常规留置导尿失败后处理急性尿潴留临床方法的对比分析
胡海义 李恭会 吴海洋
[摘要] 目的 探討常规留置导尿失败后处理急性尿潴留留置导尿的不同方法,以期提高患者一次性留置导尿成功率,尽早解除尿路梗阻并减少尿道损伤。 方法 分析2014年1月~2019年9月我院208例急性尿潴留患者的临床资料,根据治疗方式不同,将患者分为尿道扩张后留置导尿组(尿扩组)和内镜下导丝引导留置组(内镜组),分析两组留置导尿成功率及并发症的差异。 结果 尿扩组中所有女性患者、无尿道手术史患者及尿道外口狭窄患者经尿道扩张扩后均能成功留置导尿;内镜组中TUR及TURP患者均可成功留置导尿管。TUR及SP患者两组留置尿管成功率无显著性差异(P>0.05)。TURP(P<0.001)及RP(P=0.008)患者内镜组留置尿管成功率均显著高于尿扩组。内镜组留置尿管总成功率明显高于尿扩组(95.7% vs 80.9%,P=0.001);内镜组术中VAS疼痛评分(2.2±0.3 vs 5.7±0.9,P<0.001)及术中明显肉眼血尿发生率(5.4% vs 23.5%,P<0.001)均显著低于尿扩组;术后3个月拔除尿管后,内镜组尿潴留发生率明显低于尿扩组(15.1% vs 28.7%,P=0.02)。 结论 女性及无尿道手术史的男性患者大多可经尿道扩张后即可成功留置导尿;而对于合并尿道手术史,尤其合并前列腺手术史的男性患者,内镜下留置导尿管优于单纯尿道扩张。
[关键词] 急性尿潴留;常规留置导尿;困难性留置导尿;尿道扩张;膀胱造瘘术
[中图分类号] R472 [文献标识码] B [文章编号] 1673-9701(2020)10-0091-05
[Abstract] Objective To investigate different methods for treating indwelling catheterization for acute urinary retention after failure of routine indwelling catheterization, so as to improve the success rate of one-time indwelling catheterization for patients, relieve urinary obstruction as soon as possible, and reduce urethral injury. Methods The clinical data of 208 patients with acute urinary retention in our hospital from January 2014 to September 2019 were analyzed. According to different therapeutic regimens, patients were divided into the group performed with indwelling catheterization after urethral dilatation(urethral dilatation group) and the endoscopic guidewire-guided indwelling group(endoscopic group). The differences in success rate and complications of indwelling catheterization between the two groups were analyzed. Results All the female patients, the patients without history of urethra operation and the patients with stricture of external orifice in the group of urinary dilatation were able to indwelling catheterization successfully. In the endoscopic group, TUR and TURP patients could be placed catheter successfully. There was no significant difference in the success rate of indwelling catheter in TUR and SP patients between the two groups(P>0.05). The success rate of indwelling catheter in TURP(P<0.001) and RP(P=0.008) patients in the endoscopic group was significantly higher than that in urethral dilatation group. The overall success rate of indwelling catheterization in the endoscopic group was significantly higher than that in the urethral dilatation group(95.7% vs 80.9%, P=0.001). The intraoperative VAS pain score(2.2±0.3 vs 5.7±0.9, P<0.001) and the intraoperative incidence of obvious macroscopic hematuria(5.4% vs 23.5%, P<0.001) in the endoscopic group were significantly lower than those in the urethral dilatation group. After catheter removal 3 months after surgery, the incidence of urinary retention in the endoscopic group was significantly lower than that in the urethral dilatation group(15.1% vs 28.7%, P=0.02). Conclusion Female patients and male patients with no history of urethral surgery can be successfully performed with indwelling catheterization after urethral dilatation. While for male patients with combined urethral surgery history, especially combined with prostate surgery history, endoscopic indwelling catheterization is better than simple urethral dilatation.
[Key words] Acute urinary retention; Routine indwelling catheterization; Difficult indwelling catheterization; Urethral dilatation; Cystostomy
急性尿潴留是泌尿系统常见的急症之一,占泌尿系统疾病急诊患者的53%,留置导尿或耻骨上膀胱造瘘是解除急性尿潴留患者的标准治疗。留置导尿是最为直接有效的治疗手段,常规留置导尿大多可顺利解除下尿路梗阻,但是对于一些特殊患者,比如前列腺增生的老年男性或是合并尿道手术史的患者,对于急诊医师或是社区全科医师来说,常规留置导尿往往难以顺利置管,需请泌尿外科专科医师会诊或借助其他技术手段解决。基于尿道的解剖特点,临床实践中初始常规采用16 F双腔导尿,如留置困难,为方便讨论本文视为常规留置导尿失败或困难性留置导尿。本文选取浙江大学医学院附属邵逸夫医院自2014年1月~2019年9月急诊会诊或病区住院急性尿潴留在首次常规留置导尿失败后的208例患者,分析其留置导尿的临床治疗情况,现报道如下。
1 资料与方法
1.1 一般资料
本次研究纳入自2014年1月~2019年9月经我科处理急性尿潴留首次常规留置导尿失败的患者共208例,其中男192例,女16例,年龄22~88岁,平均(72.5±5.7)岁,其中尿扩组115例(男99例,女16例),平均(70.3±6.3)岁;内镜组93例(男93例,女0例),平均(75.4±2.8)岁。两组平均年龄比较,差异无统计学意义(P>0.05),具有可比性。
尿扩组中,女16例、无尿道手术史41例、尿道口狭窄7例、12例合并内镜下肿瘤切除或碎石手术(Transurethral resection or lithotripsy,TUR)如:輸尿管镜碎石、经尿道膀胱肿瘤电切等;25例合并经尿道前列腺切除术(Transurethral resection of prostate,TURP);3例合并耻骨上前列腺摘除史(Suprapubic prostatectomy,SP);11例合并前列腺癌根治性切除术(Radical prostatectomy,RP)。内镜组中,8例曾行内镜下肿瘤切除或碎石术(TUR);43例既往行经尿道前列腺电切术(TURP);9例合并耻骨上前列腺摘除术(SP);23例合并前列腺癌根治性切除史(RP);10例曾行尿道会师成形术(Interlocking urethroplasty,IU)。
1.2 方法
术前常规了解患者病史,询问记录排尿情况、手术史、外伤史,严格遵循目前临床通用的导尿标准操作规范,初始采用16 F双腔导尿施行置管,如首次置入导尿管困难,则视为常规留置导尿管失败或困难性留置导尿。根据最终导尿情况分为尿扩组和内镜组。尿扩组即在常规导尿失败后,采用适当型号金属尿道扩张器逐号探明腔道,适度扩张尿道后留置导尿管。内镜组即在常规留置导尿失败后,尿道扩张困难腔道不确切改行膀胱镜或输尿管镜探查,留置安全导丝后在其引导下置入导尿管,从而留置导尿。经上述两种方法均留置导尿管失败的患者采用耻骨上膀胱穿刺造瘘术解除患者急性尿潴留症状。
1.3 观察指标
观察并记录两组患者不同方法导尿成功率及并发症情况,如:术中疼痛评分、明显肉眼血尿及导尿术后3月尿潴留发生率指标。术中疼痛采用视觉模拟评分(Visusal analogue scale,VAS)疼痛评分量表进行评估,用于患者术中留置导尿管疼痛程度的评估。基本的方法是用一条标有标准刻度的长为10 cm的一次性标尺,两端分别为“0”分端和“10”分端,0分表示无痛,10分代表难以忍受的最为剧烈的疼痛。患者标记后予以记录。所有患者均于术后2 h内用透明容器收集第一次排尿的尿液,记录肉眼血尿情况及导尿术后3个月后随访排尿情况,记录再次发生尿潴留的发生情况。
1.4 统计学方法
采用SPSS19.0统计学软件进行数据分析。计量资料符合正态分布,用均数±标准差(x±s)表示,采用t检验,计数资料以[n(%)]表示,采用χ2检验,P<0.05为差异有统计学意义。
2 结果
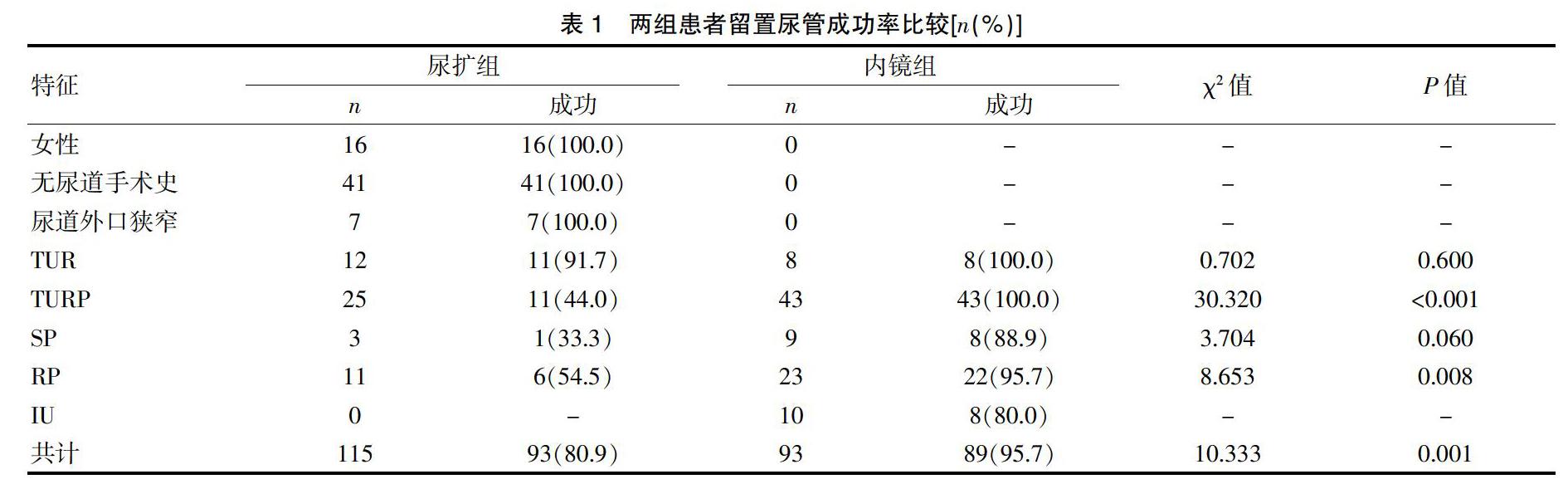
2.1 两组患者留置尿管成功率比较
尿扩组中所有女性患者、无尿道手术史患者及尿道外口狭窄患者经尿道扩张扩后均能成功留置导尿;内镜组中TUR及TURP患者均可成功留置导尿管。TUR及SP患者两组留置尿管成功率无显著性差异(P>0.05)。TURP(P<0.001)及RP(P=0.008)患者内镜组留置尿管成功率均显著高于尿扩组。内镜组共留置尿管成功89例,成功率为95.7%,而尿扩组留置尿管成功93例,成功率为80.9%,内镜组留置尿管总成功率明显高于尿扩组(P=0.001)。见表1。
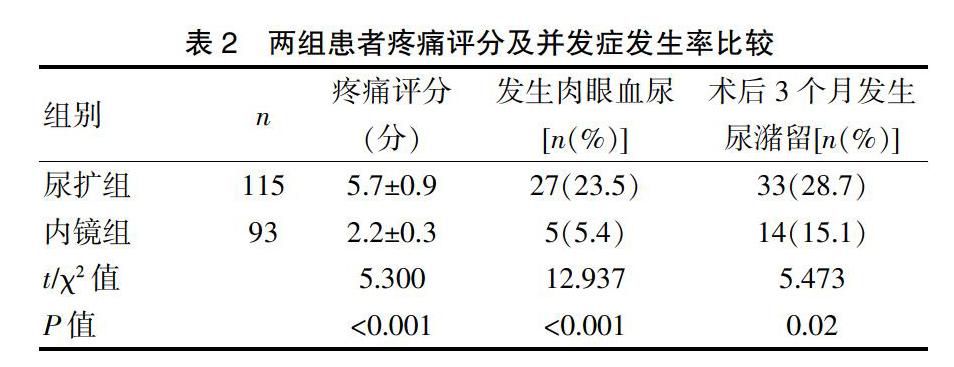
2.2 两组患者疼痛评分及并发症发生率比较
尿扩组疼痛评分(VAS)为(5.7±0.9)分,内镜组疼痛评分(VAS)为(2.2±0.3)分,两组之间有显著性差异(P<0.001);尿扩组共有27例患者术中出现明显肉眼血尿,内镜组共有5例患者术中出现明显肉眼血尿,后者肉眼血尿发生率显著低于前者(5.4% vs 23.5%,P<0.001)。术后3个月拔除尿管后,尿扩组及内镜组分别有33例及14例患者出现尿潴留,内镜组尿潴留发生率明显低于尿扩组(15.1% vs 28.7%,P=0.02)。见表2。
3 讨论
急性尿潴留是泌尿外科及急诊科较为常见的疾病,高龄男性前列腺增生继发尿潴留最为常见,同时随着泌尿外科经尿道腔内手术以及尿道重建手术的开展,尤其前列腺的腔内治疗继发尿道狭窄或是膀胱颈口挛缩的发生率也有所增加[1,2]。患者常因急性尿潴留急诊来院,不同的患者导致尿潴留的原因也不尽相同,常见致病因素可以单独或合并以下情况:①膀胱出口梗阻;②逼尿肌功能障碍;③膀胱过度充盈[3]。探讨首次常规留置导尿失败后留置导尿的操作策略,以期提高一次性留置导尿的成功率,避免不必要操作,尽早解除患者下尿路梗阻是本文讨论重点。
导尿术作为改善急性尿潴留的一种有效治疗手段已存在相当长的历史,同时也是一名医师必须掌握的基本操作。目前导尿管种类较多,有单腔、双腔及三腔导尿,多种涂层导尿管甚至末端弯曲的导尿管也日益应用广泛。导尿管的直径决定了其型号大小,通常以French(简称Fr)为单位,1 Fr=0.33 mm。成年男性尿道直径大约30 Fr,基于男性与女性尿道的不同解剖,16 Fr型号大小的导尿管适合于绝大多数人,是留置导尿的初始选择[4,5]。临床上常规留置导尿困难者多为老年男性患者,其皆因前列腺增生所致后尿道延长,或者既往合并尿道相关手术史或盆腔放疗史,比如:尿道会师术、前列腺摘除或前列腺癌根治性切除术等,患者存在尿道狭窄、膀胱颈口后唇抬高挛缩硬化或尿道内腔欠光滑所致[6,7]。对于后尿道延长患者必要时需借助金属导丝引导。而既往有尿道手术史患者可合并尿道狭窄,可追踪既往排尿情况,如仍有尿线变细,可尿道扩张器探查尿道,探明尿道内腔多可留置;如平素排尿难以成线,提示尿道狭窄严重,而盲目扩张器械挤压组织可致内腔消失,增加难度,此时不妨考虑膀胱镜或输尿管镜导丝引导下探明腔道再行尿道扩张,早在1994年Beaghler M等[8]利用膀胱软镜顺利完成留置导尿,避免了膀胱造瘘。否认尿路手术史患者多可在充分润滑下,纠正耻骨前弯,选取合适型号的导尿管,顺利置入。不适当的反复置管可造成尿道黏膜损伤甚至假道形成,很大程度上延长了患者住院时间,增加了后期处理的复杂性[5]。女性尿道短而直,常规置管简单易行,因而一些复杂性留置导尿难度容易忽视,尤其对于部分老年女性,体型肥胖或因雌激素水平撤退,或者宫颈癌放疗术后,阴道组织萎缩而同时向阴道内牵拉尿道口,致尿道口暴露不清,留置导尿也较为棘手,此时可以食指探入阴道,可避免导尿管滑入阴道,同时可在手指导引下置管或者利用妇科窥阴器暴露阴道及尿道口,以便置管[9]。值得一提的是,留置導尿过程中,尤其是女性患者,应注意安慰缓解紧张情绪,避免其过分紧张,嘱患者深呼吸、放松有助于改善膀胱痉挛从而顺利置管。Patel AR等[10]在一项系统性多元分析中证实留置导尿过程中,以2%利多卡因麻醉尿道黏膜与安慰剂组对照并无明显差异,然而患者对麻醉剂的安慰作用还是相当依赖。诸多留置导尿技巧相继报道,Harkin DW等[11]在1998年报道了30例外伤后复杂性导尿患者,通过注射器抽吸60 mL生理盐水连接导尿管,导尿管遇到阻力后,迅速注水,扩张尿道腔,同时快速插入导尿管,利用该方法30例患者均置管成功,同时避免应用导丝、扩张器、内镜等器械。越来越多的国内外学者也根据自身的实践经验报道了一些新技巧[11-15],也有学者利用超声影像监视下导丝引导留置导尿,但尚不广泛[16],目前多数研究建议对于初始导尿困难的患者,利用导丝引导下留置导尿管,更加确切安全[3,16]。Bugeja S等[15]根据相应的原理结合镍钛锘导丝与16 F导尿管开发了一款导尿装置(Urethral catheterisation device,UCD),提高了一次性成功置管几率同时减少了尿道损伤。Yuminaga Y等[17]通过一项多中心前瞻性的研究认为,运用亲水导丝引导下留置导尿管(即Seldinger 技术)对于非泌尿专业医务人员处理常规留置导尿管困难的患者与泌尿专业人员相比同样安全有效。
留置导尿是一项侵入性操作,伴随着感染的风险,反复盲目置管受阻,容易导致尿道损伤甚至假道形成,延长留置时间,继发尿路感染[18,19]。Sliwinski A等[20]对急诊尿潴留困难留置导尿管进行了综述,认为留置导尿前充分了解患者既往排尿情况及尿路手术史,掌握困难性留置导尿的技巧,有助于采取合适的措施以便提高留置导尿成功机率,减少患者痛苦。然而对于尿道梗阻严重的患者,单纯性尿道扩张或是内镜探查有可能加重尿道梗阻,在此情况下膀胱造瘘仍然是临床明智的选择[6]。本次研究提示,所有女性患者、尿道无手术操作史患者、尿道外口狭窄患者尿扩后均能成功留置导尿。对于尿道手术操作史常规留置导尿失败患者,尿扩后留置导尿成功率明显低于采用内镜下探查,留置安全导丝后在其引导下留置导尿成功率,二者在统计学上有显著差异。
综上所述,对于常规留置导尿失败后急性尿潴留的临床处理,尤其要留意患者是否合并下尿路尤其是前列腺手术史,避免盲目暴力插管。对于男性尿道手术史患者,在常规导尿失败后,借助内镜探查与导丝引导,和单纯通过尿道扩张后置管相比,一次性置管成功率明显提高,有助于尽早解除患者下尿路梗阻。值得注意的是,本研究例数较少,缺乏更为严密的前瞻性设计对照,同时难以涵盖临床所有尿潴留情况,对于病情复杂的尿潴留患者,膀胱造瘘术仍然是一项相对安全有效的治疗手段。
[参考文献]
[1] Tao H,Jiang YY,Jun Q,et al. Analysis of risk factors leading to postoperative urethral stricture and bladder neck contracture following transurethral resection of prostate[J]. International Braz J Urol:Official Journal of the Brazilian Society of Urology,2016,42(2):302-311.
[2] Granieri MA,Wang HS,Routh JC,et al. A nationwide assessment of the emergency department management of acute urinary retention due to urethral stricture[J]. Urology,2017,100(3):79-83.
[3] Yoon PD,Chalasani V,Woo HH. Systematic review and meta-analysis on management of acute urinary retention[J].Prostate Cancer and Prostatic Diseases,2015,18(4):297-302.
[4] Thomsen TW,Setnik GS. Videos in clinical medicine. Male urethral catheterization[J]. The New England Journal of Medicine,2006,354(21):e22.
[5] Daneshgari F,Krugman M,Bahn A,et al. Evidence-based multidisciplinary practice:Improving the safety and standards of male bladder catheterization[J]. Medsurg Nursing:Official Journal of the Academy of Medical-Surgical Nurses,2002,11(5):236-241,246.
[6] Rocco NR,Zuckerman JM. An update on best practice in the diagnosis and management of post-prostatectomy anastomotic strictures[J]. Therapeutic Advances in Urology,2017,9(5):99-110.
[7] Song J,Eswara J,Brandes SB. Postprostatectomy anastomosis stenosis:A systematic review[J]. Urology,2015,86(2):211-218.
[8] Beaghler M,Grasso M,Loisides P. Inability to pass a urethral catheter:The bedside role of the flexible cystoscope[J]. Urology;1994,44(2):268-270.
[9] Rouzi AA. Urinary catheterization and female genital mutilation[J]. CMAJ:Canadian Medical Association Journal=Journal De l'Association Medicale Canadienne,2013, 185(3):235.
[10] Patel AR,Jones JS,Babineau D. Lidocaine 2% gel versus plain lubricating gel for pain reduction during flexible cystoscopy:A meta-analysis of prospective,randomized,controlled trials[J]. The Journal of Urology,2008, 179(3):986-990.
[11] Harkin DW,Hawe M,Pyper P. A novel technique for difficult male urethral catheterization[J]. British Journal of Urology,1998,82(5):752-753.
[12] 翦曉明,夏仁惠,李志民,等. 吸痰管结合导丝用于男性尿道狭窄留置导尿的效果观察[J]. 中国中西医结合外科杂志,2013,19(4):442-443.
[13] 相俊,罗华荣,廖国强. 留置导尿新方法在男性尿潴留患者中的应用[J]. 临床医学工程,2012,19(7):1102-1103.
[14] Alnadhari I,Abdeljaleel O,Ali O,et al. Urethral catheterization of buried penis in obese patients:A novel technique and literature review[J]. Obesity Surgery,2018,28(10):3348-3351.
[15] Bugeja S,Mistry K,Yim IHW,et al. A new urethral catheterisation device(UCD) to manage difficult urethral catheterisation[J]. World Journal of Urology,2019,37(4):595-600.
[16] Tadtayev S,Gresty H,Manson-Bahr D. Difficult urethral catheterisation made safer:Visualising the 'blind' hydrophilic wire[J]. Annals of the Royal College of Surgeons of England,2016,98(8):594.
[17] Yuminaga Y,Kam J,Louie-Johnsun M. Multi-centre,prospective evaluation of the Seldinger technique for difficult male urethral catheter insertions by non-urology trained doctors[J]. BJUinternational,2017,120(Suppl 3):21-27.
[18] Advani SD,Fakih MG. The evolution of catheter-associated urinary tract infection (CAUTI):Is it time for more inclusive metrics?[J]. Infection Control and Hospital Epidemiology,2019:1-5.
[19] Shuman EK,Chenoweth CE. Urinary catheter-associated infections[J]. Infectious Disease Clinics of North America,2018,32(4):885-897.
[20] Sliwinski A,D'Arcy FT,Sultana R,et al. Acute urinary retention and the difficult catheterization:Current emergency management[J]. European Journal of Emergency Medicine:Official Journal of the European Society for Emergency Medicine,2016,23(2):80-88.
(收稿日期:2019-12-12)