Mobile phones in the orthopedic operating room: Microbial colonization and antimicrobial resistance
Nada Qaisar Qureshi, Syed Hamza Mufarrih, Seema Irfan, Rizwan Haroon Rashid, Akbar Jaleel Zubairi,Anum Sadruddin, Israr Ahmed, Shahryar Noordin
Abstract
Key words: Mobile phones; Contamination; Surgical site infections; Orthopedic surgeries;Antimicrobial resistance
INTRODUCTION
Each year, approximately $3.5 to $10 billion is spent on managing surgical site infections (SSIs) in the United States[1]. Data show that the incidence of SSIs is between 2% and 5%, with 60% of them being preventable[2]. Although the incidence can vary greatly as assessed using the National Nosocomial Infections Surveillance risk index[3],orthopedic surgery employs more robust sterile measures and has a lower rate of post-operative SSIs, particularly following elective surgery such as joint arthroplasty and hand surgery[4].
Nevertheless, given the consequent high morbidity, longer hospital stay,readmissions and revision procedures which increase health care costs, SSIs continue to be a cause for concern[5,6]. In 2012, according to the National Surgical Quality Improvement Program of the American College of Surgeons, SSIs were the most common cause of unplanned readmissions in 346 US hospitals[7]. It is estimated that by 2020 there will be at least 70000 total hip and knee arthroplasty revision surgeries due to deep SSIs, at a cost of US $1.62 billion annually[7].
Not surprisingly, these alarming numbers have led to countless efforts by health care professionals to identify and reduce the sources and risk factors of SSIs. Studies have identified numerous sources implicated in the transmission of pathogenic microbes including air[8], hospital surfaces[9], liquid nitrogen freezers[10], computer keyboards[11], stethoscopes[12], staff uniforms[13], tourniquets[14]and even leaving sterile trays open for too long[15].
A common source of contamination in the operating room seems to be the mobile phones used by health care professionals in all areas of the hospital[16,17]. Many studies have demonstrated the colonization of mobile or cell phones by potentially pathogenic organisms such asCoagulase-negative Staphylococcus(CoNS) species,Staphylococcus aureusand Acetinobacter[18-20]. Murgieret al[21]evaluated orthopedic operating rooms and added Corynebacterium and Viridans streptococci to the list.
While the transmission of infection through these contaminated mobile phonesviadirect and indirect routes is a possibility[18], the use of cell phones by health care professionals is a current and relevant reality, and further data are required to devise a protocol for their use in health care settings[18]. Surveys have revealed that not only are they considered an important work and academic tool by individual professionals[22], but cell phones have been shown to facilitate rapid communication between team members of the health care system[18,23]. Having an application in various clinical and educational scenarios including medical imaging[24], telemicroscopy[25], and improving patient-doctor communication[26,27], mobile phones have become indispensable.
Therefore, the aim of our study was to assess the extent of microbial colonization and drug resistance on the mobile phones of health care professionals in our hospital.Our goal was to estimate the proportion of health care workers including orthopedic and anesthesia attendings, residents, technicians and nursing staff working in the orthopedic operating room of our hospital with contaminated mobile phones. It is hoped that our findings will shed light on the need and cost-effectiveness of decontamination and/or restrictions on the use of mobile phones in operating rooms.
MATERIALS AND METHODS
We used the STROBE checklist for observational studies[28]to report the data.
Study design and setting
This was a cross-sectional study involving the collection of sample swabs from the mobile phones of hospital staff members and the administration of a structured questionnaire after obtaining informed written consent. Samples were collected in the orthopedic operating rooms and the adjacent recovery room of our university hospital over a period of two months between 0800 and 1700 h for 5-d a week excluding weekends.
Study participants
All orthopedic and anesthesia attendings, residents and technicians and all nursing staff working in the orthopedic operating room and/or the recovery room met the inclusion criteria. The only exclusion criteria were visiting staff members and medical students. The orthopedic attendings, residents and technicians were directly involved in the surgery and had physical contact with the patient. The anesthesia attendings,residents and technicians also had direct contact at the time of intubation and extubation. The nursing staff was in contact with the patient after surgery in the recovery room.
Data sources/measurement
A team of two researchers collected the data. One researcher obtained consent and administered the questionnaire while the other researcher collected the sample swabs.The questionnaire was structured to obtain brief demographic information and details of mobile phone and hand hygiene.
Informed written consent
All study participants provided informed written consent prior to study enrolment.Written consent was obtained after providing both a verbal explanation and written material regarding the study. Participants were ensured of their anonymity and Email addresses of the participants who wished to be informed of the results of the culture from the swab sample were recorded separately. Each participant was then asked to place his/her cell phone on a clean surface for collection of the swab while the questionnaire was administered.
Questionnaire administration
The participants were asked to fill out a structured questionnaire typed out in English.
Swab collection
The researchers followed a standardized protocol for sample collection developed through collaboration with the microbiology department of our university hospital.The researcher collecting the swab samples was dressed in surgical scrubs with a surgical cap and mask. After standard scrubbing, the researcher wore examination gloves to retrieve the mobile phone from the clean surface the owner placed it on. The swab was collected in accordance with recommendations from the Centers for Disease Control and Prevention[16]. First, an overlapping “S” pattern was used to cover the entire surface with horizontal strokes using a rolling motion to maximize contact with the surface. The same area was then swabbed again using vertical “S” strokes, and finally the swab was rotated once more using diagonal “S” strokes (Figure 1). Mobile covers were not removed for sample collection and any cracks on the screens were noted. Gloves were discarded after each use and the samples were labeled with a code and delivered to the microbiology lab for processing.
Study size
A total of 110 orthopedic and anesthesia attendings, residents and nursing staff working in the orthopedic operating room during the 2-mo study period were requested for a sample. With 10 refusals, 100 samples were obtained for inclusion in our study. Each mobile phone was examined only once.
Quantitative variables and statistical analysis
Data were analyzed using SPSS Version 22. A descriptive analysis was conducted on participant characteristics, the type of isolated organism and resistance to antibiotics.Continuous variables were reported as measures of central tendency and categorical variables as proportions. Based on the results of the Shapiro-Wilk normality test,appropriate measures of central tendency were reported (meanvsmedian). The Pearson chi-square test or Fisher's exact test was used to determine the relationship between cell phone contamination and variables such as age, gender, duration since last hand wash, duration since last cell phone cleaning, cracked screen, cell phone cover and cell phone with keypad.
Further analysis was conducted on the most common species isolated to identify the risk factors for contamination. This was done by fitting a binary logistic regression model. The variables were divided into 2 groups; Specialty-related factors such as(orthopedic surgeon, anesthesia attending, nursing staff, resident and technicians) and cell phone-related factors (such as type of cell phone, cracked screen, cell phone cover,duration since last cleaning of the cell phone and duration since last hand-wash).Results were reported as crude and adjusted Odds ratio. The threshold for statistical significance was set atP< 0.25 for univariate analysis andP< 0.05 for multivariable analyses.
RESULTS
Questionnaire
During the course of 2 mo, 110 individuals were approached. With 10 refusals to consent, 100 individuals participated in our study. The median age was 30 years with 81 male participants. A total of 43 orthopedic team members, 42 anesthesia team members and 15 members of the nursing staff were included. Only 10 out of the 100 participants had basic phones, with the remainder having smart phones. Sixty-seven participants had mobile covers and 42 had one or more cracks on their screen. 55 participants reported cleaning their cell phone with an alcohol swab with the median time passed since cleaning their cell phone at the time of sample collection being 24 h.Ten participants chose not to answer this question.
Culture and sensitivity
Results of the culture showed that 93 of the 100 tested cell phones were colonized by one or more bacterial species. The most common species isolated was the CoNS,found on 62% of the cell phones (Figure 2: Organisms isolated from mobile phones).This was followed by Micrococcus species (41%) and Bacillus (26%) species with the majority having low colony counts (Table 1). Twenty-one of 22 mobile phones (95.5%)belonging to attendings were colonized with potentially pathogenic bacteria.Interestingly, there was 100% and 80% resistance to meropenem among the Enterobacter and Pseudomonas species, respectively, and 54% resistance to oxacillin among CoNS species (Table 2). One phone harbored up to 6 organisms, 44 phones harbored more than 1 organism and 49 phones harbored exactly 1 organism (Figure 3).
Factors influencing bacterial colonization
To understand which factors contribute to an increased risk of colonization by the bacteria identified in the culture, variables recorded from the questionnaire were analyzed with respect to the presence or absence of colonization. Mobile covers and cracked screens were found to be associated with microbial contamination, while cleaning the cell phone, particularly within the last 24 h, were associated with having less or no contamination (Table 3).
Figure 1 Sampling technique for swab collection - The blue rectangle represents the mobile front and back.“S” shaped strokes were made vertically, horizontally and diagonally to obtain the sample.
Factors influencing colonization by CoNS
An important cause of post-operative SSIs in orthopedic surgery, CoNS was isolated on 62% of the mobile phones. To understand this further, we analyzed demographic/job-related and cell phone-related factors to assess their association with microbial contamination (Table 4). The results of univariate analysis showed that the risk of colonization with CoNS was significantly higher in orthopedic surgeons (P= 0.067), technicians (P= 0.185) and anesthesia (P= 0.009) technicians. The presence of a mobile cover (P= 0.001) and more than 24 h since cleaning the cell phone (P= 0.013)were also significant risk factors in univariate analysis. However, multivariable analysis showed that the category of anesthesia technicians (P= 0.043) and the presence of a mobile cover (P= 0.004) were the only significant risk factors for colonization by CoNS.
DISCUSSION
Despite persistent efforts to minimize the rate of post-operative SSIs, their incidence following orthopedic surgery unfortunately continues to persist[29]. Along with introducing different regimens of antibiotic prophylaxis, optimization of patients'comorbid conditions and improving operating room sterile practices[30], numerous attempts have been made to identify potential sources of SSIs in the operating room.Among the many suspects is the mobile phone, which nowadays is akin to an electronic appendage of its owner. Considering the importance of mobile phones as an academic and communicative tool[31-33], significant contamination of cell phones with drug resistant bacteria may call for restriction of their use inside the operating room and the patient's bedside.
The results of our study showed that 93 of 100 samples taken from the mobile phones of health care professionals in the orthopedic operating room were contaminated with potentially pathogenic organisms. Interestingly and of concern,the most common organism causing SSIs following orthopedic surgery[34-38], CoNS was also the most common organism isolated in our study.
The results of similar studies published during the last 2 years show a wide range of colonization between 9%-90%, with a wide variety of organisms including CoNS,Staphylococcus aureus, Acinetobacter species[16,18,39-41]. As these studies are from all around the world, this variation may be the result of differences in geographical and economic status between countries. A meta-analysis published in 2016 showed that the contamination of cell phones of health care professionals was significantly greater in developing countries in comparison to the developed world[42].
In this study, we only investigated the extent of microbial colonization of mobile phones in the orthopedic operating room. Specific investigation into whether this contamination leads to SSIs was not performed in our study. Some researchers have attempted to investigate the relationship between mobile phone contamination and SSIs. Changet al[20]in 2017 used genotyping to demonstrate the transmission of pathogenic organisms between the hands, nostrils and mobile phones of health care professionals. However, typing of strains responsible for SSIs was not carried out.Another study compared the strains found on the mobile phones and skin of health care professionals with the strains isolated from the skin and blood samples of their patients. A match was found with the strains on the skin of the patients but not with the blood isolates[43].

Table 1 Results of bacterial culture and colony counts
Theoretically, contaminated cell phones can lead to SSIs in various ways. While direct transmission (contact between the reservoir and the host) is unlikely in this situation, indirect transmissionviathe hands of medical personnel and crosscontamination of other medical equipment is plausible and is a cause for concern[18].An incident in Larry Dossey's “Distracted doctoring and the iPatient” narrates a nurse attending a phone call after washing her hands and forgets to clean them again before administering intravenous antibiotics to her patient[44], serving as an example of how cell phones may unintentionally contribute to a breach of the hand hygiene protocol.A survey conducted at a hospital in Barbados reported 47% of health care professionals using their mobile phones while attending patients with only 3%actually washing their hands after use[45]. Another study proved the ineffectiveness of the practice of using a sterile disposable towel as a barrier for attending phone calls while scrubbed in[2].
Antibiotic resistance among isolated organisms may also be a problem. Our study shows significant resistance to meropenem among Enterobacter and Pseudomonas species. More importantly, 54% of the isolated CoNS species were resistant to oxacillin/methicillin. Studies show that these methicillin resistant strains may act as reservoirs for the genetic material, particularly SCCmec Iva, found in MRSA[46].
In 2010, Royet al[47]suggested that the concept of implementing highly expensive methods to eradicate bacterial contamination in the hope of reducing the cost of treating SSIs has yet to be proven. They went on to refer to attempts made at erasing contamination that is not documented to cause SSIs as a “trap” of treating only surrogate end-points[47]. While proof of contaminated cell phones causing SSIs may not be concrete, unsafe practices involving contaminated mobile phones and the prevalence of high rates of antibiotic resistance among the isolated organisms also do not make it easy to simply discard the idea of dealing with contaminated cell phones.The balance ultimately lies in using only cheap and convenient methods to reduce contamination until a causal relationship is established.
In light of research findings we evaluated several factors including demographic variables, cell phone characteristics and cleaning practices as they relate to the contamination of mobile phones. Similar to previous studies, our results also showed that demographic variables and hand washing practices do not have any significant impact on the risk of contamination[19,48]. However, cleaning the mobile phone with an alcohol swab did decrease the risk of contamination. This may be due to the ubiquitous use of mobile phones by individuals where the phone is acting as a reservoir. Although our study shows no significant difference in contamination between basic phones and smart phones, previous studies have shown contradicting views on this[48-50].
Our study adds to existing literature by showing a significantly increased risk of contamination on phones with a mobile cover and a cracked screen. Additionally,participants who claimed to have cleaned their cell phone with an alcohol swab in the last 24 h also had significantly less contaminated cell phones. These findings could form the basis of the concept of “mobile hygiene” involving steps as simple as theperiodic change of a mobile cover, replacement of a cracked screen or even wiping your phone with an alcohol swab in the morning. With further investigation into factors contributing to the contamination of mobile phones and replication of the findings of our study, the practice of mobile hygiene could yield the perfect costeffective balance that contaminated cell phones deserve until they are established as a direct cause of SSIs. Caveats in our study include potential attribution bias as the samples continued to be collected over two months rather than in a cross-sectional manner. Furthermore, to contain the costs of sampling, we used examination gloves instead of sterile gloves to collect the culture specimens. Our study investigated only the extent of colonization by potentially pathogenic bacteria on mobile phones in the orthopedic operating room. We did not investigate the link between colonization and SSIs. Further research needs to be conducted to investigate the causation between colonization of mobile phones and SSIs. In addition, when studying the factors contributing to the risk of colonization it is necessary to identify of any source of infection in the owner of the mobile phone.

Table 2 Antibiotic resistance analysis
In conclusion, SSIs following orthopedic surgery are a cause of concern due to their associated morbidity, potential for mortality and phenomenal cost; thus, there is a need to identify and eradicate any sources of pathogenic organisms. Health care workers' mobile phones are frequently contaminated with pathogenic bacteria.Studies examining the relationship between contaminated cell phones and SSIs need to be conducted. Until such a causation is established, cheap and convenient methods are needed to decrease contamination in the form of simple practices constituting“mobile hygiene”.

Table 3 Factors affecting bacterial colonization of cell phones

Table 4 Demographic/job related and cell phone related factors for Coagulase-negative Staphylococcus species
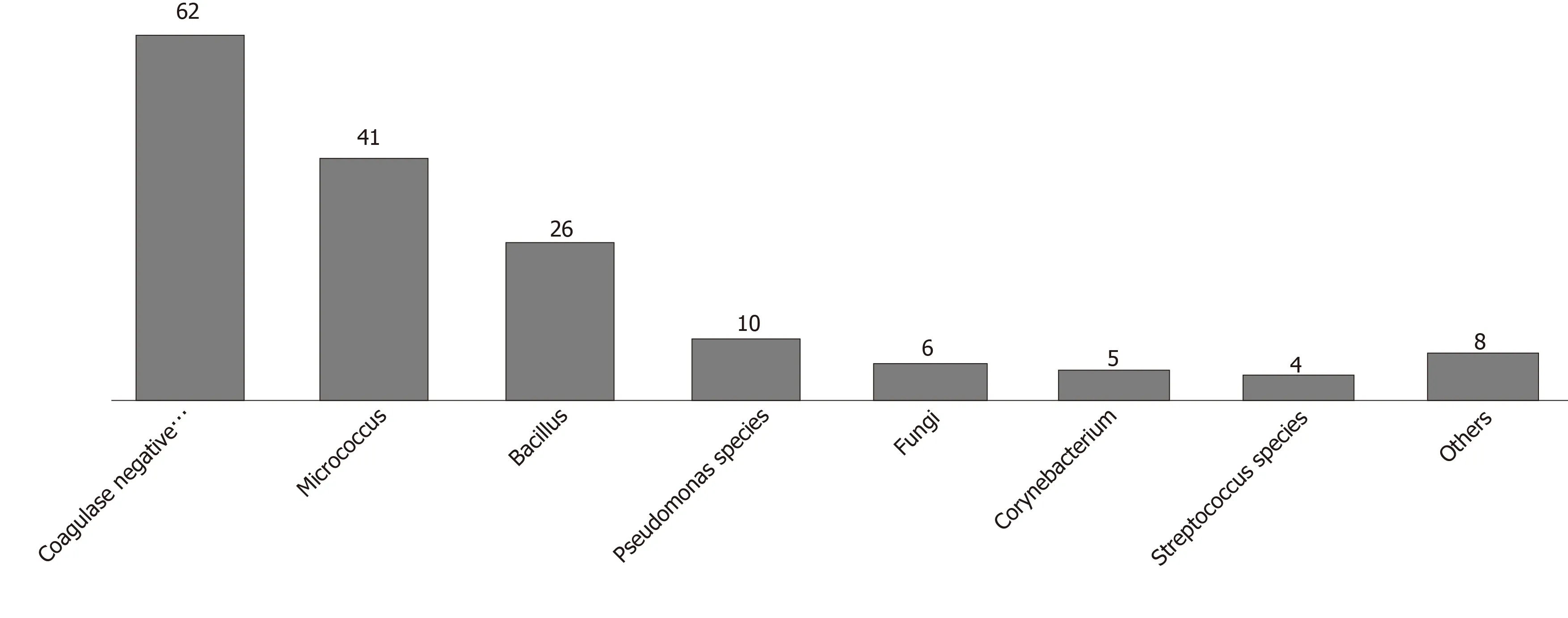
Figure 2 Most common organisms isolated from mobile phones. Number represents the number of mobile phones with the organism. 44% of mobile phones harbored more than 1 organism.

Figure 3 Number of unique species of microorganisms on mobile phones.
ARTICLE HIGHLIGHTS
Research background
Surgical site infections (SSIs) are a major cause of morbidity and mortality following orthopedic surgery. Each year, approximately $3.5 to $10 billion is spent on managing SSIs in the United States. Data show that the incidence of SSIs is between 2% to 5%, with 60% of them being preventable. To decrease the rate of SSIs following orthopedic surgery, potential sources of contamination need to be identified.
Research motivation
Literature has identified numerous sources implicated in the transmission of pathogenic microbes including air, hospital surfaces, liquid nitrogen freezers, computer keyboards,stethoscopes, staff uniforms, tourniquets and even leaving sterile trays open for too long. Mobile phones are used ubiquitously and have academic and clinical uses. Recently, mobile phones have been implicated as a source of contamination in the orthopedic operating rooms.
Research objectives
The purpose of this study was to investigate microbial colonization, risk factors and antibiotic sensitivity patterns on the mobile phones of health care professionals in the orthopedic operating room.
Research methods
We conducted a cross-sectional study involving culture and sensitivity analysis of swabs taken from mobile phones of orthopedic and anesthesia attendings, residents, technicians and nurses working in the orthopedic operating rooms over a period of 2 mo. Demographic and cell phone related factors were recorded using a questionnaire and the factors associated with contamination were analyzed.
Research results
Ninety-three of 100 mobile phones were contaminated. Species isolated were Coagulase negative Staphylococcus (62%), Micrococcus (41%) and Bacillus (26%). The risk of contamination was increased by mobile covers and cracked screens and decreased by cell phone cleaning.
Research conclusions
Mobile phones belonging to health care workers are frequently contaminated with pathogenic bacteria with the potential of transferring drug resistance to nosocomial pathogens.
Research perspectives
Studies investigating the relationship between mobile phones and SSIs need to be conducted.The concept of “mobile hygiene” involving the change of mobile covers, replacement of cracked screens or even wiping the phone with an alcohol swab could yield the cost-effective balance that contaminated cell phones deserve until they are established as a direct cause of SSIs.
 World Journal of Orthopedics2020年5期
World Journal of Orthopedics2020年5期
- World Journal of Orthopedics的其它文章
- lmpact of gender and race on expectations and outcomes in total knee arthroplasty
