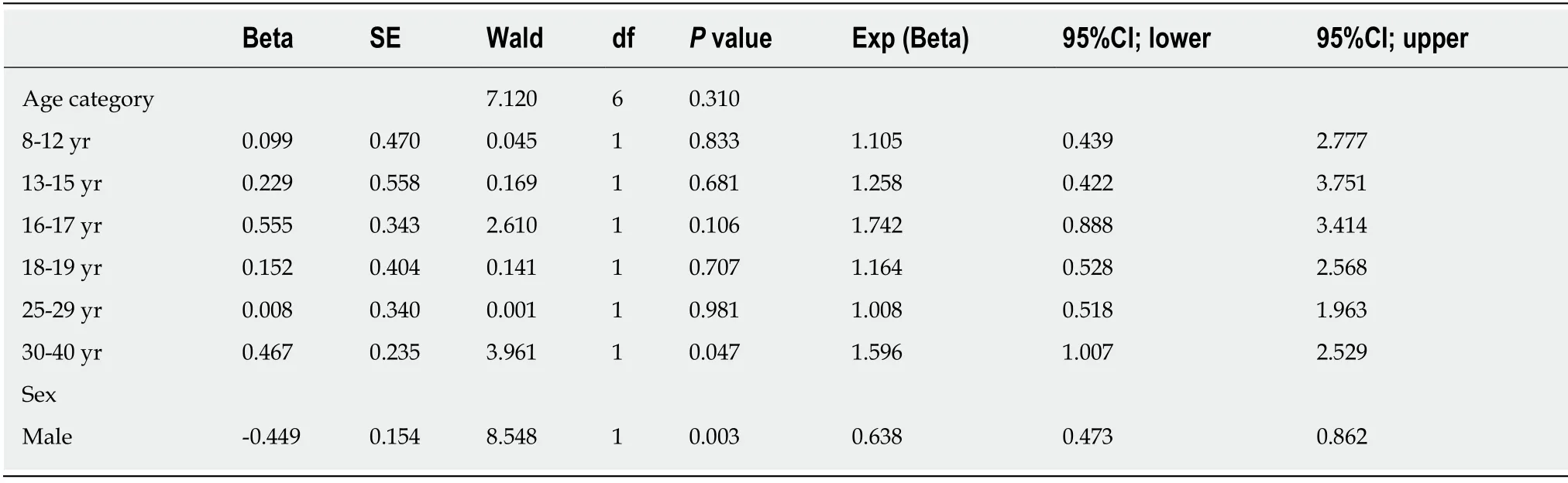
Table 9 Simple effects of age group and sex on presence of ≥ 1 of the 3 delusional attenuated psychotic symptoms or brief intermittent psychotic symptoms
Conclusion
Our results on a community sample indicate that age and sex impact on the prevalence of CHR symptoms and criteria as well as on their association with proxy measures of clinical relevance,i.e., the presentation of functional impairment and of non-psychotic mental disorder.In doing so, age and sex moderate CHR symptoms and criteria in various ways, these differences opening ways to better understand their causal pathways.Thus, further efforts at unravelling causal pathways of psychosis, at biomarker discovery and at early therapeutic intervention should consider effects of both sex and age[17,24,25,46,84].
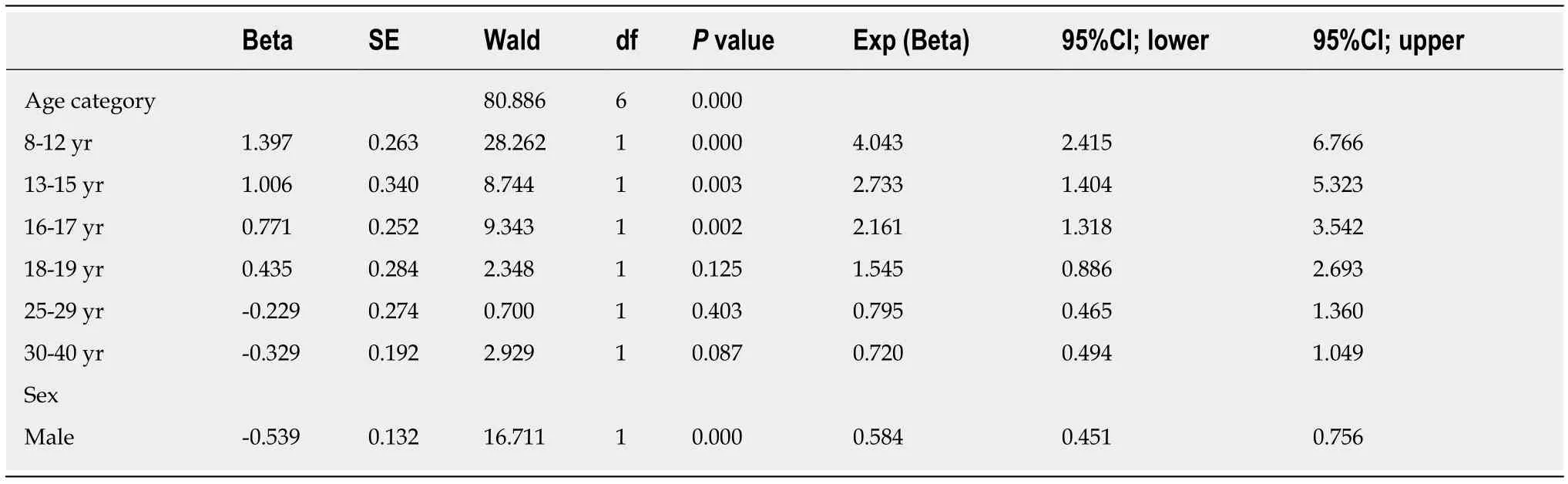
Table 10 Simple effects of age group and sex on presence of hallucinatory attenuated psychotic symptoms or brief intermittent psychotic symptoms
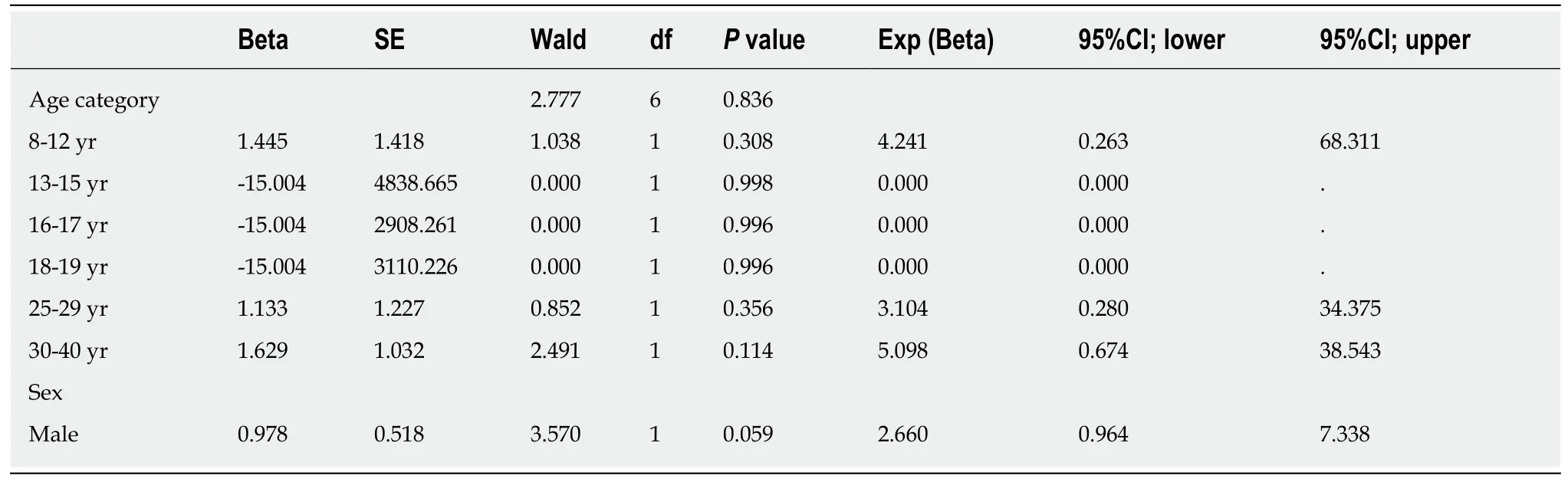
Table 11 Simple effects of age group and sex on presence of speech-disorganization attenuated psychotic symptoms
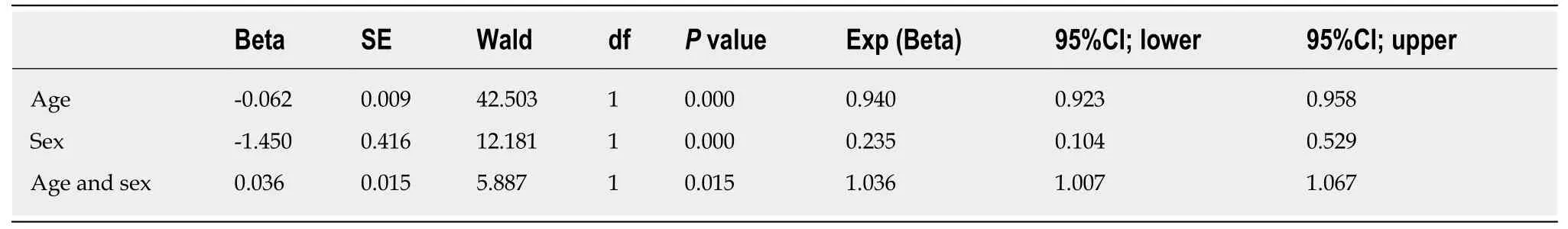
Table 12 Combined effects of selected age and sex predictors on presence of ≥ 1 of the 11 basic symptoms
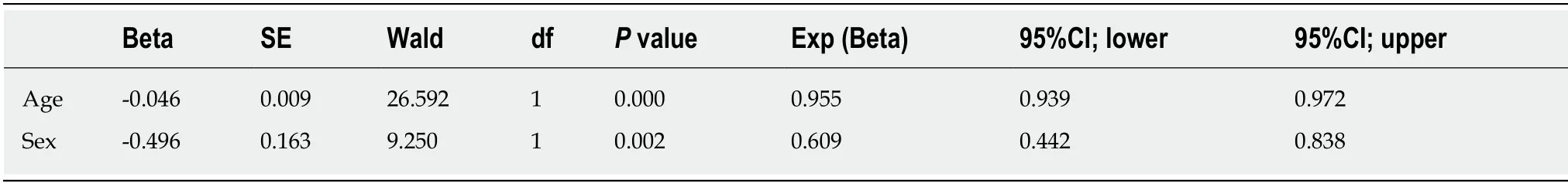
Table 13 Combined effects of selected age and sex predictors on presence of ≥ 1 of the 9 cognitive basic symptoms
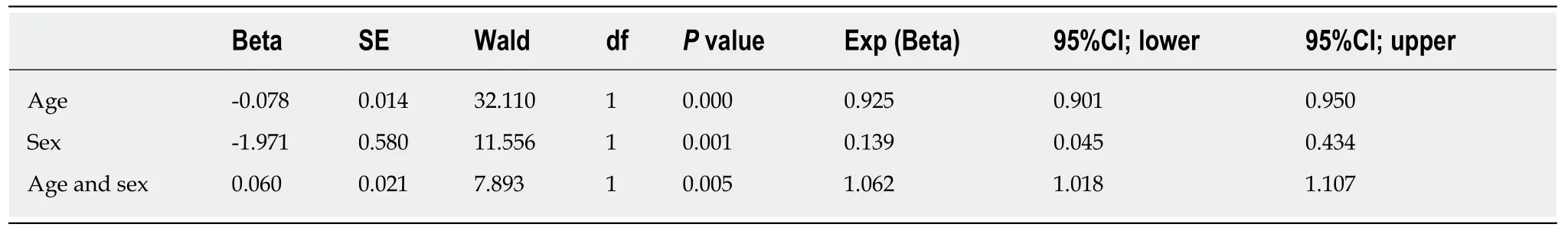
Table 14 Combined effects of selected age and sex predictors on presence of ≥ 1 of the 2 perceptual basic symptoms
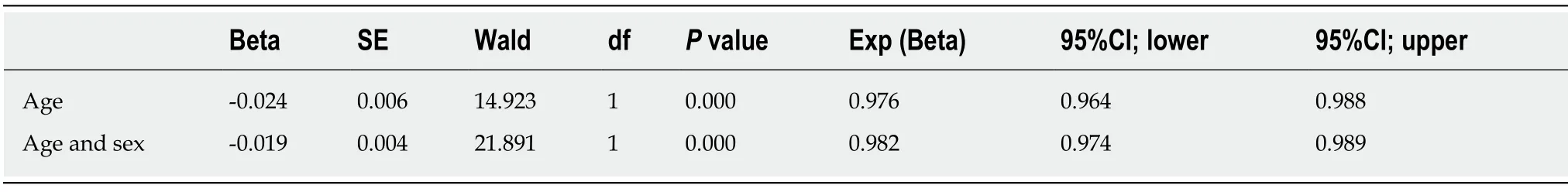
Table 15 Combined effects of selected age and sex predictors on presence of ≥ 1 of the 5 attenuated psychotic symptoms or brief intermittent psychotic symptoms
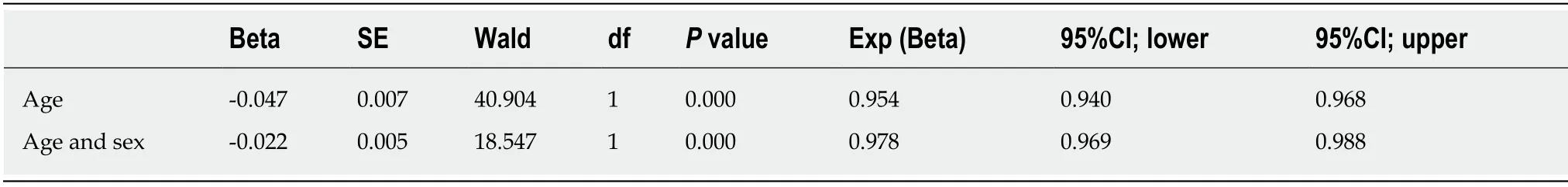
Table 16 Combined effects of selected age and sex predictors on presence of hallucinatory attenuated psychotic symptoms or brief intermittent psychotic symptoms
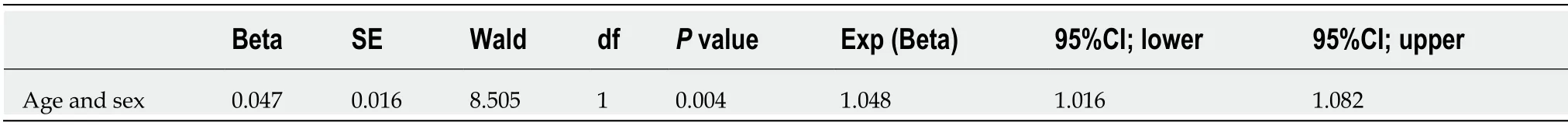
Table 17 Combined effects of selected age and sex predictors on presence of speech-disorganization attenuated psychotic symptoms
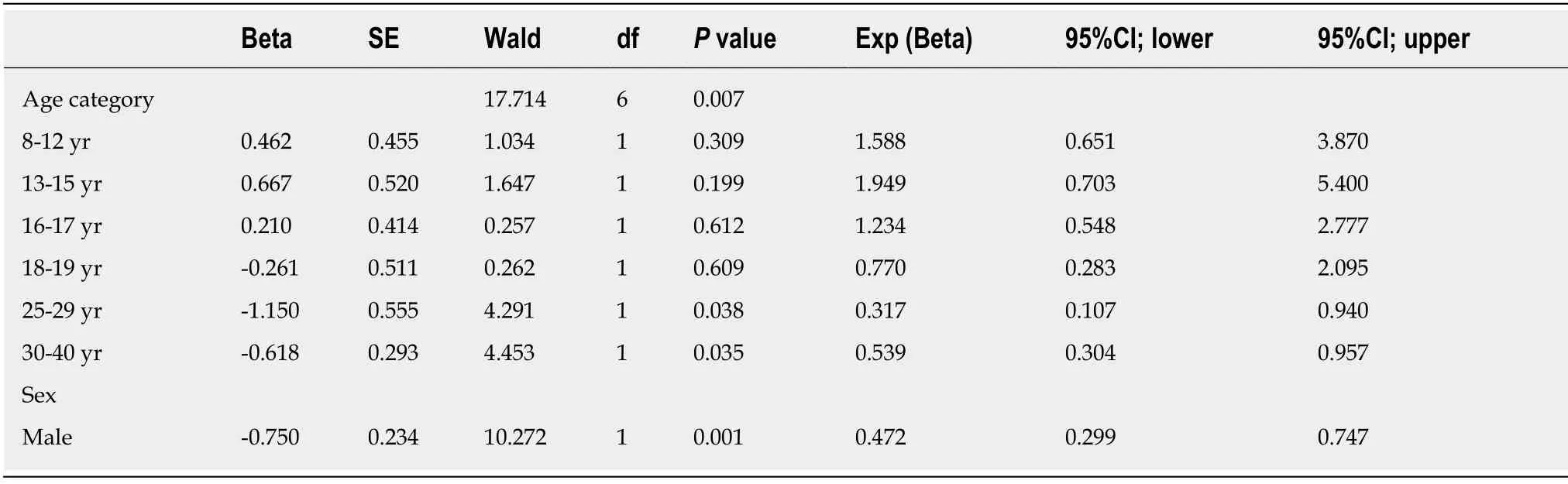
Table 18 Simple effects of age group and sex on presence of ≥ 1 clinical high risk criterion
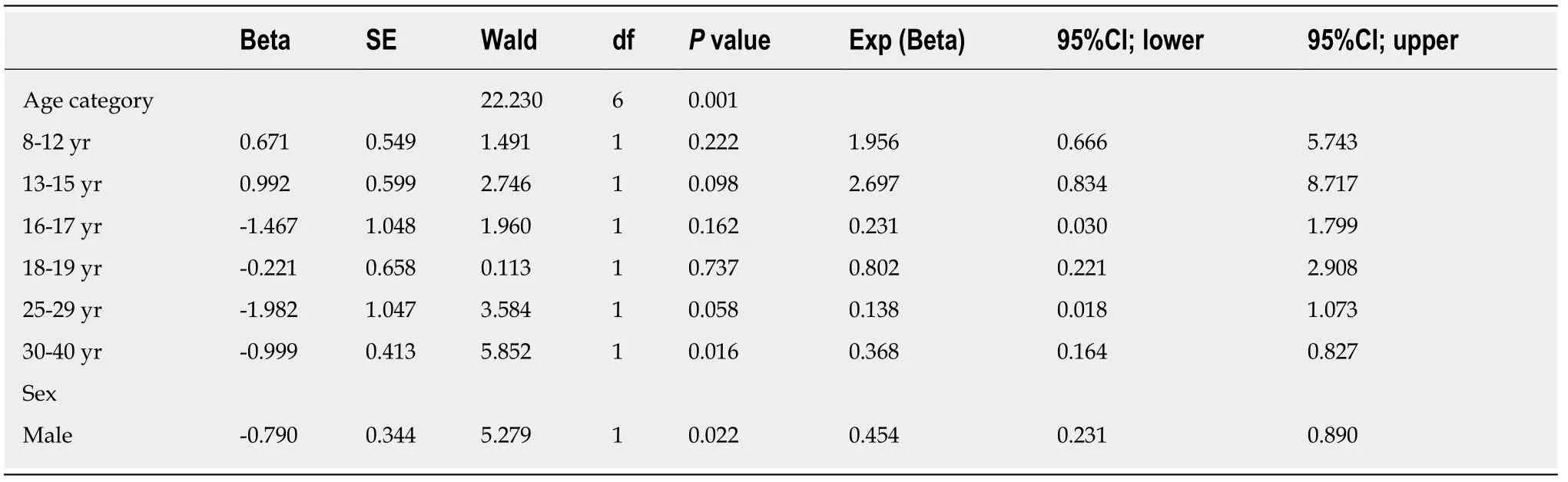
Table 19 Simple effects of age group and sex on presence of ≥ 1 European Psychiatric Association-recommended clinical high risk criterion
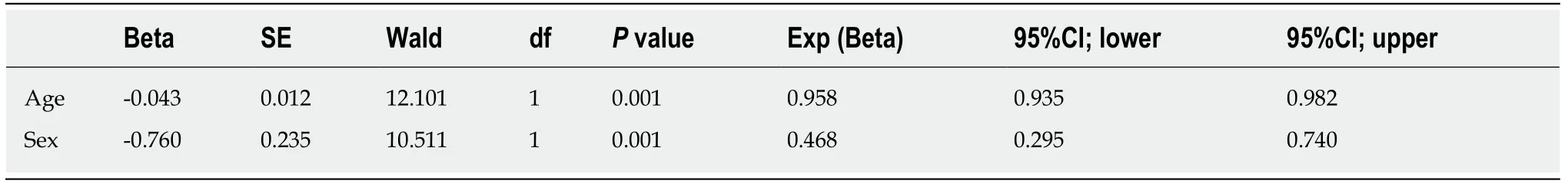
Table 20 Combined effects of selected age and sex predictors on presence of ≥ 1 clinical high risk criterion
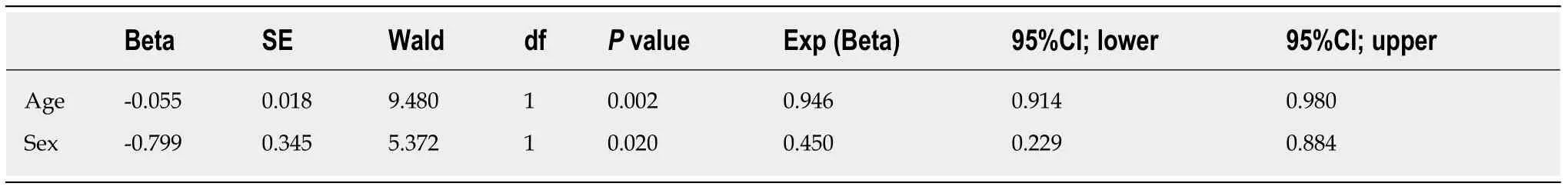
Table 21 Combined effects of selected age and sex predictors on presence of ≥ 1 European Psychiatric Association-recommended clinical high risk criterion
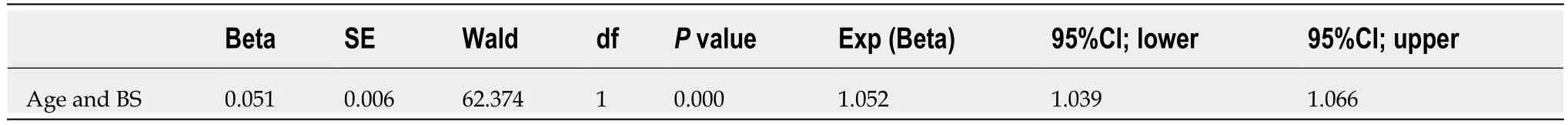
Table 22 Combined effects of selected age, sex and symptoms (≥ 1 of 11 basic symptoms) predictors on presence of psychosocial impairment (Social and Occupational Functioning Assessment Scale ≤ 70)
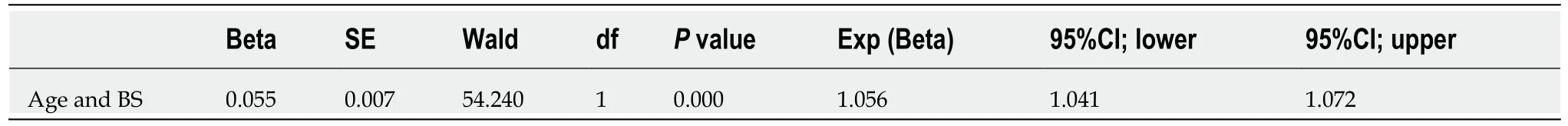
Table 23 Combined effects of selected age, sex and symptoms (≥ 1 of 9 cognitive basic symptoms) predictors on presence of psychosocial impairment (Social and Occupational Functioning Assessment Scale ≤ 70)

Table 24 Combined effects of selected age, sex and symptoms (≥ 1 of 2 perceptual basic symptoms) predictors on presence of psychosocial impairment (Social and Occupational Functioning Assessment Scale ≤ 70)
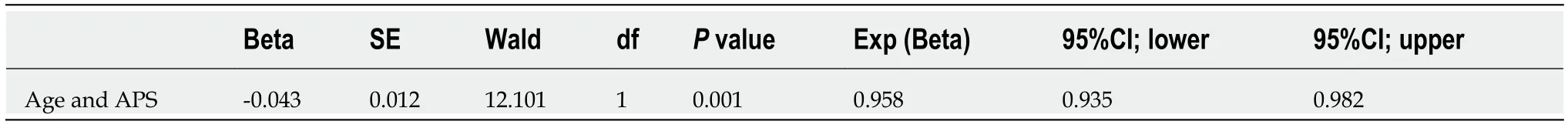
Table 25 Combined effects of selected age, sex and symptoms (≥ 1 of 5 attenuated psychotic symptoms/brief intermittent psychotic symptoms) predictors on presence of psychosocial impairment (Social and Occupational Functioning Assessment Scale ≤ 70)
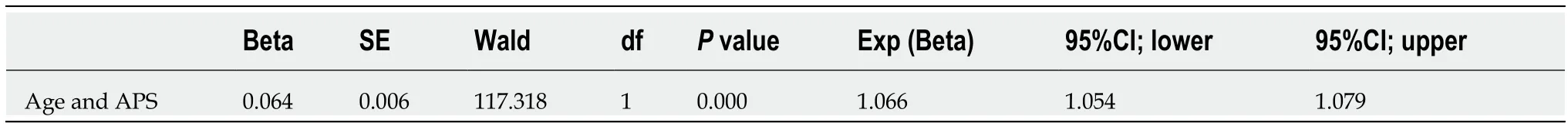
Table 26 Combined effects of selected age, sex and symptoms (≥ 1 of 3 delusional attenuated psychotic symptoms/brief intermittent psychotic symptoms) predictors on presence of psychosocial impairment (Social and Occupational Functioning Assessment Scale ≤ 70)
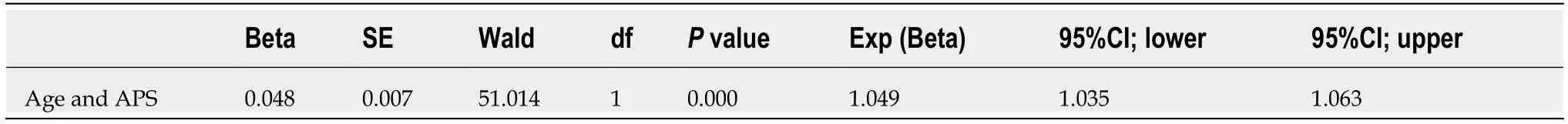
Table 27 Combined effects of selected age, sex and symptoms (hallucinatory attenuated psychotic symptoms/brief intermittent psychotic symptoms) predictors on presence of psychosocial impairment (Social and Occupational Functioning Assessment Scale ≤ 70)
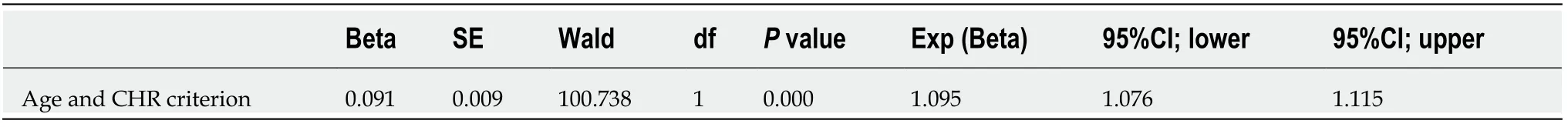
Table 28 Combined effects of selected age, sex and criteria (≥ 1 clinical high risk criterion) predictors on presence of psychosocial impairment (Social and Occupational Functioning Assessment Scale ≤ 70)
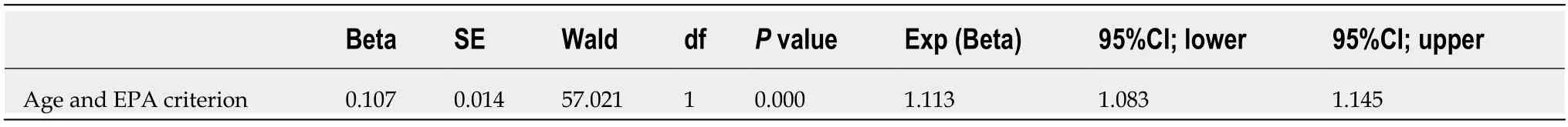
Table 29 Combined effects of selected age, sex and criteria (≥ 1 European Psychiatric Association criterion) predictors on presence of psychosocial impairment (Social and Occupational Functioning Assessment Scale ≤ 70)
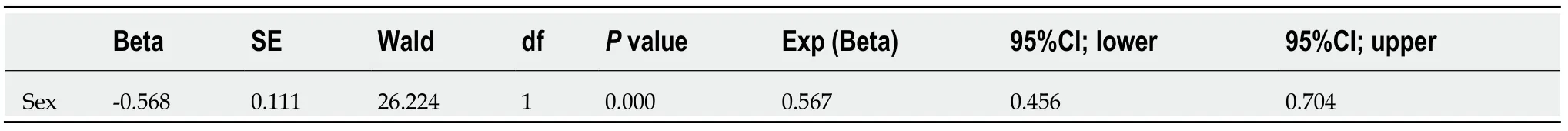
Table 30 Combined effects of selected age, sex and symptoms (≥ 1 of 11 basic symptoms) predictors on presence of any non-psychotic axis-l disorder
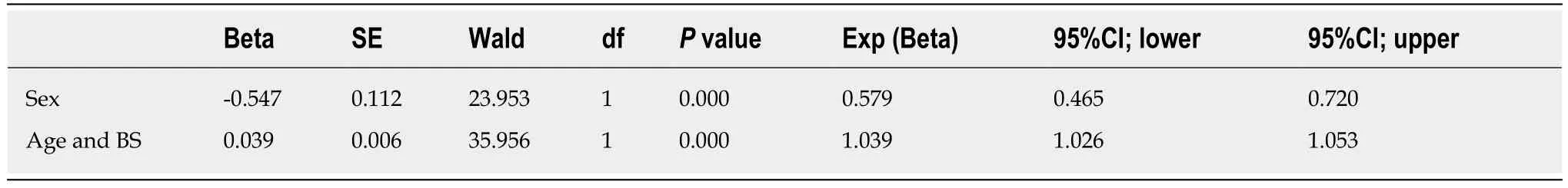
Table 31 Combined effects of selected age, sex and symptoms (≥ 1 of 9 cognitive basic symptom) predictors on presence of any nonpsychotic axis-l disorder
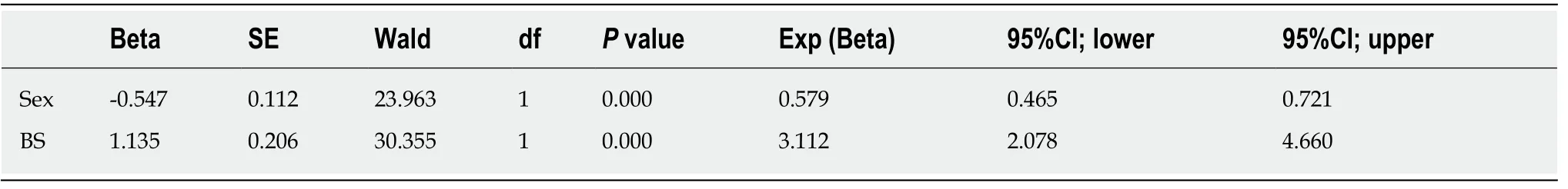
Table 32 Combined effects of selected age, sex and symptoms (≥ 1 of 2 perceptual basic symptoms) predictors on presence of any nonpsychotic axis-l disorder
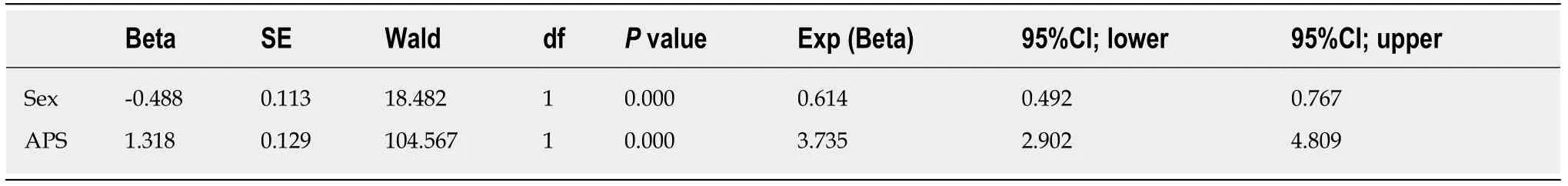
Table 33 Combined effects of selected age, sex and symptoms (≥ 1 of 5 attenuated psychotic symptoms/brief intermittent psychotic symptoms) predictors on presence of any non-psychotic axis-l disorder
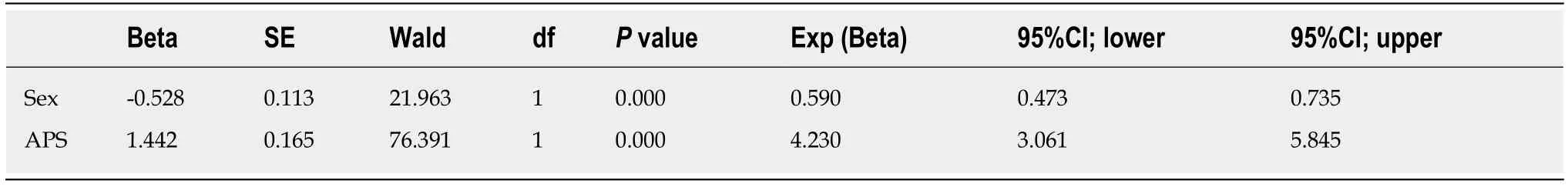
Table 34 Combined effects of selected age, sex and symptoms (≥ 1 of 3 delusional attenuated psychotic symptoms/brief intermittent psychotic symptoms) predictors on presence of any non-psychotic axis-l disorder
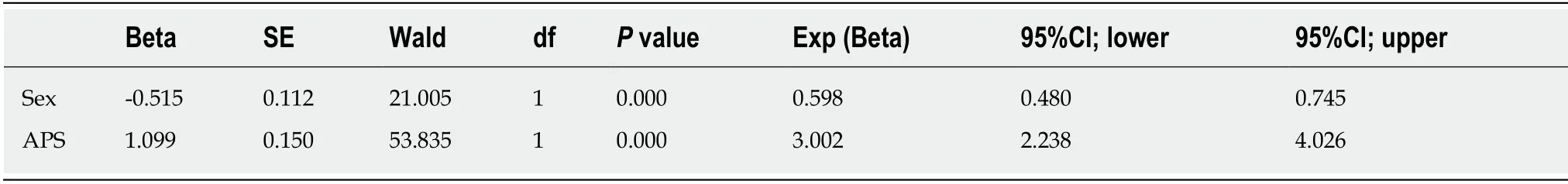
Table 35 Combined effects of selected age, sex and symptoms (hallucinatory attenuated psychotic symptoms/brief intermittent psychotic symptoms) predictors on presence of any non-psychotic axis-l disorder
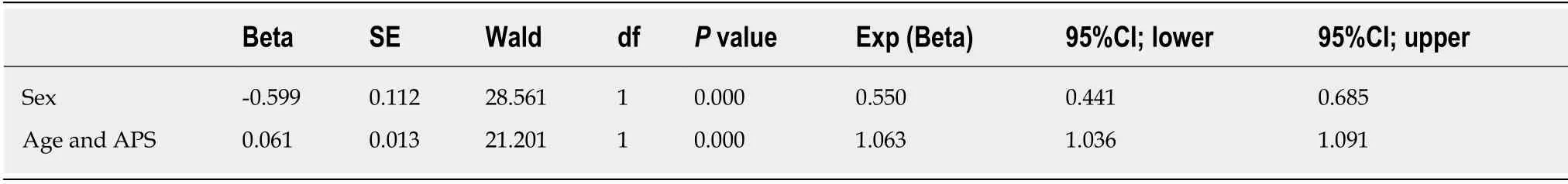
Table 36 Combined effects of selected age, sex and symptoms (speech-disorganization attenuated psychotic symptoms) predictors on presence of any non-psychotic axis-l disorder
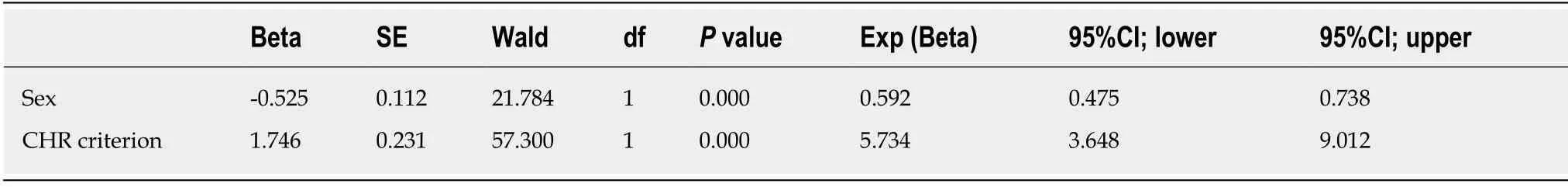
Table 37 Combined effects of selected age, sex and criteria (≥ 1 clinical high risk criterion) predictors on presence of any non-psychotic axis-l disorder
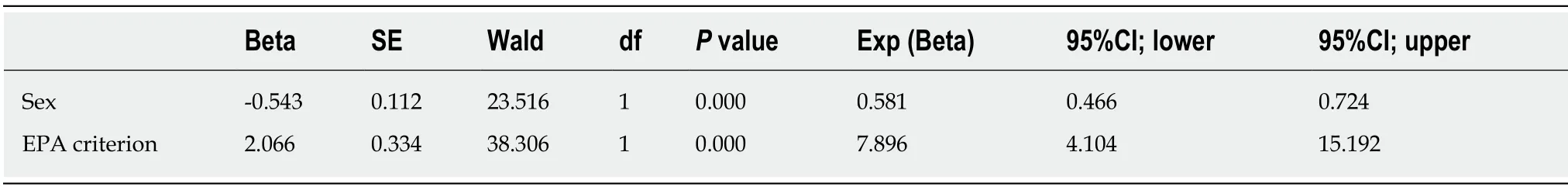
Table 38 Combined effects of selected age, sex and criteria (≥ 1 European Psychiatric Association criterion) predictors on presence of any non-psychotic axis-l disorder
ARTICLE HIGHLIGHTS
Research background
Age and sex are crucial aspects in neurodevelopment and are partly interrelated, presenting as important factors in mental disorders related to neurodevelopment.One example of these disorders are psychotic disorders whose age-at-onset and type (affectivevsnon-affective) are influenced by sex.Furthermore, in community samples, clinical high risk (CHR) symptoms and criteria that are currently used for an early detection of psychosis,i.e., attenuated and transient psychotic as well as cognitive and perceptual basic symptoms, were reported to be more frequent and less clinically relevant in children and adolescents in whom CHR criteria are also related to lower rates of conversion to psychosis.
Research motivation
From the differences in these age thresholds,i.e., around age 16 for attenuated psychotic symptoms, and around age 18 and 23 for perceptual and cognitive basic symptoms, it was speculated that sex differences in brain and cognitive maturation might lead to lower age thresholds in the clinical significance of BS and possibly APS in females compared to males.Yet,studies on the interaction of age and sex on CHR symptoms and criteria are lacking.
Research objectives
The main objective was to examine the association of age and sex on the presentation and clinical relevance of clinical high-risk criteria and their constituting symptoms in a large community study of 8- to 40-year-olds.
Research methods
We investigated the effect of both age and sex on the prevalence of CHR criteria and symptoms and on their association with psychosocial impairment and mental disorder in a community sample ofn=2916 8- to 40-year-olds.The sample was composed of community participants in two studies:The “Bern Epidemiology At-Risk” (BEAR) study and the “Binational Evaluation of At-Risk Symptoms in Children and Adolescents” (BEARS-Kid) study.Both studies used a stratified sampling method to obtain a representative sample of 7370 people aged 16-40 years in the BEAR study (response rate:63.4%) and of 980 minors aged 8-17 years in the BEARS-Kid study (response rate:32.6%) from citizens of the Swiss Canton of Bern.
Research results
Five hundred forty-two (18.6%) participants reported any CHR symptom;of these, 261 (9.0%)participants reported any one of the 11 criteria relevant cognitive and perceptual basic symptoms, and 381 (13.1%) any one of the five attenuated or transient psychotic symptoms.Fewer participants met any one of the four symptomatic CHR criteria (n=82, 2.8%).Both age and sex were significantly associated with CHR symptoms and criteria, mostly by younger age and female sex.Though slightly differing between symptom groups, age thresholds were detected around the turn from adolescence to adulthood,i.e., around age 18;they were highest for cognitive basic symptoms and CHR criteria,i.e., around age 23.With the exception of the infrequent attenuated psychotic symptom “speech disorganization”, the interaction of age with CHR symptoms and criteria predicted functional impairment;whereas, independent of each other, sex and CHR symptoms mostly predicted mental disorders.Only once, in case of functional impairment, an interaction of both age and sex with CHR symptoms - perceptual basic symptoms - became significant.
Research conclusions
Next to confirming the important role of age and sex in the prevalence and clinical relevance of CHR symptoms and criteria, their differential relations to CHR symptoms reveal important insight in possible causal pathways.
Research perspectives
In psychosis research, future efforts at unravelling causal pathways of psychosis, at biomarker discovery and at early therapeutic intervention should consider effects of both sex and age.
ACKNOWLEDGEMENTS
The authors thank our Australian colleague, Mrs.Madelyn Thomson, for her careful language assistance.