The research idea of Xuebijing injection in influencing severe pneumonia-pulmonary fibrosis with blood stasis syndrome evolution by inhibiting inflammation, endotoxin and dispersing blood stasis
Rui Zheng, Chengyu Li, Ping Wang, Min Li, Pengqian Wang,5, Changming Zhong, Jianxun Wang, Hongcai Shang*
REVIEW
The research idea of Xuebijing injection in influencing severe pneumonia-pulmonary fibrosis with blood stasis syndrome evolution by inhibiting inflammation, endotoxin and dispersing blood stasis
Rui Zheng1, Chengyu Li2, Ping Wang3, Min Li4, Pengqian Wang1,5, Changming Zhong1, Jianxun Wang3, Hongcai Shang1*
1Key Laboratory of Chinese Internal Medicine of Ministry of Education and Beijing, Dongzhimen Hospital, Beijing University of Chinese Medicine, Beijing, China;2Tianjin Chase Sun Pharmaceutical Co., Ltd, Tianjin, China;3School of Life Sciences, Beijing University of Chinese Medicine, Fangshan District, Beijing, China;4Department of Cardiology, Third Affiliated Hospital of Beijing University of Chinese Medicine, Beijing, China;5Institute of Chinese Materia Medica, China Academy of Chinese Medical Sciences, Beijing, China.
Severe pneumonia is one of the most serious infectious diseases. Delayed intervention may lead to pulmonary fibrosis, which greatly threatens people’s life and health. Blood stasis syndrome is an important underlying syndrome throughout the evolution of severe pneumonia-pulmonary fibrosis. Xuebijing injection (XBJ) was developed under the theoretical system of “Three syndromes and three methods”, demonstrating a good efficacy in treating severe pneumonia and pulmonary fibrosis due to its effect of removing blood stasis and dispersing toxins. Previous studies have shown that XBJ can protect vascular endothelial function, improve coagulation function and regulate immunity by inhibiting inflammatory. Hence, the research hypothesis is put forward that XBJ treats blood stasis syndrome by removing blood stasis and dredging blood vessels, to inhibit the disease progress of severe pneumonia to pulmonary fibrosis. Further researches are need to confirm the function and explore the mechanism of XBJ.
Xuebijing injection, Severe pneumonia, Pulmonary fibrosis, Blood stasis syndrome, Coagulation

Background
Severe pneumonia (SP) is one of the most serious infectious diseases. It is mainly caused by the infection of bacteria, viruses and fungi in the terminal airway. It characterizes by acute onset, complex condition, many complications and poor prognosis. Deterioration of SP can develop intopulmonary fibrosis (PF) [1]. PF is the end-stage condition of interstitial lung disease featured by fibroblast proliferation, a large number of extracellular matrix (ECM) accumulation, inflammatory damage and tissue structure destruction, which is the structural abnormality caused by abnormal repair of normal alveolar tissue.
The progression mechanism of severe pneumonia-pulmonary fibrosis
The progression of severe pneumonia-pulmonary fibrosis
Severe inflammatory reaction caused by SP results in lung tissue damage, structural damage and various cytokines release. Transforming growth factor-β1 (TGF-β1) activates mesenchymal cells to differentiate into myofibroblasts (MFB), which synthesizes numerous ECM and promotes the adhesion between ECM and cells.In addition, tumor necrosis factor-α (TNF-α) can activate the secretion of alveolar macrophages, leading to the cascade reaction of cytokines in the early stage of disease [2]. Various cytokines, growth factors, proinflammatory mediators and chemokines play important roles in the formation of tissue repairing with interstitial cell accumulation, leading to the formation of PF.
Blood stasis syndrome (BSS) running through the evolution of SP to PF
SP is caused by the lung Qi deficiency and weakness of protective-energy. The invasion of external pathogenic factors disorders lung Qi normal movement and impairs diffusion of fluid. The closing of lung Qi changes into noxious heat and further leads to phlegm, retained fluid and blood stasis. The etiology and pathogenesis of SP are blood stasis, phlegm, heat and toxin. The BSS runs through the whole course of pneumonia and ranks high in the syndrome elements of SP [3, 4]. With the duration of disease, the proportion of BSS [5] is keeping rising, demonstrating the key factor for the deterioration of SP [6].
The syndrome of PF is based on Qi deficiency and blood stasis. The common syndrome and main pathogenesis of PF is BSS [7]. Blood stasis is not only the pathological product, but also an important pathological factor of PF [8]. Blood stasis leads to abnormal Qi movement, resulting in inefficiency of lung nourishment, and accumulation of inner heat and toxin. It leads to the deficiency of both lung Qi and Yin and gradually develops into PF. Therefore, removing blood stasis is the key point of the treatment and prognosis of SP to PF.
BSS includes coagulation, fibrinolysis and microcirculation abnormality, which indicates blood circulation stagnation. At the beginning of invasive inflammation, a large number of capillaries appear endothelial damage, endothelial cell activation, and vascular leakage. In view of BSS, traditional Chinese medicine adopts the method of promoting blood circulation and removing blood stasis. It can not only improve the imbalance of coagulation/anticoagulation, inhibiting the release of harmful vasoactive medium, but also block different factors from activation in coagulation dysfunction [9]. This method plays a significant role in different stages of coagulation dysfunction.
The theoretical basis of “the co-regulation of inflammation, toxin and blood stasis”
Xuebijinginjection (XBJ) is developed according to the theory of “three syndromes and three methods”. It is composed of five Chinese herbal extractions, which are Honghua (), Chishao (), Danshen (), Danggui () and Chuanxiong ().acts as the monarch herb, promoting blood circulation and removing blood stasis.andare the ministerial drug which can cool blood, disperse blood stasis, detoxify the body, and helpto activate blood and Qi.andare adjuvants, which can nourish the blood, strengthen the body and remove blood stasis. The combination plays the functions of activating blood circulation, removing blood stasis, unblocking circulation tracts and dispersing toxin.
“Three syndromes and three methods” includes: ① the method of clearing away heat and detoxifying in treating toxic heat syndrome; ② the method of improving blood circulation and dispersing stasis in treating BSS; ③ the method of strengthening the body resistance in treating acute deficiency patterns. The key point of transformation is from “toxic heat syndrome” to “blood stasis syndrome” [10].
Furthermore, the theory of “Inhibiting the bacteria, endotoxin and inflammatory” was put forward [11]. In terms of pathological mechanism of SP, Prof. Li explained the process from “toxic heat syndrome” (inflammation storm) to “BSS” (coagulation disorder, diffuse intravascular coagulation), and finally to “acute deficiency syndrome” (shock, multiple organ dysfunction syndrome). BSS is considered as the watershed of the development of severe disease. The generation of BSS is mainly due to the injury of endothelial cells of blood vessels by inflammatory mediators, which affects the coagulation system, leading to the disorder of coagulation function.
The mechanism of “co-regulation of inflammation, toxin and blood stasis”
The main chemical components of XBJ are hydroxysafflor yellow A, paeoniflorin, Senkyunolide Ⅰ, tanshinol, ferulic acid, etc. It has been shown to produce anti-inflammatory effect, protectvascular endothelium, regulate blood coagulation, and immunity by the mechanism of “multi-component, multi-target and multi-pathway” [12]. XBJ is a representative drug of BSStreatment in the theory of “Co-therapy of Bacteria, toxin, inflammatory factors” and “Three Syndromes and Three Methods” [13, 14]. XBJ has been proven to cut off the bound between severe infection and coagulation disorders. It also can improve immune function and have antioxidation function. Details are showed in Figure 1.
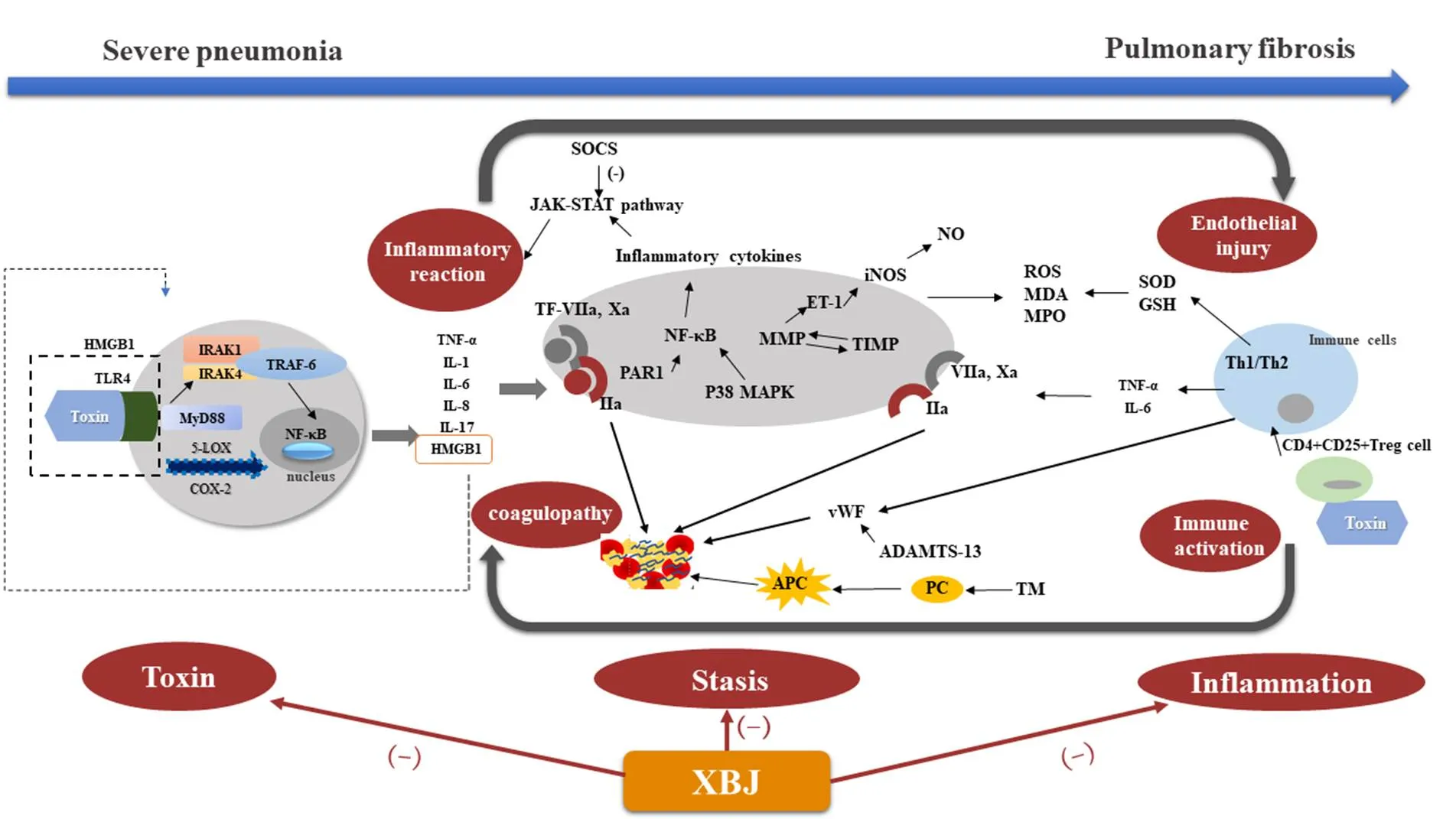
Figure 1 The mechanism of XBJ in influencing SF-PF with blood stasis syndrome evolution by inhabiting inflammation, endotoxin and dispersing blood stasis (5-LOX, 5-lipoxygenase; VⅡa, Xa, Ⅱa are coagulation factors; ADAMTS-13, von willebrand factor-cleaving protease; APC, Activated protein C; COX-2, cyclooxygenase-2; ET-1, endothelin-1; GSH, Glutathione; HMGB1, High mobility group box protein 1; IL, interleukin; iNOS, inducible nitric oxide synthase; IRAK1, Interleukin-1 receptor associated kinase; IRAK4, Interleukin-4 receptor associated kinase; MDA, Malondialdehyde; MMP, Matrix Metalloproteinase; MPO, myeloperoxidase; MyD88, Myeloid differentiation factor 88; NF-κB, Nuclear factor kappa B; PAR, Protease-activated receptor; PC, Protein C; ROS, reactive oxygen species; SOD, superoxides dismutase; SOCS, Suppressor of cytokine signaling; TF, Tissue Factor; Th1/Th2, T helper cells 1/T helper cells 2; TIMP, tissue inhibitor of metalloproteinase; TLR4, Toll-like receptor 4; TM, thrombomodulin; TNF-α, Tumor Necrosis Factor-α; TRAF-6, TNF receptor associated factor-6; vWF, von Willebrand factor.)
Inhibiting inflammation
XBJ can antagonize endotoxin and inhibit the expression of many inflammatory factors, such as TNF-α, IL-1, IL-6, IL-8 and IL-17. It also reduces the expression of high mobility group box protein 1 (HMGB1) and inhibits TLR4-NF-κB pathway [15-17]. XBJ can regulate the secretion of inflammatory factors by promoting Suppressor of cytokine signaling (SOCS) to feedback regulate JAK-STAT pathway [18]. It reduces platelet aggregation, removes oxygen free radicals, protects vascular endothelial function and eliminates a series of procoagulant factors, thereby restoring the dynamic balance of the coagulation and fibrinolytic system [19].
Protecting vascular endothelial function
XBJ restores the balance of matrix metalloproteinase (MMP) and tissue inhibitor of metalloproteinase (TIMP)[20, 21].It plays a protective role in vascular endothelium by reducing endothelin-1 (ET-1), inducible nitric oxide synthetase (iNOS) and nitric oxide (NO)[22-24].
Regulating immune function
XBJ can improve the immune function by raising the proportion of Th1 cells, then increasing Th1/Th2 ratio in sepsis rats [25, 26]. It further improves the immune function of patients by promoting the apoptosis of CD4+CD25+T cells (Tregs) [27, 28], and inhibiting the expression of apoptosis-related proteins such as Fas, Bax, PD-1, decreasing the apoptosis of T cells and neutrophils [25, 29-31]. XBJ can also regulate the differentiation balance of T cell (Treg) and Th17 to reduce inflammatory factor levels. Thus it protects organs function and improve survival rate in sepsis mice [32]. It has also been proved that the combination of XBJ can significantly increase the level of CD3+CD4+and CD4+/CD8+T cells, improve the immune function of patients, and reduce the inflammatory response in clinical trials [33].
Improving coagulation function
XBJ reduceshypercoagulable state in sepsis rats, by reducing the secretion of tissue factor (TF), down-regulating TF, catalyst protein disulfide isomerase (PDI)and protease activated receptor 1 (PAR-1)[34, 35]. XBJ can also increase the level of plasma activated protein C (APC), von Willebrand factor lysing protease (ADAMTS-13) and reduce the level of thrombomodulin (TM), von Willebrand factor (vWF) and the expression of endothelial protein C receptor (EPCR) in sepsis rats. It plays a key role in improving coagulation abnormalities [36-39].
Evidence basis of XBJ in the treatment of SP-PF evolution
The result of a three-year long randomized controlled trials of XBJ versus placebo for critically ill patients with SP, with 33 hospitals and 710 patients enrolled, was published in Critical Care Medicine[40]. It showed that XBJ combined with routine treatment could significantly reduce the 28-day mortality of patients with SP by 8.8% (95% CI 2.4%-15.2%,= 0.006), increase the improvement rate of pneumonia severity index (PSI) by 14.4% (95% CI 6.9%-21.8%,< 0.001), and reduce the mechanical ventilation time and ICU hospitalization time by 5.5 days (= 0.012) and 4 days (= 0.004) respectively.
XBJ has also been used for the treatment of PF, especially ones caused by acute poisoning. A meta-analysis of clinical efficacy of XBJ in treatment of acute paraquat poisoning, which included 27 studies and a total of 1429 patients, showed compared with conventional treatment alone, combination with XBJ could reduce the 14-day mortality (RR = 0.62, 95%CI 0.54-0.72,< 0.000)and the incidence of PF (RR = 0.57, 95%CI 0.53-0.85,= 0.001), improving the oxygenation level of patients furthermore [41]. Some scholars have confirmed that XBJ could delay the process of PF by inhibiting the inflammatory reaction of acute lung injury in PF rats induced by oleic acid, presenting organ protection function[42]. Li used one-off intratracheal injection of bleomycin to prepare the rate model of acute PF. It was demonstrated that XBJ combined with prostaglandin E1 could alleviate early inflammatory response and collagen production by inhibiting the expression of TNF-α and TGF-β1, effectively improve the pathological changes of PF and slow the deterioration process [43].
The efficacy of XBJ in the treatment of SF has been recognized has received widely recognition. Since 2013, it has been included in 11 treatment guidelines or expert consensus about SF [44]. XBJ was recommended for pneumonia in China Association of Chinese Medicine Announcement for Standards Clinical Practice Guideline [45].XBJ can reduce the content of hydroxyproline (Hyp) in lung tissue and inhibit the expression of TNF-α, TGF-β1and ERK to protect lung tissue andinhibit fibrosis [46]. So XBJ was recommended in Expert consensus on diagnosis and treatment of acute paraquat poisoning (2013) [47].
Conclusion
Based on the existing research, XBJ has the characteristics of “multi-component, multi-target and multi-pathway”. The evolution of BSS of SP to PF can be interfered by XBJ through inhibiting inflammation, protecting vascular endothelial function, regulating immune function and coagulation function. Based on the theoretical basis of “Three syndromes and three methods” and “Inhibiting the bacteria, endotoxin and inflammatory”, we propose that XBJ is characterized by its main effect of promoting blood circulation and removing blood stasis, represents as “inhibiting inflammation, endotoxin and dispersing blood stasis”. XBJ can be used to prevent the occurrence and progress of SP to PF with BSS, so as to achieve the “prevention before disease onset, prevention disease from exacerbating” therapeutic purpose.
1. Yang J, Ceng F, Huang K. A nursing care case of double lung transplantation assisted by extracorporeal membrane oxygenation in the abnormal period of pulmonary fibrosis secondary to severe pneumonia. J of Nurs and Reha 2019, 18: 92-94. (Chinese)
2. Zhang L, Lang Z, Sun L, et al. Pathological study of pulmonary fibrosis in severe acute respiratory syndrome. Chin J of Infe Dise 2005, P: 46-48.(Chinese)
3. Luo Q. TCM syndrome distribution regularity of severe pneuminia and risk factor analysis. Guangzhou Univ of Chin Med 2015. (Chinese)
4. Fan XL. The research of distribution law of TCM syndrome elements and the relationship with prognostic factors of severe pneumonia. China academy of Chin medl sci 2014. (Chinese)
5. Lu J. Clinical characteristics of pulmonary interstitial fibrosis in Chinese and Western medicine. Nanjing Univ of Chin Med 2018. (Chinese)
6. Zhang W, Wang YG, Liu QQ, et al. TCM Syndromes and Etiology-Pathogenesis of Severe and Critical Cases of Influenza A(H1N1): An Analysis of123Cases. J of Trad Chin Med 2011, 52: 35-38. (Chinese)
7. Fu XF, Zhou L, Liu XT, et al. Investigation and analysis on TCM syndrome manifestations in 61 patients with pulmonary interstitial fibrosis. Modern Chin Clinical Med 2010, 17: 1-4. (Chinese)
8. Meng LH, Jiang LD, Zhang XM. Microscopic study of blood stasis syndrome of pulmonary interstitial fibrosis. Global Trad Chin Med 2017, 10: 1202-1204. (Chinese)
9. Zhang Q, Li J, Liang X, et al. The preventive effect of Chinese herbal preparation Xuebijing against hyperactive inflammation after hepato-pancreato-biliary surgery. Ann Transl Med 2019, 7: 2305-5839.
10. Li Y, Wang J, Li Z. Treatment of sepsis based on syndrome differentiation of "three syndromes and three methods". Chin Crit Care Med 2006, 18: 643-644. (Chinese)
11. Li Z, Ren X, Li Y, et al. Research progress in the treatment of sepsis with "three syndromes and three methods" and "co-treatment of bacterial, toxin, inflammation". Chin J TCM WM Crit Care, 2012, 19: 321-323. (Chinese)
12. Ma S, Yu H, Zhang X, et al. Study on the material basis of Xuebijing and the multi-target effect of sepsis. Chin J of Integrative Med 2015, 35: 1351-1355. (Chinese)
13. Wang J, Xue L. Bacteria, endotoxin and inflammatory factors: a new strategy for the treatment of severe sepsis. Chin Critical Care Med 1998, 10: 323-325. (Chinese)
14. Lin X. Research of the new strategy for the treatment of systemic inflammatory response syndrome and multiple organ dysfunction syndrome: an experimental study of the effect of traditional Chinese herb- “Xue bi jing”. Chin Crit Care Med 1997, P: 18-20, 64. (Chinese)
15. Ou Y, Huang Y, Su W, et al. Effect of Xuebijing Injection on TLR4 signaling pathway mediated intestinal mucosal barrier dysfunction in SAP rats. Ghuangzhou Med J 2019, 50: 1-5. (Chinese)
16. Sun M, Tu Y, Ou Y, et al. The effect of Xuebijing injection and its pharmacokinetics on the expression of TNF-α, IL-1, IL-6, IL-8 and IL-10 in sepsis rats. J of Tianjin Univ of Trad Chin Med 2018, 37: 13-15. (Chinese)
17. Wang Q, Wu X, Tong X, et al. Xuebijing ameliorates sepsis-induced lung injury by downregulating HMGB1 and RAGE expressions in mice. eCAM, 2015, Article ID:860259.
18. Li A, Li J, Bao Y, et al. Xuebijing injection alleviates cytokine-induced inflammatory liver injury in CLP-induced septic rats through induction of suppressor of cytokine signaling 1. Exp Ther Med 2016, 12: 1531-1536.
19. He J. The Study of Xuebijing Injection Effecting Hemodynamics and Correlation with Endothelial function in Severe Sepsis. Guangzhou Univ of Chin Med 2014. (Chinese)
20. Hou J, Song Z, Zhang Y, et al. The effect of Xuebijing on MMP-9 level in sepsis rats and its protective effect on lung. Hebei Med 2014, 36: 645-647. (Chinese)
21. Sun Q, Zuo H, Tang L, et al. The expression of matrix metalloproteinases in the lung of the rats with vibrio vulnificus sepsis and the intervention of Xuebijing injection. Chin J of Emer Med 2011, 4: 385-390. (Chinese)
22. Wang W, Zhang Y, Li H, et al. Effect and possible mechanism of Xuebijing on acute lung injury in early sepsis rats. Progress in Modern Biomed 2017, 17: 4820-4823. (Chinese)
23. Zhao GJ, Li ZW, Sun Q, et al. Effect of Xuebijing injection on inducible nitric oxide synthase activity and nitric oxide levels in lung of rats with Vibrio vulnificus sepsis. Chin J of Inter Chin and West Med 2010, 2: 99-101. (Chinese)
24. Zhu HY, Zheng GJ, Li YP, et al. Effects of Xuebijing injection on expressions of hypoxia inducible factor-1α and its target gene inducible nitric oxide synthase in septic rats. Chinese Chin J of Inter Chin and West Med 2010, 2: 96-98. (Chinese)
25. Liu M, Deng X, Li W, et al. The effect of Xuebijing Injection on the expression of claudin 4 protein and helper T lymphocyte type 1 in sepsis rats. shanghai med, 2015, 38: 133-138. (Chinese)
26. Zhang S, Sun C, Wen Y, et al. Effect of Xuebijing Injection on serum inflammatory mediators and Th1 / 2 in sepsis rats. Chin Crit Care Med 2006, 11: 673-676. (Chinese)
27. Dai XG, Yao YM, Ai YH. Effect of apoptosis of CD4+CD25+regulatory T lymphocytes on polarization of helper T lymphocytes and potential interventional influence of Xuebijing injection in septic rats. Chin Crit Care Med 2009, 3: 135-138. (Chinese)
28. Dai XG, Yao YM, Ai YH. Effect of Xuebijing injection on lipopolysaccharide-induced apoptosis of CD4+CD25+regulatory T cells and immune function of effector T cells in vitro. Chin J of Emer Med 2009, 9: 932-936. (Chinese)
29. He X, Yan P, Zou Q, et al. Effect of Xuebijing on the expression of tumor protein controlled by neutrophil translation in Acinetobacter baumannii septic rats. Chin J of Clin Pharm & Ther 2014, 19: 29-32. (Chinese)
30. Chen XW. Effect of Xuebijing Injection on Apoptosis and PD-1/PD-L1 Expression in T Cells of Rats with Sepsis. Medical information 2014, 26: 233-234. (Chinese)
31. Wang Y, Chang W, Cao S. Experimental study on the effect of Xuebijing on the expression of Fas Bax protein in spleen tissue of sepsis. Chin Crit Care Med 2007, 10: 905-908. (Chinese)
32. Chen X, Feng Y, Shen X, et al. Anti-sepsis protection of Xuebijing injection is mediated by differential regulation of pro- and anti-inflammatory Th17 and T regulatory cells in a murine model of polymicrobial sepsis. J Ethnopharmacol 2018, 211: 358-365.
33. Chen L, Zhuo Y, Ceng Z, et al. Effect of Xuebijing injection combined with ambroxol hydrochloride on the immune function and inflammatory factors in the elderly patients with severe pneumonia. J of Emer in Trad Chin Med 2019, 28: 1411-1413. (Chinese)
34. Chai Y,Li JY,Chai YF, et al. The effect of Xuebijing injection on the procoagulation of tissue factor by inositol-requiring enzyme 1α signaling pathway. Chin J of Emer Med 2018, 2: 159-163. (Chinese)
35. Zhang Z, Shen Q, Zhu J, et al. Effect of Xuebijing on expression of plasminogen activator inhibitor-1 in lung tissue of rats with lipopolysaccharide induced acute lung injury. Chin J of Clin Healthcare 2011, 14: 163-166. (Chinese)
36. Lu J, Yang SJ, An YZ, et al. Effects of blood circulation medicine on early stage circulation and activated protein C in septic rats. China Med 2010, 3: 212-214. (Chinese)
37. Gui YG, Yao YM, Chai YF. A comparison of interference effect between Xuebijing injection and activated protein C on lipopolysaccharide-induced tissue factor and protease activated receptor-1 expressions on monocytes in rats. Chin J of Inter Chin and West Med 2009, 6: 326-329. (Chinese)
38. Li Y, Qiao Y, Wu Z, et al. Effect of Xuebijing Injection on tumor necrosis factor - α and coagulation function in sepsis rats. Chin J of Inter Chin and West Med 2007, 2: 104-107. (Chinese)
39. Li YP, Qiao YJ, Wu ZX, et al. Effects of Xuebijing injection on thrombomodulin and endothelial cell protein C receptor in septic rats. Chin Crit Care Med 2007, 6: 365-368. (Chinese)
40. Song YL, Yao C, Yao YM, et al. XueBiJing Injection Versus Placebo for Critically Ill Patients With Severe Community-Acquired Pneumonia: A Randomized Controlled Trial. Crit Care Med 2019, 47: e735-743.
41. Qian H, Liu B, Shen F, et al. Xuebijing can improve the clinical efficacy and reduce the mortality of acute paraquat poisoning: a meta-analysis of 1429 cases. Chin Crit Care Med 2019, 31: 1416-1422.(Chinese)
42. Wang Y. Effect of Xuebijing on pulmonary fibrosis after acute lung injury in rats. Guangzhou Medical College 2011. (Chinese)
43. Li Z, Liu H, Wang J. Xuebijing combined with prostaglandin E1 in the prevention and treatment of acute pulmonary fibrosis on experimental study. Chin J of Emer Med 2007, 16: 255-259. (Chinese)
44. LIi CY, Zhang XY, Liu S, et al. Current Evidence and Research Prospects of Xuebijing Injection in Treating Novel Coronavirus-infected Pneumonia (COVID-19). World Science and Technology/Modernization of Traditional Chin Med and Materia Med 2020, 22: 11-5699. (Chinese)
45. China Association of Chinese Medicine. The T/CACM standard for Clinical Practice Guideline on Traditional Chinese Medicine Alone or combined with Antibiotics for Patients with Community Acquired Pneumonia. Beijing: China Trad Chin Med Press 2017. (Chinese)
46. Li HX, Wang X. Study on the protective effect of Xuebijing injection on lung injury in rats with acute paraquat poisoning. Modern J of Integrated Trad Chin and Western Med 2019, 28: 1508-1513. (Chinese)
46 Emergency physicians branch of Chinese Medical Association. Expert consensus on diagnosis and treatment of acute paraquat poisoning (2013). Chin J Crit Care Med 2013, 33: 484-487. (Chinese)
Blood stasis syndrome is an important underlying syndrome throughout the evolution of severe pneumonia-pulmonary fibrosis.Xuebijing injection demonstrates a good efficacy in treating severe pneumonia and pulmonary fibrosis due to its effect of removing blood stasis and dispersing toxins. Hence, the research hypothesis is put forward that XBJ treats blood stasis syndrome by removing blood stasis and dredging blood vessels, to inhibit the disease progress of severe pneumonia to pulmonary fibrosis.
Xuebijing injection, an herbal prescription, was developed under the theoretical system of “Three syndromes and three methods”. It is widely used in the treatment of sepsis systemic inflammatory response syndrome, according to Chinese guidelines. The bioactive roles include activating circulation, strengthening and consolidating body resistance, removing blood stasis and clearing away toxins and so on.
:Zheng R, Li CY, Wang P, et al. The research idea of Xuebijing injection in influencing severe pneumonia-pulmonary fibrosis with blood stasis syndrome evolution by inhibiting inflammation, endotoxin and dispersing blood stasis.TMR Modern Herbal Medicine 2020, 3(2): 113-119.
Executive Editor: Chaoyong Wu
Submitted: 27 February 2020,
7 March 2020,
*Correspondence to: Hongcai Shang, Key Laboratory of Chinese Internal Medicine of Ministry of Education, Dongzhimen Hospital Affiliated to Beijing University of Chinese Medicine, No.5 Haiyuncang Hutong, Dongcheng District, Beijing 100700, China. Email: shanghongcai@126.com
Abbreviations: XBJ, Xuebijing injection; SP, Severe pneumonia; PF, pulmonary fibrosis; ECM, extracellular matrix; TGF-β1, Transforming growth factor-β1; TNF-α, tumor necrosis factor-α; BSS, Blood stasis syndrome; HMGB1, high mobility group box protein 1; SOCS, Suppressor of cytokine signaling MMP, matrix metalloproteinase; TIMP, tissue inhibitor of metalloproteinase; ET-1, endothelin-1; iNOS, inducible nitric oxide synthetase; NO, nitric oxide; TF, tissue factor; PDI, protein disulfide isomerase; PAR-1, protease activated receptor 1; APC, plasma activated protein C; ADAMTS-13, von Willebrand factor lysing protease; TM, thrombomodulin; vWF, von Willebrand factor; EPCR, endothelial protein C receptor; PSI, pneumonia severity index; Hyp, hydroxyproline.
Funding: This work was supported by the second batch of “Ten thousand plan”-National high level talents special support plan (W02020052).
Competing interests: Chengyu Li is the employee of Chase Sun Pharmaceuticals. The other authors have no conflicts of interest to declare.
Online: 13 March 2020.
 TMR Modern Herbal Medicine2020年2期
TMR Modern Herbal Medicine2020年2期
- TMR Modern Herbal Medicine的其它文章
- Effects of theophylline/chitosan/β-cyclodextrin microspheres for oral drug delivery on an asthmatic rat model
- Research progress on chemical composition, pharmacological effects of Forsythia suspensa (Thunb.) Vahl and predictive analysis on Q-marker
- The functional components and mechanism of Linderae Radix in treating diabetic nephropathy based on the network pharmacology
- Dendrobium huoshanense improves doxorubicin-induced heart failure in C57BL/6 mice
- The roles of traditional Chinese herbal medications in regulating mitochondrial activity to reverse cancer
