Clinical observation of acupuncture plus repetitive transcranial magnetic stimulation in the treatment of post-stroke insomnia
Zhang Wei (张伟), Ma Kun-qin (马坤琴), Xiao Hong-bo (肖洪波), Li Pei-fang (李佩芳), Gui Mei-lin (桂美琳),Lu Yin-feng (卢尹凤), Chen Rui-quan (陈瑞全), Zhu Zong-jun (朱宗俊)
1 Anhui University of Chinese Medicine, Hefei 230031, China
2 The First Affiliated Hospital of Anhui University of Chinese Medicine, Hefei 230031, China
3 The Second Affiliated Hospital of Anhui University of Chinese Medicine, Hefei 230061, China
Abstract Objective: To evaluate the clinical efficacy of the Governor Vessel-unblocking and mind-regulating acupuncture method plus repetitive transcranial magnetic stimulation (rTMS) in the treatment of post-stroke insomnia.Methods: A total of 72 patients with post-stroke insomnia were randomly divided into 2 groups, with 36 cases in each group. The control group received rTMS treatment with a frequency of 1 Hz and a motion threshold value of 90%. The observation group received acupuncture with Governor Vessel-unblocking and mind-regulating method based on the rTMS treatment of the control group. The points were Baihui (GV 20), Shenting (GV 24), Yintang (GV 29), Fengfu (GV 16),Sishencong (EX-HN 1), Shenmen (HT 7), Sanyinjiao (SP 6), Shenmai (BL 62) and Zhaohai (KI 6). The treatment was performed once a day for 5 d a week followed by 2 d of rest for 4 weeks. The improvements of Pittsburgh sleep quality index (PSQI), self-rating anxiety scale (SAS) and self-rating depression scale (SDS) scores were observed after treatment,and the clinical efficacy was compared between the two groups.Results: After 4 weeks of treatment, the PSQI, SAS, and SDS scores of the two groups were all reduced, and the intra-group differences were statistically significant (all P<0.001). After treatment, the three scores in the observation group were all lower than those in the control group, and the differences between the two groups were statistically significant (P<0.05, P<0.05, P<0.001). There was a statistically significant difference between the observation group and the control group comparing the clinical efficacy (P<0.05).Conclusion: The therapeutic effect of the Governor Vessel-unblocking and mind-regulating acupuncture method plus rTMS in treating post-stroke insomnia is better than rTMS alone, and it can better improve the anxiety and depression of patients.
Keywords: Acupuncture Therapy; Governor Vessel; Insomnia; Depression; Anxiety; Stroke; Complications; Transcranial Magnetic Stimulation
Domestic studies have shown that insomnia is common among stroke patients, and its incidence is as high as 57.9%[1]. Insomnia not only affects the quality of life of stroke patients or prolongs the rehabilitation process of neurological function but also influence other stroke risk factors, such as hypertension,hyperglycemia, and hyperlipidemia, thus leading to the recurrence of stroke[2-3]. At present, the treatment of post-stroke insomnia mainly consists of oral psychotropic drugs, such as estazolam, diazepam,dzopiclone, agomelatine, and metazidine[4], but most of these drugs may cause dependence, tolerance and adverse reactions, and the symptoms tend to relapse once withdrawal[5]. Considering the deficiencies and defects of drug treatment for insomnia, it is urgent to choose an appropriate non-drug treatment protocol[6].After reviewing the literature, we found that the acupuncture method of Governor Vessel-unblocking and mind-regulating had an ideal effect on post-stroke insomnia, and the sleep quality of patients was greatly improved[7].
Repetitive transcranial magnetic stimulation (rTMS),as a non-invasive treatment, has a significant effect on post-stroke insomnia, possibly because it improves insomnia symptoms by improving anxiety and depression and suppressing negative emotions in patients[8]. This study observed the clinical efficacy of acupuncture combined with rTMS in the treatment of post-stroke insomnia, which is summarized as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Western medicine diagnostic criteria
Western medicine diagnostic criteria for post-stroke insomnia referred to the diagnostic criteria for cerebral hemorrhage, cerebral infarction, and insomnia in Neurology[9].
1.1.2 Diagnostic criteria of traditional Chinese medicine (TCM)
Referring to the diagnostic criteria of stroke and insomnia in the Traditional Chinese Internal Medicine[10].
1.2 Inclusion criteria
Met the above diagnostic criteria; aged between 35 and 70 years old; no use of psychiatric drugs, or withdrawal for over 2 weeks; signed the informed consent.
1.3 Exclusion criteria
Consciousness disorders or mental disorders; serious organic diseases and unstable vital signs; pregnancy or lactation; fear of acupuncture or history of fainting during acupuncture sessions; metal implants.
1.4 Statistical methods
All data were analyzed by SPSS version 21.0 statistical software. The measurement data conforming to normal distribution were expressed as mean ± standard deviation (x ±s). If the data met the requirements of normality and homogeneity of variance, the two independent sample t-test was used for inter-group comparison, and the paired t-test was used for intra-group comparison. If normality was not satisfied,the non-parametric test was adopted, and median(lower quartile, upper quartile) was adopted, that is, M(QL, QU) was used to represent. Wilcoxon rank-sum test was used for inter-group comparison, and the paired sample rank-sum test was used for intra-group comparison. The counting data were tested by the Chi-square test. The ranked data were analyzed by Ridit.P<0.05 indicated statistical significance.
1.5 General data
A total of 72 participants with post-stroke insomnia who were admitted to the Department of Acupuncture and Rehabilitation of the First Affiliated Hospital of Anhui University of Chinese Medicine between January 2018 and January 2019 were selected. The participants were randomly divided into two groups with 36 patients in each group using the random number table. The observation group ranged from 35 years old to 64 years old. The shortest duration was 1.3 months, and the longest was 19 months. There were no statistically significant differences between the two groups in general data such as gender, age, and duration of disease (all P>0.05), indicating that the two groups were comparable (Table 1).

Table 1. Comparison of general data between the two groups
2 Treatment Methods
Patients in both groups received basic treatments such as blood pressure regulation, blood sugar control,plaque stabilization, anti-platelet aggregation, and improvement of cerebral circulation[11].
2.1 Observation group
The observation group received the Governor Vesselunblocking and mind-regulating acupuncture method plus rTMS treatment.
2.1.1 rTMS treatment
YD-MT200 transcranial magnetic stimulator (Henan Youde Medical Equipment Co., Ltd., China) was used with 1 Hz and 90% motor threshold (MT) for rTMS treatment.
Treatment site: The coil center was placed at the right dorsolateral prefrontal lobe of the patient, tangential to the treated cortex.
Treatment parameters: 1 400 times of total stimulation pulses per time, once a day, with a 2 d rest after 5 d of treatment per week, for a total of 4 weeks.
2.1.2 Acupuncture
Points: Baihui (GV 20), Shenting (GV 24), Yintang(GV 29), Fengfu (GV 16), Sishencong (EX-HN 1),Shenmen (HT 7), Sanyinjiao (SP 6), Shenmai (BL 62) and Zhaohai (KI 6).
Method: Disposable filiform acupuncture needles of 0.35 mm in diameter and 25-40 mm in length were selected. After routine sterilization, one-hand needling insertion method was used for Baihui (GV 20), and the needle was inserted with an angle of about 15° into 15-20 mm rapidly. The needles at Sishencong (EX-HN 1)were subcutaneously punctured into the epicranial aponeurosis with the tip toward Baihui (GV 20) and the depth of 10-15 mm. Yintang (GV 29) was punctured with pinching insertion method by 10-15 mm. Shenting(GV 24) was punctured toward Yintang (GV 29) at the depth of 15 mm. The needle at Fengfu (GV 16) was gently punctured by 10-15 mm with the needle tip toward the mouth and the patient in relaxation. The depth of insertion can be increased or decreased according to the height and weight of the patient, but not over 5 mm. Shenmen (HT 7) and Sanyinjiao (SP 6)were perpendicularly punctured by 15-20 mm in depth,and Shenmai (BL 62) and Zhaohai (KI 6) were perpendicularly punctured by 10-15 mm in depth. After the needling qi arrived at all points, even reinforcingreducing manipulation was performed. The intensity was determined by the patient’s tolerance. The needles were retained for 30 min. The acupuncture treatment was performed once a day, 5 d a week, followed by 2 d of rest, for a total of 4 weeks.
2.2 Control group
Participants in the control group received the same rTMS treatment as that in the observation group, and the stimulation parameters and treatment course were the same as those in the observation group.
3 Therapeutic Efficacy Observation
3.1 Observation items
All participants were evaluated by the following three assessment tools before and after treatment.3.1.1 Pittsburgh sleep quality index (PSQI)
PSQI was used to assess sleep quality. The questionnaire includes the following seven components:subjective sleep quality, sleep latency, sleep duration,habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. Each component was scored on a scale of 0-3 points, and the sum of each component score was the total PSQI score,ranging from 0 to 21 points. The higher the score, the worse the sleep quality.
3.1.2 Self-rating anxiety scale (SAS)
The SAS was used for anxiety assessment. The questionnaire mainly includes 20 items, which are divided into 1-4 levels according to the frequency of symptoms, gradually increasing. The standard score is calculated by the integer part of the cumulated score multiplied by 1.25. The score <50 points indicates no anxiety, and the higher the score, the more serious the anxiety.
3.1.3 Self-rating depression scale (SDS)
The SDS was used for depression assessment. The scoring method is the same as that of SAS. On a scale of 50 points, the score <50 points indicates no depression.The higher the score, the more severe the depression.
3.2 Criteria of curative efficacy
Efficacy evaluation referred to the Guiding Principles for Clinical Study of New Chinese Medicines[12]and the PSQI reduction rate.
PSQI reduction rate = (Total PSQI score before treatment - Total PSQI score after treatment) ÷ Total PSQI score before treatment × 100%.
Clinical recovery: The sleep time increased to more than 7 h, and the quality was good. The patient felt energetic after waking up, and the PSQI reduction rate was ≥75%.
Markedly effective: The sleep time increased to more than 4 h, the sleep quality improved significantly, and the PSQI reduction rate was ≥50%, but <75%.
Effective: The sleep time increased less than 4 h, the sleep quality improved, and the PSQI reduction rate was≥25%, but <50%.
Failure: No improvement or even worse in sleep time and quality, and the PSQI reduction rate was <25%.
3.3 Clinical results
3.3.1 Comparison of clinical efficacy
During the treatment, no related adverse reactions occurred in the two groups, which showed that both treatments were safe. The comparison of clinical efficacy between the two groups was analyzed by Ridit analysis, t=-2.048, P=0.044, suggesting that the difference between the two groups was statistically significant, and the efficacy of the observation group was better than that of the control group (Table 2).
3.3.2 Comparison of the PSQI score
The result of the Wilcoxon rank-sum test comparing the PSQI score between the two groups before treatment showed Z=-1.451, P=0.147, suggesting that there was no significant difference in the score before treatment between the two groups, and they were comparable. Intra-group comparison was analyzed using the paired sample rank-sum test: the observation group, Z=-5.237, P=0.000, and the control group,Z=-5.243, P=0.000, indicating that the PSQI scores of both groups decreased significantly. Inter-group comparison of the PSQI score after treatment was analyzed using Wilcoxon rank-sum test: Z=-2.164,P=0.030, suggesting a significant difference between the two groups after treatment. See Table 3 for details.
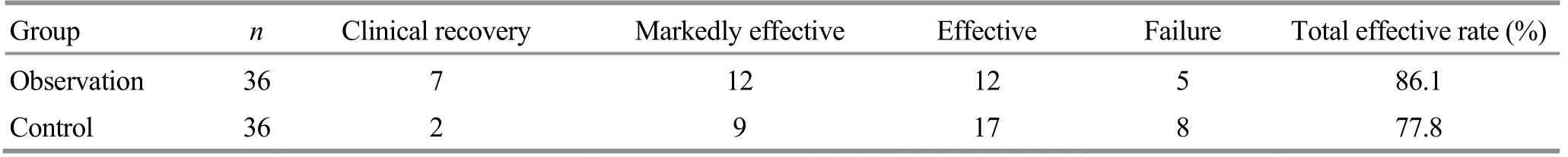
Table 2. Comparison of clinical efficacy between the two groups (case)
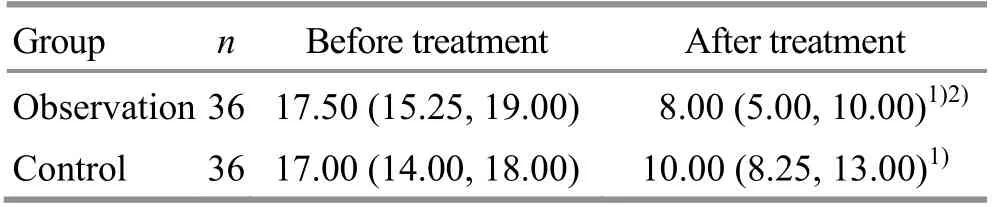
Table 3. Comparison of the PSQI score before and after treatment between the two groups [M (QL, QU), point]
3.3.3 Comparison of SAS and SDS scores
The SAS scores of the two groups before treatment were tested by two independent samples t-test:t=0.335, P=0.739, and the difference was not statistically significant, suggesting that the two groups were comparable. After treatment, the paired t-test was used for intra-group comparison: the observation group, t=12.792, P=0.000, and the control group,t=10.935, P=0.000, indicating that the SAS scores in both groups were significantly reduced. After treatment,two independent samples t-test was used for inter-group comparison of the SAS score (t=-2.590,P=0.012), suggesting that the SAS scores of the two groups were significantly different after treatment. See Table 4 for details.
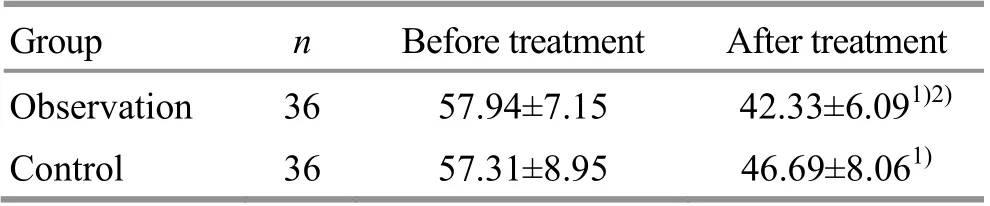
Table 4. Comparison of the SAS score before and after treatment between the two groups (x ±s, point)
Before treatment, the SDS scores of the two groups were tested by Wilcoxon rank-sum test: Z=-0.497,P=0.619, and the difference was not statistically significant, suggesting that the two groups were comparable. The paired sample rank-sum test was used for intra-group comparison after treatment: the observation group, Z=-5.161, P=0.000, and the control group, Z=-5.091, P=0.000, suggesting that the SDS scores of both groups decreased significantly. The SDS score of the observation group after treatment was compared with that of the control group. Wilcoxon rank-sum test showed Z=-5.075, P=0.000, suggesting that there was a significant difference between the two groups after treatment. See Table 5 for details.
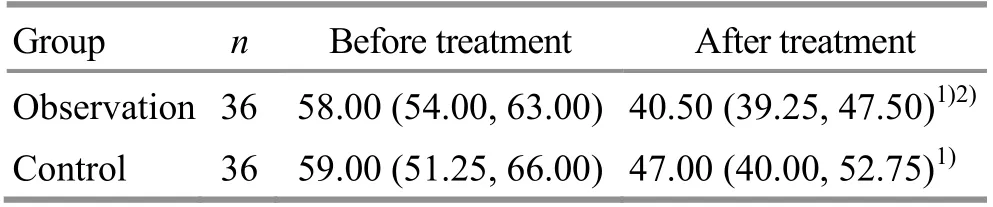
Table 5. Comparison of the SDS score before and after treatment between the two groups [M (QL, QU), point]
4 Discussion
Although insomnia is not classified as a critical and severe disease, it still can impact people's daily lives to different degrees. Those who have mild insomnia may experience fatigue, mood swings, and reduced work efficiency. Severe cases may have anxiety, depression,memory loss, lower immunity, physical discomfort, and even cerebral infarction or cerebral hemorrhage. These all place a heavy burden on patients and their families[13]. Stroke has a long recovery process, and it is often accompanied by psychological problems and varying degrees of insomnia[14]. The pathogenesis of post-stroke insomnia is not fully understood. At present,the mainstream theory holds that the direct destruction of or indirect influence on cerebrovascular areas that dominate or regulate sleep disturbs the sleep balance and leads to the occurrence of this disease[15]. These areas include the frontal lobe, orbital cortex, supraoptic nucleus, giant cell area of the midbrain, blue spot,interstitial nucleus, medullary reticular reticulum inhibitory area, and ascending reticular system. Sleep is related to the regulation of neurotransmitters.Norepinephrine (NE) is currently widely recognized as a neurotransmitter involved in arousal states. Studies have shown that 5-hydroxytryptamine (5-HT) and NE are directly or indirectly involved in the physiological regulation of sleep[16]. Deng JH, et al[17]found abnormal expression levels of serum cytokines and neurotransmitters in patients with post-stroke insomnia,especially the high expression of NE, indicating that the state of arousal was relatively prominent, which led to the occurrence of insomnia. At present, the drug treatment of this disease has different degrees of adverse reactions, resulting in poor compliance, and failure to obtain ideal clinical efficacy.
Post-stroke insomnia belongs to the category of ‘no sleep’, ‘can not sleep’, ‘can not lie down’, etc. in TCM.The disease location is mainly in the heart. The pathogenesis of post-stroke insomnia is excess yang and deficient yin and the non-interaction between yin and yang. The Governor Vessel-unblocking and mindregulating acupuncture method was used to regulate mind and balance yin and yang. This acupuncture method was developed according to the academic thought that ‘for the lesion in the brain, choose Governor Vessel acupoints’, put forward by Professor Zhang Dao-zong, a distinguished Chinese doctor. Baihui(GV 20), Shenting (GV 24), Yintang (GV 29), and Fengfu(GV 16) are Zhang Dao-zong’s main acupoints for stroke.This needling method mainly selects the points from the Governor Vessel, with standard needling technique and required depth, which is different from the traditional acupuncture method. In the meridian system of TCM, the Governor Vessel runs into the brain, and the brain is where all yang gathers. According to the treatment principle ‘an acupoint can treat the disorders where its meridian distributes’, Governor Vessel can help yin and yang interact, adjust the spirit and calm the mind[18]. Animal experiments have shown that acupuncture can reduce the glutamic acid (Glu) content in hypothalamus, and change the active state of nerve conduction by regulating the content of Glu, to control the occurrence and development of insomnia[19].Shenting (GV 24) is the place where the upgoing qi of the Governor Vessel gathers. Shenting (GV 24) is the crossing point of the Governor Vessel, Stomach Meridian and Bladder Meridian. Stimulation at Shenting(GV 24) can regulate qi and blood in the whole body, so as to unblock the Governor Vessel, regulate mind and balance yin and yang. Experiments have shown that electroacupuncture can significantly mitigate ischemia-reperfusion injury, so as to reduce the damage to brain tissues and nerves caused by ischemia, and thus improve the sleep of stroke patients[20]. Yintang(GV 29) is located between the two eyebrows and can tranquilize the mind, open orifices, calm the heart and enhance intelligence. Studies have proved that stimulation to Yintang (GV 29) can accelerate the neurotransmitter conduction to the pons, in which, the somniferous nerve centers such as the locus ceruleus and the mesenchymal nucleus, are projected on the body surface around the course of the Governor Vessel[21]. Fengfu (GV 16) is the crossing point of the Governor Vessel, Bladder Meridian, and Yang Link Vessel. Some scholars have found in ancient literature that the frequency of using Fengfu (GV 16) alone for brain diseases was up to 12.5%[22], which proved that Fengfu (GV 16) played an important role in the treatment of encephalopathy. Sishencong (EX-HN 1) are where yang gathers, located on the course of the Governor Vessel, and closely connected with the Bladder Meridian. Therefore, it can dredge qi in the whole body, with the effect of regulating and calming the mind, and harmonizing yin and yang, so that it can treat insomnia and other mental disorders[23]. Shenmen(HT 7), the Yuan-Primary point of the Heart Meridian, is where the heart qi passes and stays. It can nourish the heart, tranquilize the mind, and harmonize qi and blood.Sanyinjiao (SP 6) is the crossing point of the Liver Meridian, Spleen Meridian and Kidney Meridian. It can tonify the liver, fortify the spleen, and nourish the kidney. Insomnia is closely related to the liver, spleen and kidney, so Sanyinjiao (SP 6) is an important acupoint for treating insomnia[24]. Studies have proved that electroacupuncture at Sanyinjiao (SP 6) can regulate the diurnal activity of insomnia rats, improve the energy metabolism of the paraventricular nucleus of the hypothalamus of insomnia rats, and have a good adjustment effect on insomnia[25]. Shenmai (BL 62) and Zhaohai (KI 6) are the Confluence Points of the Eight Extraordinary Meridians, are connected with the Yin Heel Vessel and Yang Heel Vessel, respectively. Both Yin and Yang Heel Vessels are in charge of eyelid opening and closing, and thus directly related to sleep. In the meantime the Yin and Yang Heel Vessels are connected with the eyes and brain, so keeping the balance of Yin Heel Vessel and Yang Heel Vessel is key to having a good sleep[26]. Recent studies have shown that acupuncture at Shenmai (BL 62) and Zhaohai (KI 6) can significantly increase the contents of interleukin-1 (IL-1) and tumor necrosis factor (TNF) in the brain of rats, and it is better than the compatibility of other acupoints[27]. The aim of treating insomnia can be achieved by increasing the contents of gamma-aminobutyric acid (GABA) and 5-HT in the brain and reducing the NE content[28].
rTMS is based on the biological electromagnetic theory, through the pulsed magnetic field equipment to produce different frequencies on the central nervous system. It can sense and adjust local potential differences on both sides of the brain, induce hyperpolarization nerve cells, and then adjust the neural electrophysiological activity and tissue metabolism. It has been widely used in the treatment of insomnia[29-30]. Domestic scholars have reported that low-frequency rTMS can increase the release of inhibitory neurotransmitter GABA, slow down the speed of nerve signal transmission, inhibit the excitation of neurons, regulate the functional activities of the brainstem reticular structure, and thereby regulate sleep and wakefulness, and improve sleep quality[31-32].It has been reported that rTMS can effectively relieve the anxiety and depression of patients with sleep disorders and significantly improve bad mood[33].
Governor Vessel-unblocking and mind-regulating acupuncture method can benefit the mind and balance yin and yang. The main points are from the Governor Vessel, along with other acupoints, to balance yin and yang. rTMS is a popular modern rehabilitation technology. It is a non-invasive, safe, and simple operation, and can improve the metabolism of local brain tissues, regulate the expressions of neural factors in the brain, and thus promote the recovery of nerve function.
The results of this study showed that the PSQI, SAS and SDS scores of the two groups after treatment were lower than those before treatment. After treatment,compared with rTMS treatment alone, Governor Vessel-unblocking and mind-regulating acupuncture method combined with rTMS produced more significant efficacy in the treatment of post-stroke insomnia, by significantly improving the sleep quality and reducing patient’s anxiety and/or depression level. Therefore, the combination of unblocking Governor Vessel and regulating the mind and modern rehabilitation technology can produce a better outcome, and is worthy of further clinical research and application.
Conflict of Interest
The authors declare that there is no conflict of interest.
Acknowledgments
This work was supported by Mental Disorders Department Construction Project of Key Specialty During the 12th Five-year Plan Period of the State Administration of Traditional Chinese Medicine [国家中医药管理局“十二五”重点专科神志病科建设项目,No. (2012)2];Provincial Key Specialty (Disease) Construction Project of Traditional Chinese Medicine During the 13th Five-year Plan Period of Anhui Province [安徽省“十三五”省级中医重点专科(病)建设项目,No. (2017)567].
Statement of Informed Consent
Informed consent was obtained from all individual participants.
Received: 1 July 2019/Accepted: 15 August 2019
 Journal of Acupuncture and Tuina Science2020年2期
Journal of Acupuncture and Tuina Science2020年2期
- Journal of Acupuncture and Tuina Science的其它文章
- Clinical efficacy of acupuncture in treatment of chronic urticaria and its effects on the content of IgE and the imbalance of Th1/Th2 cell function
- Therapeutic observation of ‘warming-unblocking needling technique’ for knee osteoarthritis due to deficiency of liver and kidney
- Therapeutic observation of arthrolysis under brachial plexus anesthesia for adhesive capsulitis of the shoulder
- Clinical study of thumb-tack needle therapy for cervical radiculopathy based on meridian differentiation
- Clinical observation on prevention of chemotherapy infection in gastric cancer by moxa-stick moxibustion plus rhG-CSF and its effect on immune function
- Clinical observation of deep electroacupuncture at Baliao points for female stress urinary incontinence
