Pembrolizumab - emerging treatment of pulmonary sarcomatoid carcinoma:A case report
Emanuela Cimpeanu,Jibran Ahmed,Wahib Zafar,Adreana DeMarinis,Svetoslav S Bardarov,Shamim Salman,Dennis Bloomfield
Emanuela Cimpeanu,Adreana DeMarinis,Dennis Bloomfield,Department of Internal Medicine,Richmond University Medical Center,Staten Island,NY 10310,United States
Jibran Ahmed,Wahib Zafar,Department of Hematology and Medical Oncology,Westchester Medical Center,Valhalla,NY 10595,United States
Svetoslav S Bardarov,Department of Pathology,Richmond University Medical Center,Staten Island,NY 10310,United States
Shamim Salman,Department of Hematology and Medical Oncology,Richmond University
Medical Center,Staten Island,NY 10310,United States
Dennis Bloomfield,Department of Clinical Research,Richmond University Medical Center,Staten Island,NY 10310,United States
Abstract
Key words: Pembrolizumab;Pulmonary sarcomatoid carcinoma;Programmed deathligand 1;Platinum-based chemotherapy;Non-small-cell lung cancer;Overall survival;Case report
INTRODUCTION
Pulmonary sarcomatoid carcinoma (PSC) represents a high-grade histologic subtype of non-small-cell lung cancer (NSCLC),accounting for only about 1% of NSCLC and 0.4% of all lung cancers in the United States[1,2].Most are diagnosed at advanced stages and have an aggressive clinical course and lower overall survival than other histologic subtypes,even on the rare occasions when discovered incipiently[2].Management of metastatic disease has been challenging,owing to high rates of resistance to conventional platinum-based chemotherapy,which,up to recently,was the preferred treatment option for all metastatic types[2-4].While response to pembrolizumab in the more common subtypes of NSCLC has been reported by several studies,very few have addressed the efficacy of pembrolizumab in PSC.We report a case of excellent response to pembrolizumab in a patient with PSC characterized by programmed death-ligand 1 (PD-L1) expression greater than 50%.
CASE PRESENTATION
Chief Complaints
A 69-year-old man presented with one week's duration of respiratory distress and diffuse,intermittent and non-radiating left upper chest pain.
History of present illness
The patient began experiencing occasional dry cough two months prior to presentation but denied having any other symptoms.
History of past illness
There was a past medical history of 60 pack-year smoking,hypertension,diabetes mellitus type II,hypothyroidism,Parkinson's disease and depression.
Physical examination
The patient had labored and irregular breathing but did not use the accessory muscles of respiration.There was tenderness to palpation of the left chest wall and dullness to percussion in the left upper lung field,with decreased breath sounds,rhonchi and slight wheezing.There was mild diffuse abdominal tenderness,without guarding.
Laboratory examinations
Laboratory workup revealed white blood cell count 22.9 K/uL,hemoglobin 10.8 g/dL,hematocrit 37.0%,platelet count 943 K/uL,erythrocyte sedimentation rate 130,serum potassium 5.4 mmol/L and serum calcium 11.6 mg/dL.
Imaging examinations
Chest computed tomography (CT) demonstrated a solid,heterogeneous,partially necrotic mass occupying the left upper lobe,encasing the left subclavian artery and extending into the left mediastinum (Figure 1A,1B).Abdominal and pelvic CT showed hepatomegaly.There was extensive destruction of the left first rib,with less severe involvement of the left second rib,but no evidence of mediastinal,hilar or axillary adenopathy.
FINAL DIAGNOSIS
Biopsy of the mass revealed a poorly differentiated neoplasm composed predominantly of spindle cells,with rare epithelioid cells and large bizarre nuclei(Figure 2A).The immunohistochemical analysis of the lesion demonstrated that the neoplastic cells were positive for cytokeratin-7 (CK-7) (Figure 2B) but negative for thyroid transcription factor-1,p40,CK20,prostate-specific antigen,and MelanA.In addition,immunohistochemical stains for mesothelial origin,specifically Calretinin,CK5/6 and podoplanin (D2-40) were negative.The negative p40 and CK5/6 also ruled out sarcomatoid squamous cell carcinoma.The neoplastic cells tested positive for PD-L1,with a tumor proportion score greater than 50% (Figure 2C).No mutations in epidermal growth factor receptor (EGFR) exons 18,19 or 21 and KRAS codons 12,13 or 61 were present.An exon 20 insertion was identified but the mass was EGFR T790M-negative.Anaplastic lymphoma kinase (ALK) and receptor tyrosine kinase(ROS) translocations were not performed since EGFR and KRAS mutations are mutually exclusive with these translocations.The tumor was classified as stage IIIa(T4N1M0) PSC.
TREATMENT
IV fluids,Pamidronate and antibiotics were administered,and the patient's condition stabilized.Given multiple medical comorbidities,surgical debulking was not feasible.As the tumor was causing airway compromise,palliative radiation therapy was initiated.The patient was also started on pembrolizumab (200 mg) every 21 d.
OUTCOME AND FOLLOW-UP
A repeat CT scan of the chest after 5 cycles of pembrolizumab showed a decrease of more than 80 percent in the size of the tumor mass (Figure 1C,1D).
Positron emission tomography-CT (PET-CT) scan at the end of 10 cycles showed an even further decrease (Figure 3).The patient has been tolerating pembrolizumab well,with no limiting side-effects and a plan was made to continue the same treatment.At present,14 mo after first coming into the hospital,he remains asymptomatic.
DISCUSSION
When diagnosed,PSCs are frequently bulky,peripherally located and already metastatic,with poor prognosis[1].For a patient like ours,with stage III tumor,overall survival is estimated at 5.8 mo,whereas for stages I-II it is 16.9 mo and for stage IV 5.4 mo[5].The typical patient has a history of heavy smoking[1].PSCs are more widespread in Caucasians (89%) and males (59%)[5].The mean age at diagnosis is 70 years[5].Our patient fits these exact demographics - male,Caucasian,heavy smoker,in his late 60 s and with an advanced malignancy.Improved survival in PSC is seen when tumors are localized,amenable to complete surgical resection,4 cm or less in size,and when patients are not underweight or anemic[6].Our patient was not underweight but lacked other positive prognostic factors.He was,in fact,anemic and had a large,locally-invasive tumor,which put him at increased risk for a less favorable outcome.
Platinum-based chemotherapy has proven disappointing in PSC,with most patients (69%) experiencing disease progression and overall survival being only slightly increased compared to the non-platinum group (7.0vs5.3 mo)[3].Compared to patients not receiving any treatment,platinum-based chemotherapy resulted in a median overall survival of only 51 d longer[7].Decreased survival in PSC has been largely attributed to its aggressive nature as well as chemoresistance[1].The marginal performance of available treatment options warranted a need for new therapeutic strategies.
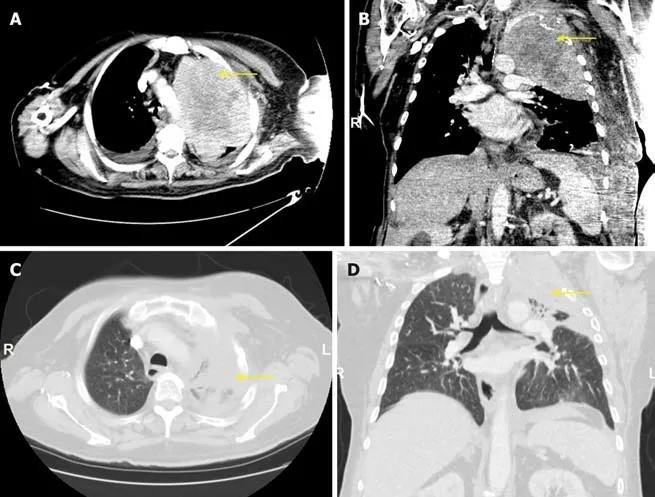
Figure1 Chest computed tomography.
The introduction of pembrolizumab,a monoclonal IgG4 kappa isotype antibody against the Programmed Death 1 pathway,for NSCLC lacking targetable EGFR or ALK mutations has resulted in improved overall survival and progression-free survival for NSCLC with PD-L1 on at least 50% of tumor cells[4,8].Pembrolizumab has become the first-line treatment for such tumor[4].KEYNOTE studies (021,024 and 189)all showed improved treatment response when pembrolizumab was added to platinum-based chemotherapy[4,9,10].In addition,patients on pembrolizumab benefited from increased overall survival,greater response rate,longer duration of response and fewer adverse effects secondary to treatment[10].However,the application of pembrolizumab for PSC has been minimally reported.On a Pubmed search,there are three other individual cases published supporting our contention that pembrolizumab is effective in this previously rapidly fatal tumor[11-13].There are six other cases in which a form of immunotherapy has been used,however,the outcome is unclear[14,15].
For PSCs with mutated EGFR,EGFR tyrosine kinase inhibitors (TKIs) can be a more suitable treatment option[16].Third generation EGFR-TKIs have proven efficacious in tumors with EGFR mutations in exons 19 and 21 as well as exon 20 T790M mutations[17].Osimertinib,a third-generation EGFR-TKI,is particularly indicated for EGFR-mutant NSCLC with an acquired T790M resistance mutation,progressing during or following treatment with EGFR-TKIs[17].Our patient lacked EGFR targetable mutations.The tumor was in fact positive for an EGFR exon 20 insertion,which is seen in about 9% of all EGFR-mutated tumors and has been linked to de-novo resistance to EGFR-TKI[18].For these reasons,EGFR-TKIs were not an appropriate choice.
CONCLUSION
The efficacy of pembrolizumab in the treatment of PSC has not been adequately studied.In our patient,it was proven a highly beneficial form of treatment.He continued to be asymptomatic,more than 14 mo after presentation.To date,this is one of the most sustained responses of PSC to an immune checkpoint inhibitor reported in the English literature.For PSC patients with PD-L1 expression on 50% or more of tumor cells,pembrolizumab is a viable option.
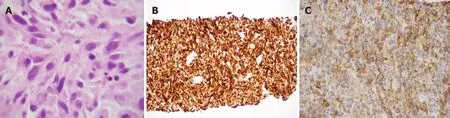
Figure2 Histological lung section.

Figure3 Chest positron emission tomography - computed tomography (lung window) after 9 cycles of pembrolizumab,with the yellow arrow pointing to an fluorodeoxyglucose-avid 5.5 cm × 4 cm mass in the left upper lobe,with central necrosis and a maximum standardized uptake value of 8.6,consistent with malignancy.
 World Journal of Clinical Cases2020年1期
World Journal of Clinical Cases2020年1期
- World Journal of Clinical Cases的其它文章
- Role of oxysterol-binding protein-related proteins in malignant human tumours
- Oncogenic role of Tc17 cells in cervical cancer development
- Acute distal common bile duct angle is risk factor for postendoscopic retrograde cholangiopancreatography pancreatitis in beginner endoscopist
- Three-dimensional computed tomography mapping of posterior malleolar fractures
- Application of a modified surgical position in anterior approach for total cervical artificial disc replacement
- Potential role of the compound Eucommia bone tonic granules in patients with osteoarthritis and osteonecrosis:A retrospective study
