Surgical intervention for malignant bowel obstruction caused by gastrointestinal malignancies
Peng-Ju Chen, Lin Wang, Yi-Fan Peng, Nan Chen, Ai-Wen Wu
Peng-Ju Chen, Lin Wang, Yi-Fan Peng, Nan Chen, Ai-Wen Wu, Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education), Department of Gastrointestinal Cancer Center, Unit III, Peking University Cancer Hospital and Institute, Beijing 100142, China
Abstract
Key words: Gastrointestinal neoplasms; Malignant bowel obstruction; Metastasis;Palliative surgery; Prognosis; Quality of life
INTRODUCTION
Malignant bowel obstruction (MBO) is a frequent event for patients with end-stage cancer, especially in gastrointestinal (GI) and ovarian cancer[1-3]. It had been reported that 10%-50% of patients with cancer will develop MBO during the preterminal stage[4]. Patients with MBO suffered from an inability to eat, abdominal pain,distention, nausea, and vomiting, resulting in a poor quality of life (QOL), stress, and emotional problems.
The clinical management of MBO requires a specific and individualized approach based on the expected rest time of the disease, objectives of care, and the patient's preferences. The primary treatment objective in patients with MBO is to relieve symptoms, restore food intake, and improve nutrition[5]. The most common treatment options for patients with MBO included nasogastric drainage, total parenteral nutrition, pain control, somatostatin, endoscopically placed stents, and palliative surgery[4]. Due to the heterogeneity of MBO patients, there is no consensus on the optimal treatment strategy for improving QOL and prolonging survival. The decision making of the management of MBO should be individualized[6].
Surgical intervention is usually considered to be the last treatment option that may relieve the symptoms of MBO. However, the decision to proceed with palliative surgery is usually difficult, especially for patients who may only have a few weeks to live. Additionally, MBO patients suffering from malnutrition are not good candidates for surgical intervention because of the high postoperative mortality and morbidity rates. Previous studies included several types of malignancies in their analysis, and most focused on the treatment of ovarian cancer. At present, there is limited evidence on the effectiveness of surgical intervention for MBO[7].
The surgical treatments for MBO include percutaneous venting gastrostomy, stoma diversion and cytoreductive surgery,etc.[8-10]. However, some patients with extensive peritoneal metastasis may have multiple obstruction sites, and an ostomy or by-pass surgery may not be feasible. Previous studies have shown that some selected patients with recurrent, unresectable colorectal cancer may benefit from cytoreductive surgery,massive tumor debulking surgery and hyperthermic intraperitoneal chemotherapy[11-14].
We performed a retrospective study at a single institution to determine the effects of palliative surgery for MBO in patients with GI cancers and analyzed symptom palliation rates, postoperative mortality, complications after surgery, and survival rates.
MATERIALS AND METHODS
Patient selection
Between January 2016 to October 2018, we enrolled 61 patients with MBO caused by peritoneal metastasis of gastric and colorectal cancer underwent surgical treatment at the Peking University Cancer Hospital.
3.2.2 子女情况 有子女的护士器官捐献态度问卷得分高于没有子女的护士,差异具有显著性(P<0.05)。有无子女是否影响护士对器官捐献的态度,目前尚未查阅到其他类似研究。本研究中95.50%的参与者是女性,可能女性做母亲后会更具爱心及奉献精神。
Including criteria for patients are: (1) Clinical evidence of bowel obstruction; (2)Obstruction distal to the Treitz ligament; (3) The presence of primary gastric and colorectal cancer; (4) The absence of curable possibilities; (5) Ineffective conservative treatment for obstruction; (6) Expected survival of more than 2 mo; and (7) Patients and their families willing to undergo surgery[4].
All patients discussed their options with the Multiple Disciplinary Team before the operation, and a treatment plan was developed based on the patients' preferences.The surgical options included ostomy/by-pass surgery (OBS) and massive debulking surgery (MDS).
Indications for OBS:(1) Localized or single-site tumor obstruction; (2) Patients may benefit from further chemotherapy; and (3) Patients and their families do not receive aggressive tumor reductive surgery.
Indications for MDS:(1) Perioperative risk evaluation indicates that patients can tolerate surgery; (2) After imaging and physical examination, it is expected that the obstruction and symptoms can be effectively relieved after operation; (3) Patients can endure at least 2 months of oral feeding and non-obstructive survival; (4) It is expected that at least 2 meters of small intestine will remain after the operation; and(5) Patients and their families had a strong preference for surgery.
Evaluation of surgical effectiveness:(1) Solid food intake and symptom relief rates 60 d after surgery[15]; (2) Postoperative complications and mortality rates within 30 d;and (3) Postoperative survival time.
Statistical analysis
Statistical analysis was performed by using the IBM-SPSS19 software package. The categorical variables were compared by the Pearson’s chi-square test. Overall survival rates were analyzed by the Kaplan-Meier method and the difference between the groups were evaluated by a log-rank test.P< 0.05 was considered as statistically significant. Significant prognostic factors were analyzed using the Cox proportional hazards regression model to determine the independent prognostic factors of MBO caused by colorectal cancer.
RESULTS
Clinicopathological features
A total of 61 patients with GI cancer were enrolled in this study. Of the 61 patients, 38 were male and 23 were female. Patient ages ranged from 19 to 88 years, with an average age of 59.6 ± 11.5 years and a median age of 61 years. The clinical and pathological data of all the patients in this study are shown in Table 1.
Evaluation of surgical effectiveness and survival analysis
In the MDS group, 3 patients showed no evidence of disease. The overall symptom improvement rate was 75.4% (46/51). The overall symptom improvement rate in the MDS group was significantly higher than in OBS group (90%vs61.3%, respectively,P= 0.016). Re-obstruction occurred in 3 patients after the operation, including 2 in the OBS group and 1 in the MDS group.
Ten patients, including 4 patients in OBS group and 6 patients in the MDS group,continued medical treatment and radiotherapy after the operation. By the final followup in June 2019, 38 of the 61 patients had died. The median survival time of the whole group was 6.5 mo, and the 6-mo survival rate was 56.5% (Figure 1A). Patients with colorectal cancer had significant longer median survival than gastric cancer (10.6 movs1.8 mo,P= 0.015, Figure 1B). Patients in MDS group had significant longer median survival than in OBS group (10.9 movs5.3 mo,P= 0.05, Figure 1C). Patients with improvement of symptoms after operation had significant longer median survival than those without (10.9 movs3.9 mo,P= 0.007, Figure 1D).
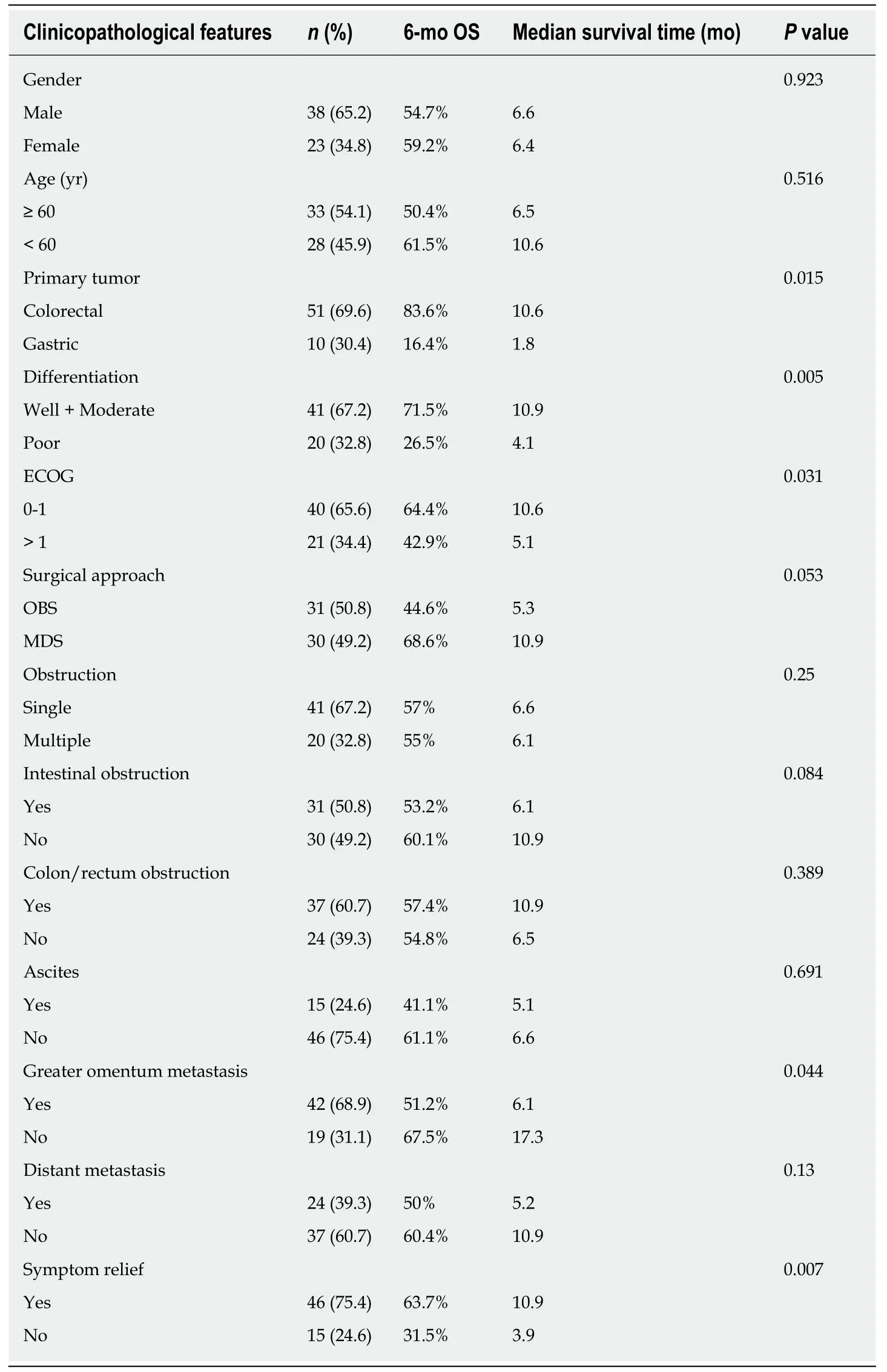
Table 1 Clinicopathological features and survival of 61 malignant bowel obstruction cases
Postoperative mortality and morbidity
In this cohort, 32 patients had complications within 30-d of surgery. In the MDS group, 1 patient had secondary surgery due to wound infection.
The overall complication rates in the MDS and OBS groups were 48.4% (15/31) and 56.7% (17/30), respectively. There was no significant difference between the two groups (P= 0.611). The mortality rates within 30 days of the operation in the MDS and OBS groups were 19.4% (6/31) and 6.7% (2/30), respectively. There was no significant difference between the two groups (P= 0.255, Table 2).
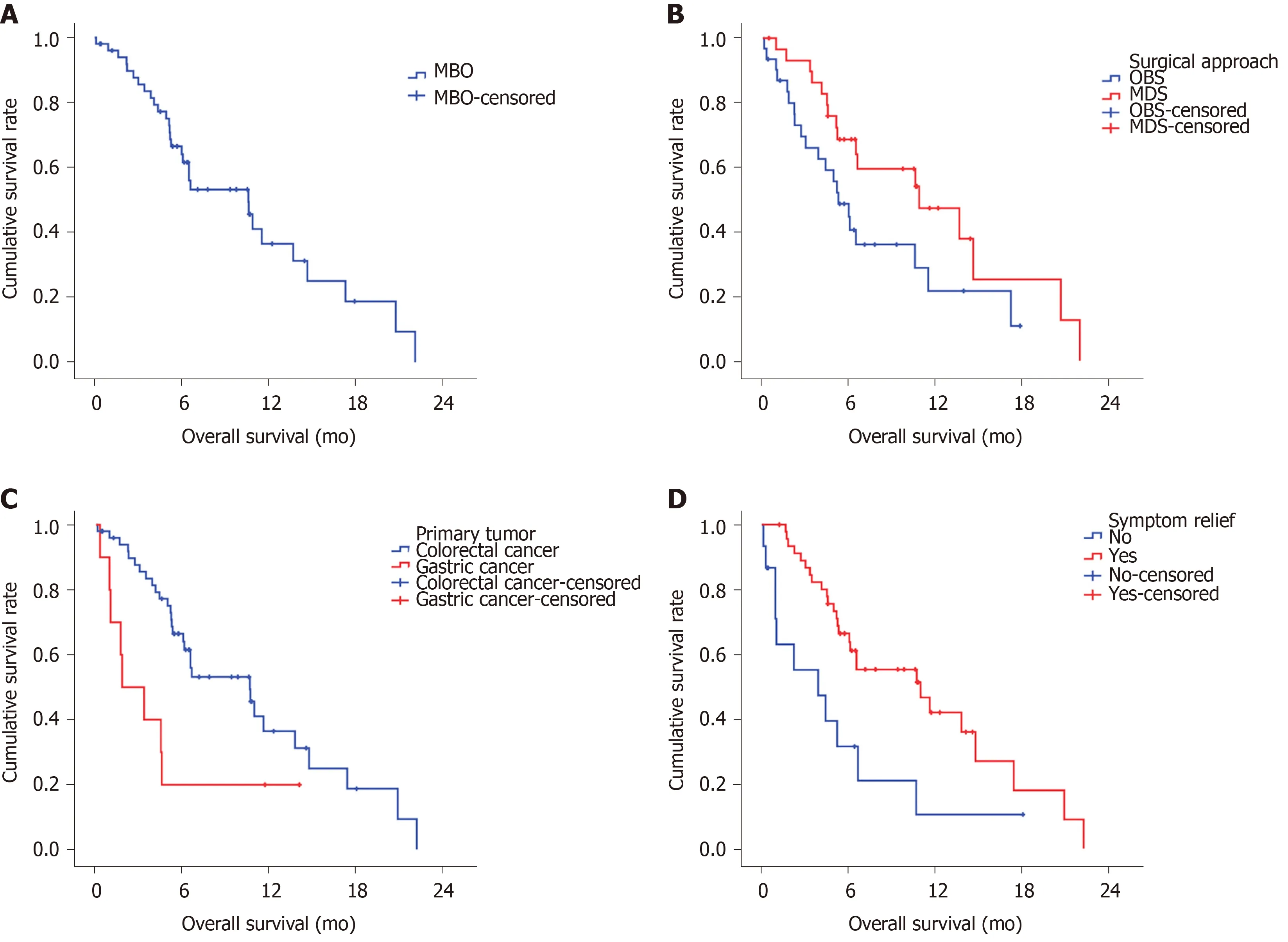
Figure 1 Kaplan-Meier curves of overall survival for patients.
Because of the short survival time of patients with gastric cancer, we conducted a univariate analysis of MBO in patients with colorectal cancer, and found that surgical approach [hazard ratio (HR) = 2.301, 95%CI: 0.999-5.299,P= 0.05], differentiation (HR= 8.509, 95%CI: 2.455-26.448,P= 0.001), greater omentum metastasis (HR = 7.718,95%CI: 2.224-26.782,P= 0.001) and distant organ metastasis (HR = 2.375, 95%CI:1.022-5.253,P= 0.044, Table 3) were independent prognostic factors for MBO caused by metastatic colorectal cancer (mCRC).
DISCUSSION
MBO patients represent a complex and heterogeneous population, and there are no evidence-based guidelines to help with the decision-making process for clinical management of the disease. Previous studies have reported on the effectiveness of palliative surgery for MBO, most of which focused on gynecologic and GI cancer populations[17-19]. However, there is little data on palliative surgery for MBO in colorectal cancer patients and most of the literature that included colorectal cancer combined several types of malignancies.
In this cohort study focused on GI cancer, we observed higher symptom relief rates and prolonged survival after MDS compared with OBS in MBO patients. For select patients with MBO caused by peritoneal mCRC, MDS can result in higher symptom palliation rates and prolonged survival without increasing mortality and morbidity rates compared with OBS. However, because of the short survival time of GI cancer patients, no surgical intervention which may cause a patient to spend the remainder of their life in the hospital should be seriously considered.
The priority of care for inoperable and conservative MBO patients is to control their symptoms and improve their QOL. Medical treatment combining total parenteral nutrition, opioids, antiemetics, and somatostatin drugs is usually considered to be the preferred treatment[20]. The primary goals in palliative surgery are symptom relief and the restoration of oral feeding. Single site obstructions can be resolved by endoscopic treatment and ostomy[21,22]. However, some patients with complete obstructions mayhave multiple sites that are occlusive, and therefore, tumor reduction surgery becomes a necessity.
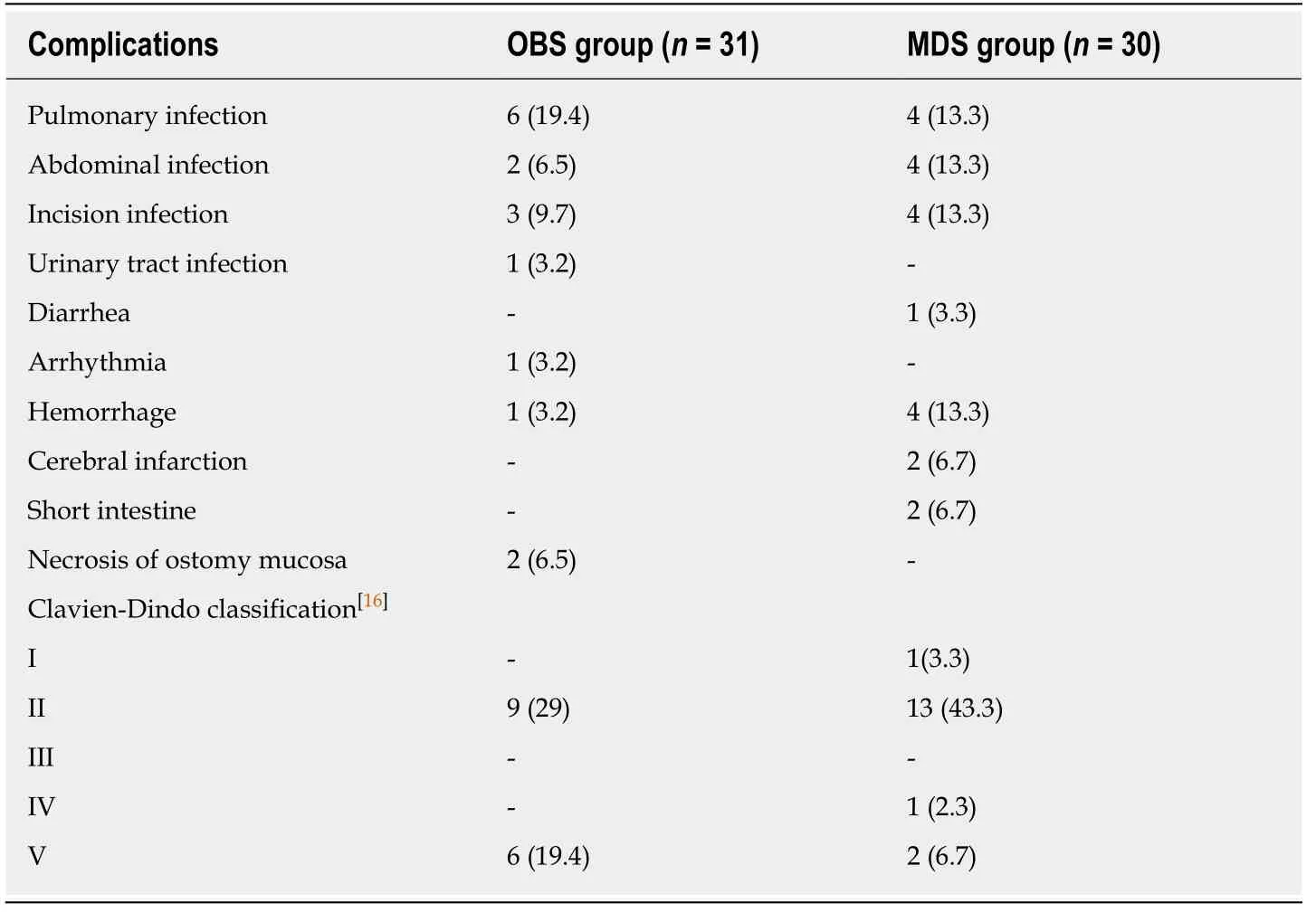
Table 2 Sixty-one cases of complications after surgery, n (%)
The overall symptom relief rate of all the patients included in this study was 76.1%.The MDS group achieved a higher symptom relief rate than the OBS group (91.3%vs60.9%, respectively), which was higher than that reported in the literature[15]. The reobstruction rate was 6.5% in this group, which was lower than the 9% reported in the literature[23]. In this group, although the obstructions were removed, the symptom improvement rate in the OBS group was not high, and 40% of these patients still needed parenteral nutritional support.
Previous studies reported that the median survival for MBO patients treated with conservative care was no longer than 4–5 wk[24]. For some MBO patients, surgical intervention can prolong survival[1,4,25-27]. In this study, the overall median survival time was 6.5 mo. The patients who underwent MDS had a longer survival time than those who underwent OBS (median survival time was 11.5 movs5.1 mo,respectively), and a longer survival time than those reported in previous literature (4-9 mo)[28,29].
In this cohort, the patients that showed significant symptom improvement and good oral food intake had significantly longer survival times than those who did not.This indicates that palliative surgery, although aimed at relieving symptoms, has also prolonged survival, likely due to the improvement in nutrition and subsequent systemic treatment. These results were in accordance with the literature[26]. However,due to the high heterogeneity of patients with malignant intestinal obstructions, it is usually difficult for surgeons to determine the best surgical approach before the operation is performed[5].
Although MDS and OBS can improve the QOL and potentially the survival time,these benefits are accompanied by high mortality and complication rates. In this study, the 30-d postoperative complication rates were as high as 54.3% and 13%,respectively, which are similar to those reported in previous literature (6%-40%) and 5%-15%, respectively[5,18,28,30]. Notably, patients undergoing OBS had comparable complication rate and mortality after surgery as patients in the MDS group,suggesting that the short-term prognosis of patients cannot be overlooked.
Much of the literature defines surgical benefit as at least 60 d of survival after the operation. In this cohort, the median survival of gastric cancer patients was only 1.8 mo, suggesting surgery should not be routinely undertaken in patients with end-stage gastric cancer. However, MBO patients with colorectal cancer may benefit from surgical intervention especially for select patients that can withstand treatment with MDS. Previous studies have suggested candidate prognostic indicators that a patient has a low likelihood of benefiting from surgery for MBO. Age, surgical treatment,ascites, low albumin, hypoproteinemia, and primary tumors are reported to be the main prognostic factors. The number of combined risk factors determines survivalrates and the incidence rates of short-term complications after surgery[6,18,27,28,31]. Before any palliative surgical intervention is performed, the feasibility of surgery and the probability that a patient will benefit not only from an improvement in QOL but in terms of survival should be taken into consideration[32]. In this cohort, survival analysis showed that the primary tumor site, differentiation, the surgical approach,the ECOG score and greater omentum metastasis were the prognostic factors for MBO patients with GI cancer. Whereas in mCRC, differentiation, surgical approach, greater omentum metastasis and distant organ metastasis were the most important independent prognostic factors.

Table 3 Multivariable analysis prognostic factors of 51 malignant bowel obstruction colorectal cancer patients
The limitations of this study were the small sample size and the high heterogeneity of the patients. We lacked the data on the use of medical antineoplastic drugs and the patientKARS/BRAFstatus. There may also be selection bias that affects the conclusions. Although symptom relief and survival benefit were observed in this group, the risk of serious complications and mortality cannot be ignored. Surgeons should fully weigh the life-expectancy, potential benefits and risks, and the QOL of patients after the operation. The aim of surgical and other approaches must be considered and prioritized based on each patient’s and family’s goals and preferences.Although surgeons usually actively treat postoperative complications, it is may be unacceptable for some patients with end-stage diseases spending the rest life in hospital.
Because of the patient heterogeneity, it seems impossible to conduct a random study of malignant intestinal obstruction. In the future, registry studies may be needed to provide high-level evidence about the treatment of MBO and the QOL of patients should be taken into account.
In conclusion, because of the short expected-survival time for patients with gastric cancer and MBO, the high perioperative complication and mortality rates should be seriously considered before any surgical intervention is performed even for an ostomy. For select patients with MBO caused by peritoneal mCRC, MDS may result in high symptom palliation rates and prolonged survival compared with OBS, without increasing mortality and morbidity rates.
ARTICLE HIGHLIGHTS
Research background
Malignant bowel obstruction (MBO) is a frequent event for end-stage malignant cancers. There is no consensus on the optimal treatment strategy for improving quality of life and prolonging survival. There were fewer studies focused on the surgical intervention of MBO with gastrointestinal (GI) cancers.
Research motivation
We wanted to investigate the effects of palliative surgery for MBO in patients with GI cancers in order to guide treatment.
Research objectives
To define the surgical outcome difference between massive debulking surgery (MDS) and ostomy/by-pass surgery (OBS) for MBO patients with GI cancer.
Research methods
MBO patients with GI cancer receive palliative surgery were included MDS group and OBS group. This study mainly investigated the difference of short outcome and survival between the two groups.
Research results
This study reported that patients in the MDS group had significantly higher symptom palliation rate than OBS group, and the median survival time in the MDS group was significantly longer than in the OBS group.
Research conclusions
Massive debulking surgery can significantly improve symptom and prolong survival for MBO patients with colorectal cancer, without increasing mortality and morbidity rates compared with ostomy/by-pass surgery. However, MDS had no such advantage in gastric cancer.
Research perspectives
The treatment of MBO remained controversial and no well-evidenced. This small sample study demonstrates the effectiveness, safety and survival benefit of massive debulking surgery in colorectal cancer patients with MBO. It is difficult to carry out large sample randomized controlled study. In the future, it is necessary to establish a large sample registration study.
 World Journal of Gastrointestinal Oncology2020年3期
World Journal of Gastrointestinal Oncology2020年3期
- World Journal of Gastrointestinal Oncology的其它文章
- Utility of positron emission tomography-computed tomography scan in detecting residual hepatocellular carcinoma post treatment: Series of case reports
- Clinical outcomes of patients with duodenal adenocarcinoma and intestinal-type papilla of Vater adenocarcinoma
- FOLFOXIRI vs FOLFIRINOX as first-line chemotherapy in patients with advanced pancreatic cancer: A population-based cohort study
- Impact of preoperative chemoradiotherapy using concurrent S-1 and CPT-11 on long-term clinical outcomes in locally advanced rectal cancer
- Circulating cytokines and outcome in metastatic colorectal cancer patients treated with regorafenib
- Association between interleukin-21 gene rs907715 polymorphism and gastric precancerous lesions in a Chinese population
