Prolonged prothrombin time at admission predicts poor clinical outcome in COVID-19 patients
Lang Wang,Wen-Bo He,Xiao-Mei Yu,Da-Long Hu,Hong Jiang
Lang Wang,Wen-Bo He,Xiao-Mei Yu,Hong Jiang,Department of Cardiology,Renmin Hospital of Wuhan University,Wuhan 430060,Hubei Province,China
Lang Wang,Wen-Bo He,Xiao-Mei Yu,Hong Jiang,Cardiovascular Research Institute,Wuhan University,Wuhan 430060,Hubei Province,China
Lang Wang,Wen-Bo He,Xiao-Mei Yu,Hong Jiang,Hubei Key Laboratory of Cardiology,Wuhan 430060,Hubei Province,China
Da-Long Hu,School of Biotechnology and Biomolecular Sciences,The University of New South Wales,Sydney 2052,Australia
Abstract BACKGROUND The prognostic value of coagulation disorder in coronavirus disease 2019(COVID-19)patients should be demonstrated.AIM To investigate the abnormalities of coagulation parameters in the patients with COVID-19 and their prognostic values.METHODS Consecutive patients admitted in the isolation ward of Renmin Hospital of Wuhan University from January 31 to February 5,2020 with confirmed COVID-19 were included.The primary outcomes were death and survival as of March 11.Demographics,vital signs,comorbidities and laboratory tests were collected and compared between those who died and survivors.Logistic regression analysis for prognostic factors was performed.Kaplan-Meier analysis was used to compare the estimated survival rate between patients with prolonged prothrombin time and normal prothrombin time.RESULTS The total number of patients with confirmed COVID-19 who were enrolled was 213.The median age was 62 years,and 95 patients(44.6%)were men.Fifty-one patients were critical(23.9%),79 patients were severe(37.1%)and 83 patients were moderate(39%).As of March 11,2020,99 patients were discharged(46.5%),79 patients(37.1%)stayed in the hospital and 35 patients(16.2%)died.Median time to death was 6(4-8)d,while median hospital stay was 32(22-36)d in survivors(P<0.001).More men(P = 0.002)and elderly patients(P <0.001)were found in the group of those who died.The respiration rate at admission was higher in the group of those who died(P <0.001).The incidences of hypertension(P = 0.028),cerebrovascular disease(P <0.001),chronic kidney disease(P = 0.02)and chronic obstructive pulmonary disease(P <0.001)were higher in the group of those who died.Platelet count was decreased in the group of those who died(P = 0.002)whereas prothrombin time(P <0.001),activated partial thromboplastin time(P =0.033),concentration of D-dimer(P <0.001)and fibrin degradation products(P <0.001)were increased in the group of those who died.Prothrombin time[odds ratio(OR):2.19,P = 0.004],respiration rate(OR:1.223,P <0.001),age(OR:1.074,P<0.001)and fibrin degradation products concentration(OR:1.02,P = 0.014)were predictors of death.The survival rate was significantly lower in patients with prolonged prothrombin time compare to those with normal prothrombin time(P<0.001).CONCLUSION Prothrombin time,concentration of fibrin degradation products,respiration rate and age were predictive factors for clinical outcomes of COVID-19 patients.
Key Words:COVID-19;Coagulation;Prothrombin time;Fibrin degradation products;Prognosis;Infectious disease
INTRODUCTION
Coronavirus disease 2019(COVID-19)is caused by severe acute respiratory syndrome coronavirus 2(SARS-CoV-2)infection.Since the first COVID-19 case was diagnosed in December 2019,the SARS-CoV-2 has been spreading rapidly around the world.As of March 19,it has caused 209839 infection cases including 8778 deaths[1].According to the preliminary statistics from the Chinese Center for Disease Control and Prevention,nearly 20% of the patients were severe to critical,and the case-facility rate of which was much higher than the whole patient population[2].The disease progressed extremely fast in some severe to critical patients.Thus,early identification of COVID-19 patients at high risk is important for improving the clinical practice and outcomes.
Coagulation disorder has been reported in COVID-19 patients in several descriptive studies[3-5].The elevation of D-dimer and fibrin degradation products(FDP),shortened or prolonged prothrombin time(PT),abnormal platelet count,occurrence of thrombosis or bleeding and complication of disseminated intravascular coagulation(DIC)were observed in COVID-19 patients in different clinical stages[6,7].These findings indicate that the coagulation disorder played an important role in the clinical process of COVID-19.Coagulation disorder at the end-stage of COVID-19 or after invasive treatment is common and reasonable but with limited prognostic value.The coagulation function at the early stage of hospitalization should be paid more attention to,which may help the doctors to identify patients at high risk and guide the clinical strategy.
MATERIALS AND METHODS
Study design and participants
This is a retrospective,single-center study.Confirmed COVID-19 cases admitted from January 31 to February 5,2020 to Renmin Hospital of Wuhan University were enrolled in this study.The patients with recent trauma,anticoagulation treatment,confirmed thrombosis or bleeding before hospitalization were excluded.The diagnosis of COVID-19 was based on the interim guidance for novel coronavirus pneumonia published by the National Health Commission of the People’s Republic of China[8].Patients with COVID-19 were divided into mild,moderate and severe according to the report of the World Health Organization-China joint mission on COVID-19[9].Laboratory confirmed cases without pneumonia were classified as mild,laboratory confirmed cases with pneumonia were classified as moderate,patients with dyspnea,respiratory frequency ≥ 30/min,blood oxygen saturation ≤ 93%,PaO2/FiO2ratio <300,and/or lung infiltrates in >50% of the lung field within 24-48 h were classified as severe.The patients with respiratory failure requiring mechanical ventilation,shock or other organ failure that required intensive care were classified as critical.This study(WDRY2020-K032)was approved by the Ethics Committee of Renmin Hospital of Wuhan University.
Procedures
Specific nucleic acid of SARS-CoV-2 was detected using real-time polymerase chain reaction to confirm viral infection.Chest X-ray and/or computed tomography were performed for the COVID-19 diagnosis.The patients’ medical records were reviewed by trained physicians.Demographics,vital signs,comorbidities,laboratory results of platelet count and coagulation function were collected.All the vital signs were achieved at admission.Comorbidities including hypertension,diabetes,cardiovascular disease,cerebrovascular disease,chronic kidney disease,chronic obstructive pulmonary disease(COPD),malignancy and autoimmune diseases were collected from patient history.All the blood samples for laboratory tests were collected within 24 h after admission.Platelet count was determined using the Sysmex XN-9000(Japan),an automated hematology analyzer.The PT,activated partial thromboplastin time(APTT)and thrombin time(TT)were determined by the clot formation technique.The concentration of fibrin,FDP and D-dimer were quantified by the nephelometric analysis.All the coagulation tests were performed using a Sysmex CS5100 automatic coagulation analyzer(Japan)and proprietary reagents.The normal ranges of the laboratory findings were according to the test manual and reagent description of Renmin Hospital of Wuhan University.
Statistical analysis
Basic statistical analyses were performed using Statistic Package for Social Science version 26.0(Chicago,IL,United States).The normality of continuous variables was tested using the Kolmogorov-Smirnov test.Hypothesis testing was performed for comparing continuous and categorical variables in different outcome groups using the Mann-WhitneyUtest and chi-squared test,respectively.The comorbidities,clinical and laboratory variables that differed significantly based on comparative statistics were included in univariate and multivariate analysis.Variables with statistical significance in the univariate logistic regression were included in the multivariate analysis using forward stepwise logistic regression.The survival rates were analyzed using Kaplan-Meier analysis.All significance levels were computed for two-tailed testing and the cutoff of significance was set atP<0.05 and high significance atP<0.001.
RESULTS
Outcomes
The clinical outcomes were survival and death as of March 11,i.e.5 wk after the last admission.According to the interim guidance for novel coronavirus pneumonia published by the National Health Commission of the People’s Republic of China[8],patients were discharged when their symptoms improved significantly,with no fever for at least 3 d,obvious absorption of inflammation on pulmonary imaging and negative results for at least two consecutive SARS-CoV-2 nucleic acid tests with an interval of more than 24 h.Patients who did not meet the discharge standard stayed at the hospital for treatment.The discharged patients and those who stayed in the hospital until the end date of follow-up were grouped in the survival group.
Demographics and baseline clinical characteristics
Of 213 patients enrolled,the median age was 62 years,and 95 were men(44.6%).As presented in Table 1,61% of the enrolled patients were classified as severe or critical.All the patients who died were critically ill.By Mar 11,2020,99 patients were discharged(46.5%),79 patients(37.1%)stayed in the hospital and 35 patients(16.2%)died.There were more males and elderly patients in the group of those who died.Compared with the survivors,comorbidities including hypertension,cerebrovascular disease,chronic kidney disease and COPD were more prevalent in the group of those who died.Vital signs at admission including heart rate,systolic blood pressure,diastolic blood pressure and respiration rate were compared between groups.The respiration rate was significantly higher in those who died.
The onset-to-admission time was compared between the survivors and those who died,and no significant difference was found.The length of hospital stay was also analyzed.For the patients who continued hospitalization until the end date of followup,the length of stay was defined as the duration from admission to the end date of follow-up.The length of hospital stay in survivors was 32(22-36)d,while the admission-to-death time was only 6(4-8)d for those who died.
Laboratory findings
Platelet count and coagulation parameters were analyzed in the present study.Of the included 213 patients,thrombocytopenia was found in 26(12.2%),and thrombocytosis was found in 10(4.7%).PT was prolonged in 39 patients(18.8%).Activated APTT was shortened in 27 patients(12.7%)and was prolonged in 56 patients(26.3%).Eight patients(3.8%)were found with prolonged TT.The shortening of PT or TT was not observed in the present study.The fibrinogen levels in 9 patients(4.7%)were below the normal range and were elevated in 105 patients(49.3%).The concentrations of Ddimer were increased in 123 patients(57.7%),and the concentrations of FDP were elevated in 66 patients(31%).
Comparison of platelet count,coagulation function parameters and the incidence of abnormalities in coagulation indices between survivors and those who died are shown in Table 2.The platelet count was significantly lower in those who died,whereas PT,APTT and the concentrations of D-dimer and FDP were all significantly higher in those who died.There were significant differences in the incidences of thrombocytopenia,PT prolongation,APTT prolongation,TT prolongation,fibrinogen reduction,D-dimer elevation and FDP elevation between those who survived and those who died.
Univariate and multivariate analysis for the prognostic factors
Univariate and multivariate logistic regressions were used to analyze the risk factors for fatal outcome(Table 3).The factors with significant differences between the death and survival groups,including age,sex,comorbidities,respiration rate,platelet count,PT,APTT,D-dimer and FDP,were included in the regression.Univariate analysis showed that age,sex,hypertension,cerebrovascular disease,chronic kidney disease,COPD,respiration rate,PT,concentrations of D-dimer and FDP may contribute to the death risk of COVID-19 patients.Then those factors with statistical significance in the univariate regression were taken for the multivariate analysis using forward stepwise logistic regression,in which PT[odds ratio(OR):2.19,95% confidence interval(CI):1.285-3.733,P= 0.004],respiration rate(OR:1.223,95%CI:1.095-1.366,P= 0.001),age(OR:1.074,95%CI:1.034-1.115,P= 0.001)and FDP concentration(OR:1.02,95%CI:1.004-1.037,P= 0.014)remained to be the significant predictors for death in the multivariate logistic model.
Survival curves in patients with prolonged PT and normal PT
The survival curves of patients with prolonged PT and normal PT were plotted,and the survival rates were analyzed using Kaplan-Meier analysis(Figure 1).The survival rate at day 5 of hospitalization in normal PT group and prolonged PT group were estimated at 95.8% ± 1.6% and 76.9% ± 6.7%,respectively.The survival rate at day 11 in normal PT group and prolonged PT group were estimated at 90.4% ± 2.3% and 64.1% ± 7.7%,respectively.According to the result of Log-rank,Breslow and Tarone-Ware tests,the survival curves of the two groups have a highly significant difference(P= 0.001).
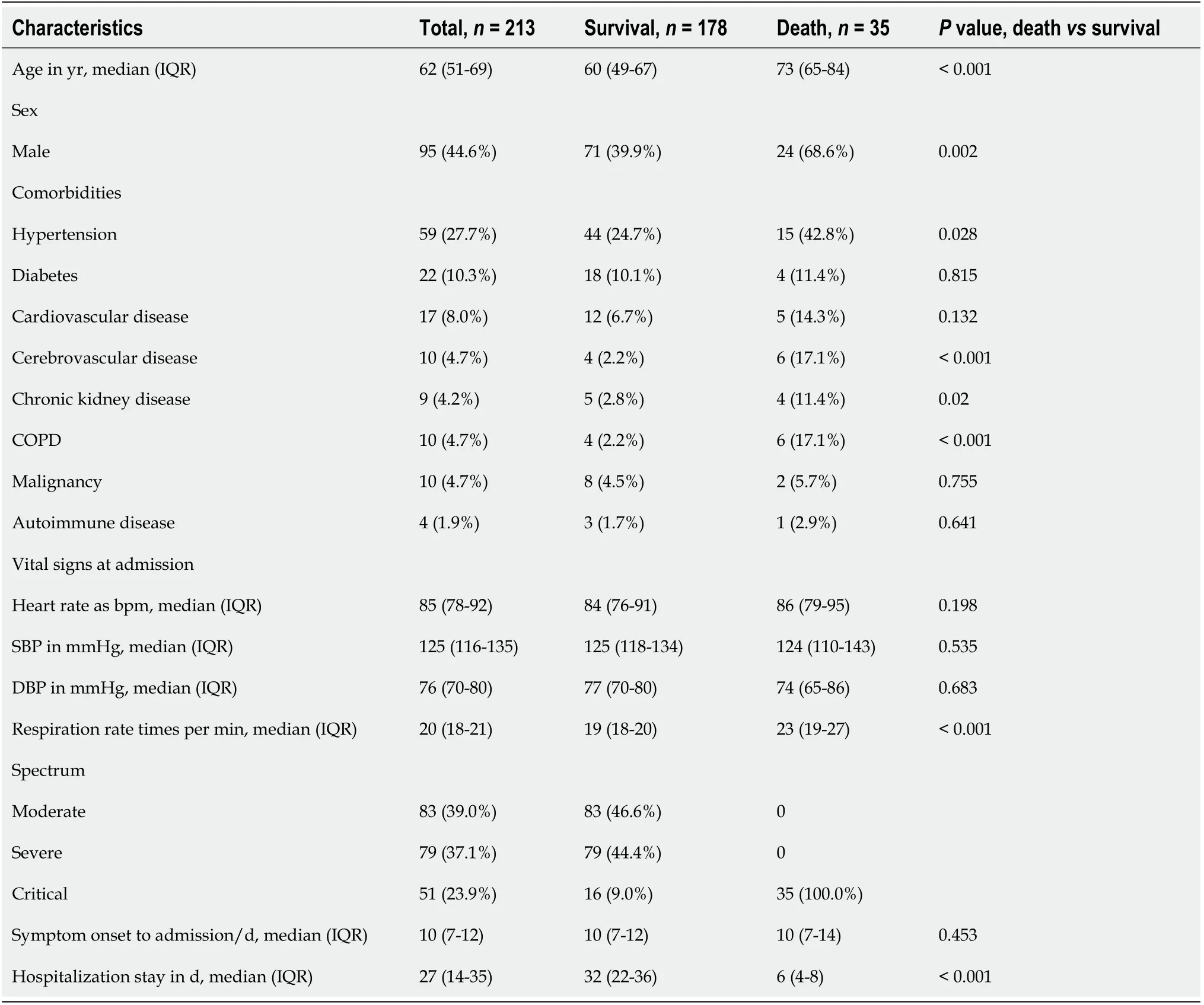
Table 1 Baseline characteristics of patients enrolled
DISCUSSION
In the present study,we investigated the prognostic value of coagulation parameters in patients with COVID-19 based on at least 5 wk of follow-up.Prolonged PT at admission was found to be a strong predictor for a poor outcome in COVID-19 patients as well as age,respiration rate and FDP concentration,which were also found to contribute to the risk of death in COVID-19 patients.
Renmin Hospital of Wuhan University is a designated hospital for severe COVID-19 patients.In the present study,35 of 213 patients had died by the 5 wk follow-up,and the CRF was 16.4%,which was higher than the whole patient population.Up to 61% of the enrolled patients were severe to critical,which might contribute to the higher fatality rate.The median survival time for those who died was 6 d,indicating that the disease progressed rapidly in some critical patients.Elderly age and more males were more commonly found in the group of those who died,which was consistent with previous reports[2].Comorbidities including hypertension,cerebrovascular disease,chronic kidney disease and COPD,which are more common in the elderly people,were more prevalent in the group of those who died in the present study.The medianheart rate and blood pressure at admission were all in the normal range both in survivors and those who died,indicating the vital signs of most patients were stable at admission.The respiration rate was significantly higher in those who died.The increased respiration rate might reflect the severity of lung lesions and hypoxic conditions in COVID-19 patients.
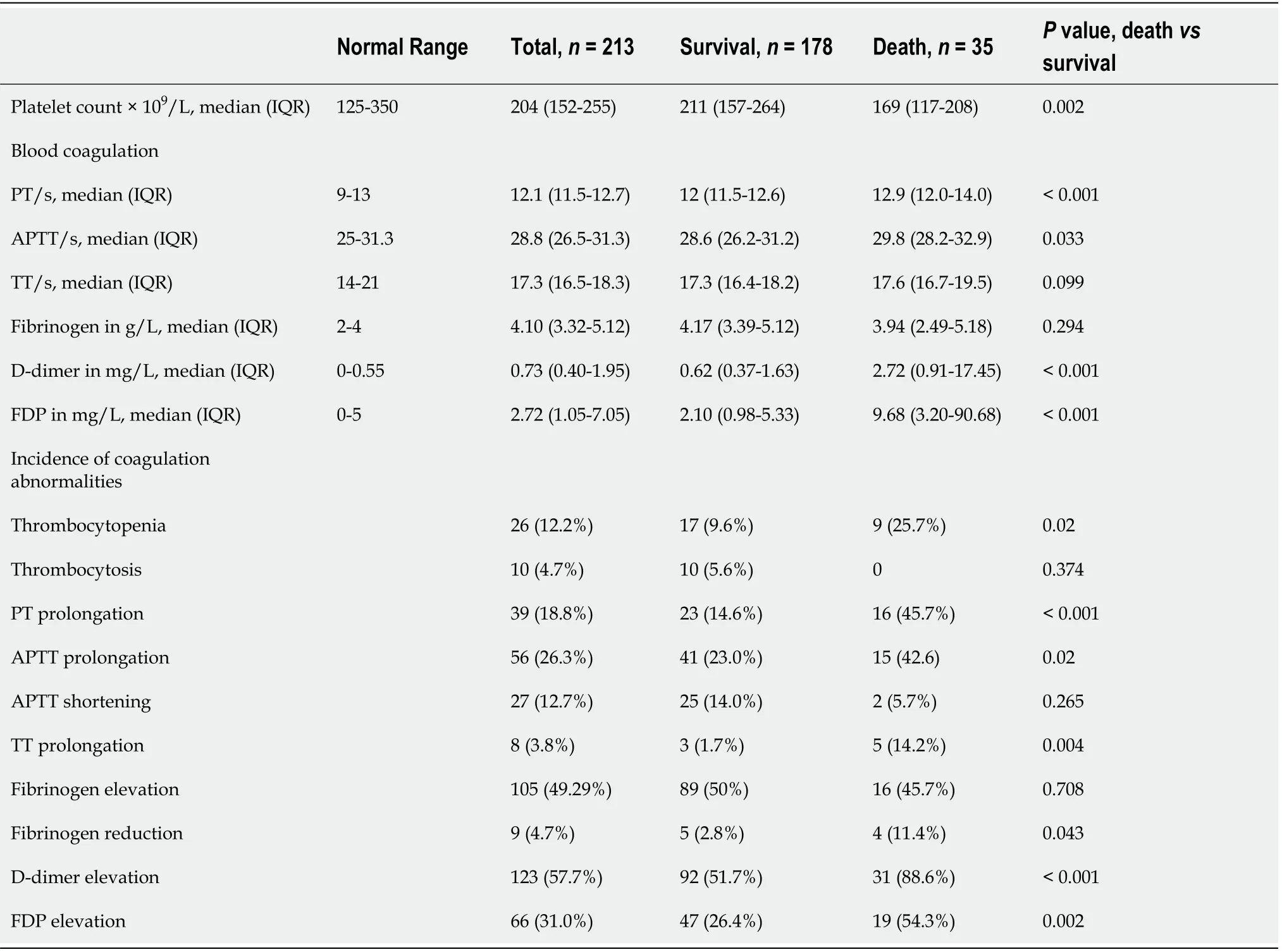
Table 2 Laboratory findings at admission
Coagulation disorder has been reported in various viral infections including SARSCoV,MERS-CoV and influenza virus infection[10-14].All aspects of the coagulation cascade,primary hemostasis and fibrinolysis could be affected.The coagulation parameters not only reflect the hemostasis but also associate with the inflammation and organ dysfunction[15].In the present study,the comparison of laboratory findings between those who died and survivors showed a significant difference in platelet count and coagulation parameters.Both thrombocytopenia and thrombocytosis were found in COVID-19 patients.However,platelet count in those who died was significantly lower than that in the survivors.The incidence of thrombocytopenia was correspondingly higher in those who died.Similar findings in platelet count had been reported in SARS-CoV infection[16].Consumption associated with thrombin-mediated platelet activation and adhesion to endothelial cells and leucocytes could contribute to the reduction of circulating platelets in the critically ill patients[17].
No patients showed shortened PT,whereas prolonged PT was found in 18.8% of the patients in the present study.The PT and APTT were significantly longer in those who died,but there was no difference with TT.The incidences of PT and APTT prolongation were also increased in those who died.PT and APTT evaluate the integrity of the extrinsic and intrinsic pathways of coagulation,respectively,while both PT and APTT are affected by the final common pathway[18,19].The prolonged PT and APTT in those who died might indicate the activation of coagulation and the consumption of coagulation factors.
Elevation of D-dimer and FDP were found in 57.7% and 31% of the COVID-19patients,respectively,which was consistent with previous reports[3,6].The median concentrations of D-dimer and FDP were significantly increased in those who died compared with survivors.D-dimer and FDP both originate from the degradation of fibrin and are manifestations for thrombosis and the activation of the fibrinolysis system.Elevation of D-dimer was also associated with severe infection[15,20].The raised D-dimer and FDP concentrations implicate thrombophilia and system inflammation in those COVID-19 patients.
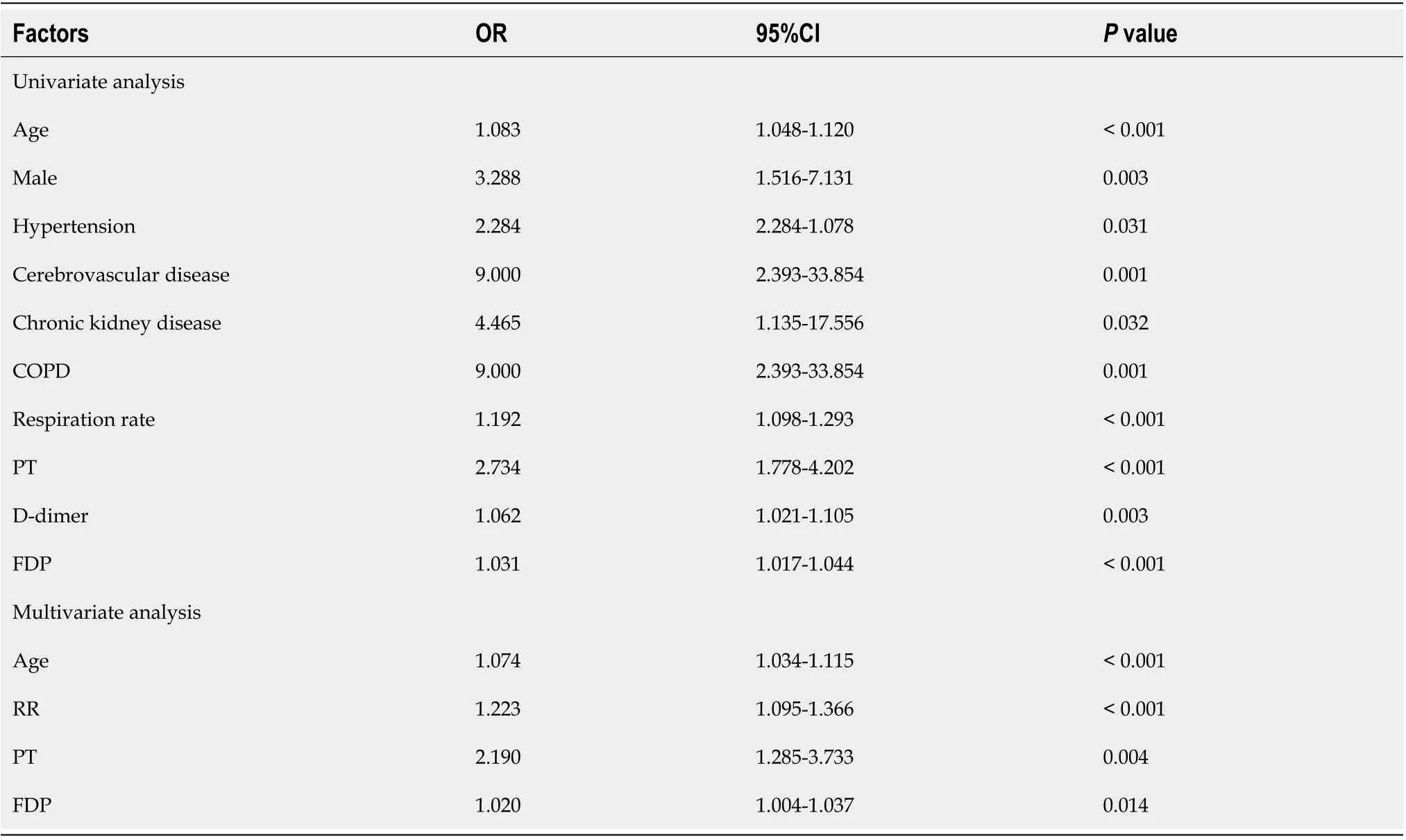
Table 3 Univariate and multivariate logistic regression for prognosis factors
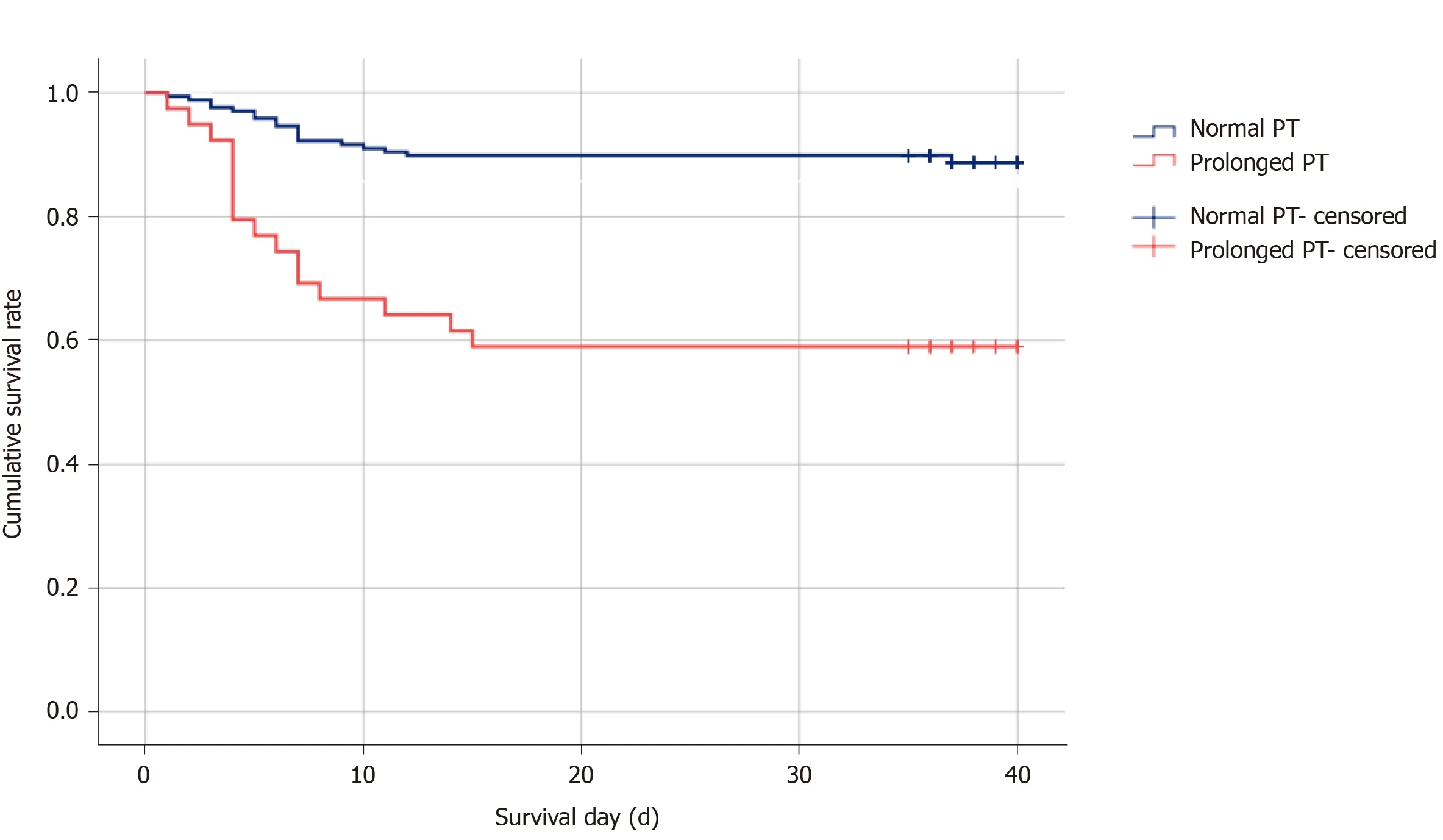
Figure 1 Survival curves of patients with prolonged prothrombin time and normal prothrombin time.The survival curves of patients with prolonged prothrombin time and normal prothrombin time were analyzed using Kaplan-Meier analysis.Log-rank,Breslow and Tarone-Ware tests showed the survival curves of the two groups had a highly significant difference(P <0.001).PT:Prothrombin time.
As the platelet count and several parameters of coagulation were significantly different between those who died and survivors,the prognostic value of these factors for COVID-19 was analyzed using logistic regression.PT,concentrations of D-dimer and FDP,age and respiration rate were found to contribute to the fatal outcome in COVID-19 patients.Multivariate analysis showed that PT was a strong prognostic factor with an odds ratio of 2.190 in the COVID-19 patients.FDP concentration was also predictive for the clinical outcomes of COVID-19 patients;however,the prognostic value was limited as the odds ratio was around 1.Age and respiration rate were also found to be prognostic factors in the multivariate analysis,which probably reflect the baseline state and the degree of hypoxia.To further illustrate the impact of PT prolongation on the fatality,the patients were divided into prolonged PT group and normal PT group.Then the survival curve was plotted and analyzed using Kaplan-Meier analysis.The prolonged PT group showed significantly lower estimated survival rate at day 5 of hospitalization,at day 11 of hospitalization and at the end date of follow-up.These data demonstrated that prolonged PT at admission could be a warning sign for high risk of death in the COVID-19 patients.
Tanget al[21]reported the abnormal coagulation in COVID-19 patients.In their study,the comparison of coagulation parameters in survivors and those who died was based on a 10-d to 12-d observation.Significant anomalies of coagulation parameters were observed in those who died,and the development of DIC was more frequent in those who died.DIC is a serious abnormality of coagulation function that usually occurs at the late stage of infectious diseases.In our present study,there were only two patients with DIC(≥ 5 points)[22]at admission(data not shown).The occurrence of DIC reflects the severity of disease.However,it may not have great predictive value.
In our present study,coagulation parameters at admission were analyzed using multivariate logistic regression,which showed PT is a strong prognosis factors of COVID-19.The PT is a measure of the integrity of the extrinsic and final common pathways of the coagulation cascade that consists of tissue factor and factors VII,II,V,X and fibrinogen.The elevation of PT/international normalized ratio in infectious disease is usually accompanied with low factor levels of VII,IX and X.This is associated with bleeding risk and relates to thrombosis in the patients with infectious disease[23].PT could be a relatively early and sensitive indicator for systematic coagulation dysfunction in infectious disease.Our study underscores the need for early detection of coagulation function,which is especially important for risk assessment in COVID-19 patients.
CONCLUSION
Coagulation disorders were significantly more common in the patients who died with COVID-19 than the survivors.Prothrombin time,concentration of fibrin degradation products,respiration rate and age were predictive factors for clinical outcomes of COVID-19 patients.Patients with prolonged prothrombin time at admission should be treated with caution as they were faced with much higher risk of death.
ARTICLE HIGHLIGHTS
Research background
Coronavirus disease 2019(COVID-19)has been spreading rapidly around the world.The disease progressed extremely fast in some severe to critical patients.
Research motivation
Early identification of COVID-19 patients at high risk is important for improving the clinical practice and outcomes.
Research objectives
To investigate the abnormalities of coagulation parameters in the patients with COVID-19 and their prognostic values.
Research methods
A retrospective,single-center study included 213 patients.The coagulation parameters at admission were compared between the survivors and those who died.The prognostic values of coagulation disorders were analyzed with logistic regression.
Research results
Coagulation disorders were significantly more common in the patients who died with COVID-19 than the survivors.Prothrombin time(PT),concentration of fibrin degradation products,respiration rate and age were predictive factors for fatal outcomes.The fatality of patients with prolonged PT at admission was significantly higher than those with normal PT.
Research conclusions
Patients with prolonged PT at admission were faced with a much higher risk of death.Thus,clinicians should be aware of this and treat these patients with caution.
Research perspectives
Patients with prolonged prothrombin time at admission should be treated with caution as they faced a much higher risk of death.Coagulation disorders were significantly more common in the patients who died with COVID-19.
 World Journal of Clinical Cases2020年19期
World Journal of Clinical Cases2020年19期
- World Journal of Clinical Cases的其它文章
- Role of monoclonal antibody drugs in the treatment of COVID-19
- Review of simulation model for education of point-of-care ultrasound using easy-to-make tools
- Liver injury in COVID-19:A minireview
- Transanal minimally invasive surgery vs endoscopic mucosal resection for rectal benign tumors and rectal carcinoids:A retrospective analysis
- Impact of mTOR gene polymorphisms and gene-tea interaction on susceptibility to tuberculosis
- Establishment and validation of a nomogram to predict the risk of ovarian metastasis in gastric cancer:Based on a large cohort
