Early renal injury indicators can help evaluate renal injury in patients with chronic hepatitis B with long-term nucleos(t)ide therapy
Tong-Tong Ji, Ning Tan, Hai-Ying Lu, Xiao-Yuan Xu, Yan-Yan Yu
Tong-Tong Ji, Ning Tan, Hai-Ying Lu, Xiao-Yuan Xu, Yan-Yan Yu, Department of Infectious Diseases, Peking University First Hospital, Beijing 100034, China
Abstract BACKGROUND Patients with chronic hepatitis B (CHB) with long-term nucleos(t)ide therapy may experience renal insufficiency. Traditional renal function indicators, such as urine protein, serum urea nitrogen (BUN), and serum creatinine, are normal when early mild lesions occur. Therefore, more sensitive renal function indicators are needed.AIM To investigate the significance of early renal injury indicators in evaluating renal injury in patients with CHB with long-term nucleos(t)ide therapy.METHODS We collected the clinical data of 69 outpatients with CHB at Peking University First Hospital from March 2018 to January 2020 who had been treated with longterm nucleos(t)ide therapy and analyzed the results of early renal injury indicators. Continuous normal distribution data were analyzed by the t-test to determine the difference between two groups. Continuous non-normally distributed data were analyzed by the Mann-Whitney U-test between two groups.The Kruskal-Wallis H test was used to determine the differences among multiple groups. Enumeration data were analyzed by the chi-square test. The related factors of early renal injury indicators were analyzed by logistic regression analysis.RESULTS The average treatment duration with nucleos(t)ide analogs of the 69 patients with CHB was 99.7 ± 28.7 mo. The cases of patients with elevated BUN and hypophosphatemia were 6 (8.7%) and 13 (18.8%), respectively; 31 (44.9%) patients had abnormal early renal injury indicators, including 9 patients with abnormal urine microalbumin, 7 patients with abnormal urine immunoglobulin, 6 patients with abnormal urine transferrin, and 19 patients with abnormal α1 microglobulin.There were no significant differences in the mean values of age, sex, BUN,estimated glomerular filtration rate (eGFR), serum uric acid, serum calcium, or serum phosphorus between the two groups of patients with and without early renal injury indicators. However, the mean levels of serum creatinine and urine creatinine, N-acetyl-β-D-glucosidase enzyme, α1 microglobulin, and urine immunoglobulin in the former group of patients were significantly higher than those in the latter group of patients (P < 0.05). The incidence of early renal injury in patients with eGFR ≥ 90, 60-89, and 30-59 mL/(min·1.73 m2) was 36.4% (8/22),47.6% (20/42), and 60% (3/5), respectively. Logistic regression analysis results showed that gamma-glutamyl transpeptidase [odds ratio (OR) = 1.05 (1.008-1.093), P = 0.020], direct bilirubin [OR = 1.548 (1.111-2.159), P = 0.010], serum creatinine [OR = 1.079 (1.022-1.139), P = 0.006], and age [OR = 0.981 (0.942-1.022),P = 0.357] were independent predictors of early renal injury.CONCLUSION Patients with CHB treated with long-term nucleos(t)ide analog therapy had a high probability of early renal injury, and early renal injury indicators were highly sensitive and could be used to monitor early renal impairment.
Key Words: Early renal injury; Chronic hepatitis B; Nucleos(t)ide analog; N-acetyl-β-Dglucosidase enzyme; α1 microglobulin; Urine immunoglobulin
INTRODUCTION
Nucleos(t)ide analogs (NAs), including lamivudine (LAM), adefovir dipivoxil (ADV),telbivudine (LdT), entecavir (ETV)[1,2], tenofovir disoproxil fumarate (TDF)[3,4], and tenofovir alafenamide fumarate (TAF)[5-7], are important antiviral drugs for patients with chronic hepatitis B (CHB). Patients with CHB need to have their renal function monitored regularly during treatment because long-term antiviral therapy can cause renal injury. Early renal injury indicators can detect early mild renal lesions, which is helpful in the early detection, early diagnosis, and early treatment of renal dysfunction. In this article, we retrospectively analyzed the clinical data of patients with CHB who received long-term NA therapy in the outpatient Department of Liver Disease of Peking University First Hospital. We mainly observed and discussed the clinical value and significance of early renal injury indicators in the evaluation of renal injury in patients with CHB with long-term NA therapy.
MATERIALS AND METHODS
Subjects
In this article, we retrospectively analyzed the clinical data of 69 patients with CHB who had received long-term NAs in the outpatient Department of Liver Disease of Peking University First Hospital from March 2018 to January 2020, including 48 males(69.6%) with an average age of 54.1 ± 12.0-years-old and 21 females (30.4%) with an average age of 57.6 ± 9.2-years-old. The diagnostic criteria refer to the “Guidelines for the Prevention and Treatment of Chronic Hepatitis B”[8]of China. The exclusion criteria included antiviral treatment course < 2 years; patients with chronic liver disease caused by non-hepatitis B virus (HBV) or chronic HBV infection with other liver diseases; patients with other chronic kidney diseases; and patients with diabetes mellitus. The study protocol was approved by the Ethics Committee of Peking University First Hospital in 2018 (Research No. 264), and all patients signed informed consent forms.
Research methods
The clinical data of patients were collected, including age, sex, type of antiviral drugs,treatment time, liver function, HBV deoxyribonucleic acid (DNA), serum urea nitrogen(BUN, normal value: 1.8-7.1 μmol/L), creatinine (normal value: 44-133 μmol/L), uric acid (normal value: 150-420 μmol/L), serum calcium (normal value: 2.12-2.75 mmol/L), serum phosphorus (normal value: 0.96-1.62 mmol/L), serum magnesium(normal values: 0.8-1.2 mmol/L), estimated glomerular filtration rate [eGFR,mL/(min·1.73 m2)], and early renal injury indicators such as urine creatinine(mmol/L), urine microalbumin (normal value: 0-19 mg/L), urine transferrin (normal value: 0-2 mg/L), urine α1-microglobulin (normal value: 0-12 mg/L), urine immunoglobulin (normal value: < 8 mg/L), and N-acetyl-β-D-glucosidase (NAG)enzyme (normal value: 0.3-12 U/L). As long as one of the early renal injury indicators was abnormal, it was defined as early renal damage. Serum creatinine was measured by the picric acid rate method (Zhongsheng Beikong Company’s kit; Hitachi 7600 automatic biochemical analyzer). The detection methods of early renal function indicators were as follows: Urinary creatinine was measured by the picric acid method(Zhongsheng Beikong Biotechnology, Beijing, China); urine microalbumin, urine transferrin, urine α1-microglobulin, and urine immunoglobulin were determined by immune scatter turbidity (Beckman Coulter, Brea, CA, United States); and NAG enzyme was determined by the MNP-G1CNAc substrate method (Gcell Kit; Beijing Jiuqiang Biological Company, Beijing, China). HBV DNA was detected by the Da'an Real-Time Fluorescence polymerase chain reaction HBV DNA Quantitative Detection Kit of Sun Yat-sen University, and the lower limit of detection value was 100 IU/mL.
Statistical analysis
Statistical analyses were performed using SPSS 25.0 software (Armonk, NY, United States). The measurement data were expressed as (mean ± standard deviation) or the median, and continuous normally distributed data were analyzed byt-test to determine the difference between two groups. Continuous non-normally distributed data were analyzed by the Mann-WhitneyU-test between two groups. The Kruskal-Wallis H test was used to determine the differences among multiple groups.Enumeration data were analyzed by the chi-square test. The related factors of early renal injury indicators were analyzed by logistic regression analysis, andP< 0.05 was considered statistically significant.
RESULTS
Antiviral therapy efficacy
A total of 69 patients with CHB were enrolled in this study, including 48 males (69.6%)and 21 females (30.4%). Among them, one patient received LAM, 7 patients received ADV, 41 patients received ETV, 14 patients received ADV + ETV, one patient received LdT, 4 patients received TDF, and one patient received TAF. The average antiviral treatment duration was 99.7 ± 28.7 mo. All patients with CHB had stable situations,and most of them had normal liver function with an undetectable HBV DNA level(specific values were omitted).
Influence of different antiviral drugs on renal function
The serum creatinine level of 69 patients was in the normal range. Six patients (8.7%)had an increase in BUN levels, and 13 patients had hypophosphatemia (18.8%). There was no significant abnormality in the routine urine test of all patients. Patients in the ADV/TDF treatment group had a higher percentage of increased BUN, early renal injury, and hypophosphatemia than the patients in the non-ADV/TDF treatment group, but the differences between the two groups were not statistically significant (P> 0.05). Specific data are shown in Table 1. Hypermagnesemia occurred in 4 patients and 6 patients in the ADV/TDF and non-ADV/TDF treatment groups, respectively,and hypercalcemia occurred in 1 patient and 2 patients, respectively. Elevated serumcreatinine levels and hypocalcemia were not found in all patients.
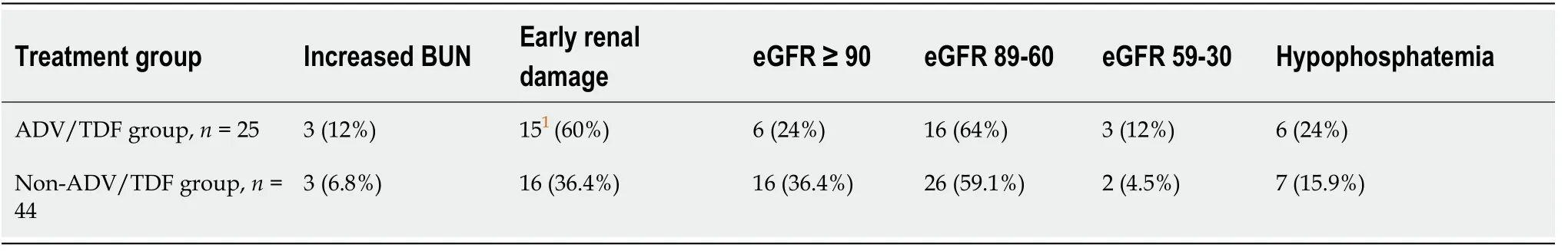
Table 1 Renal function test results of patients with and without adefovir dipivoxil / tenofovir disoproxil fumarate treatment
Impact of antiviral therapy on the eGFR
According to the eGFR value, 69 patients with CHB were divided into the following three groups: (1) EGFR ≥ 90 mL/(min·1.73 m2) group; (2) EGFR = 60-89 mL/(min·1.73 m2) group; and (3) EGFR = 30-59 mL/(min·1.73 m2) group. The number of patients in the three groups was 22 (31.9%), 42 (60.9%), and 5 (7.2%), respectively. There was no significant difference in sex, the mean value of liver function, serum uric acid, serum calcium, or serum magnesium among the three groups (P> 0.05, specific data omitted). Differences in age, serum creatinine, and the duration of antiviral treatment among the three groups were statistically significant (P< 0.05). The serum levels of urea nitrogen and phosphorus in the third group of patients were significantly different from those in the first group and the second group of patients (P< 0.05). With the decrease in eGFR value, the percentage of patients with hypophosphatemia or early renal injury increased, but the difference among the three groups was not statistically significant (P> 0.05). The specific figures are shown in Table 2.
Impact of antiviral therapy on early renal injury indicators
A total of 31 (44.9%) of 69 patients had abnormal early renal injury indicators, which were considered early renal damage, including 9 patients with abnormal urine microalbumin, 6 patients with abnormal urine transferrin, 14 patients with abnormal NAG enzyme, 19 patients with abnormal α1 microglobulin, and 7 patients with abnormal urinary immunoglobulin. There were no significant differences in the mean values of age, sex, alanine aminotransferase, aspartate aminotransferase,microalbumin, alkaline phosphatase, total bilirubin, BUN, eGFR, serum uric acid,serum calcium, serum phosphorus, and serum magnesium in patients with or without early renal injury (P> 0.05). However, the differences in gamma-glutamyl transpeptidase (GGT), direct bilirubin (DBIL), and serum creatinine levels, as well as urine creatinine, NAG enzyme, α1 microglobulin, and urine immunoglobulin levels were statistically significant between the two groups of patients (P< 0.05). Patients with early renal injury had a greater percentage of eGFR < 70 mL/(min·1.73 m2) than patients without early renal injury, but the difference was not statistically significant (P> 0.05). The specific figures are shown in Table 3.
Results of logistic regression analysis
The results of logistic regression analysis showed that GGT [odds ratio (OR) = 1.05(1.008-1.093),P= 0.020], DBIL [OR = 1.548 (1.111-2.159),P= 0.010], blood creatinine[OR = 1.079 (1.022-1.139),P= 0.006], and age [OR = 0.981 (0.942-1.022),P= 0.357] were independent predictors of early renal injury for patients with CHB with NA treatment.
DISCUSSION
For most patients with CHB, NA therapy is safe and well tolerated, but some patients may experience adverse reactions, such as renal insufficiency, myositis,rhabdomyolysis, and lactic acidosis[9,10]. Among the NA drugs, nephrotoxic side effects with ADV are common and mainly manifest as an increase in serum creatinine and a decrease in serum phosphorus, which can cause Fanconi syndrome, renal failure,osteomalacia, and fractures[11,12]. The main reason for its nephrotoxicity is that the organic anion transporter 1 of the proximal tubule has a strong affinity for NAs and can promote the absorption of ADV, resulting in a higher concentration in theproximal tubule. This kind of kidney damage can be reversed after withdrawal of antiviral drugs, but a few patients still show persistent renal damage.
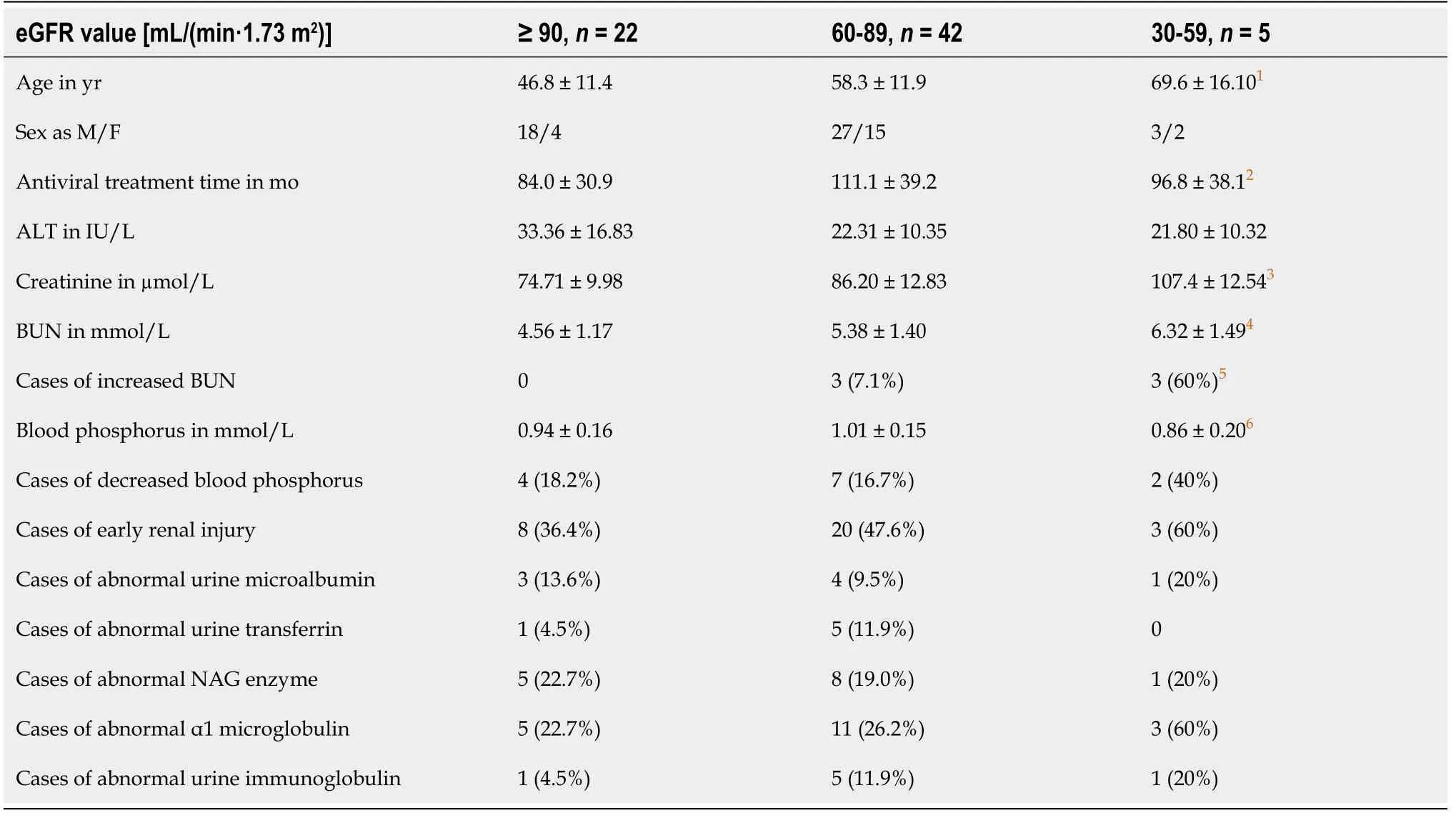
Table 2 Examination results of patients in different estimated glomerular filtration rate value groups
Garaet al[12]carried out an average of 7.4 years of follow-up observations on 51 patients with CHB who received ADV or TDF antiviral therapy and found that 7 patients had proximal renal tubular damage. After the antiviral treatment was changed from ADV to ETV, kidney damage achieved improvement in 6 patients.Chinese scholars also reported that ADV could reduce the eGFR value, while LAM and ETV had no significant impact[9]. Amarapurkaret al[13]analyzed renal function in 292 patients with CHB with a 64-mo treatment of ADV combined with LAM and found that 9.6% of the patients had renal damage, and 27.1% of patients had hypophosphatemia, of which 14 developed Fanconi syndrome. In previous clinical observations, we also found that the renal side effect of ADV was the largest, ETV was the second largest, and LAM was the lowest[14]. In this study, we retrospectively analyzed the clinical data of 69 patients with CHB with an average of 99.7 mo of antiviral treatment with NAs. The results showed that 6 patients (8.7%) had elevated levels of BUN, and 13 patients had hypophosphatemia (18.8%). With the decrease in the eGFR value, the mean values of BUN and creatinine increased significantly, the mean values of serum phosphorus decreased significantly (P< 0.05), and the percentage of patients with hypophosphatemia or early renal injury increased.Moreover, patients with ADV/TDF treatment had a greater percentage of high levels of BUN, early renal injury (60%vs36.4%), hypophosphatemia, and eGFR value less than 70 mL/(min·1.73 m2) compared to patients without ADV/TDF treatment. This further illustrated that long-term treatment with NAs had a certain degree of impact on renal function, especially the potential renal toxicity of ADV, which was significant.Therefore, ADV should not be used in clinical antiviral therapy for patients with CHB.
Early renal mild lesions are reversible, but clinical symptoms are not obvious.Traditional renal function indicators such as urine protein, BUN, and serum creatinine are normal when early mild lesions occur. When the above renal function indicators present abnormalities, approximately 50% of the nephrons have been irreversiblydamaged, and the optimal period of treatment has been missed. Therefore, early renal injury indicators have great significance for the early detection, early diagnosis, and early treatment of renal dysfunction. Early renal injury indicators are generally divided into two categories: (1) Glomerular markers, which are mainly used to detect damage to glomerular function, including urinary microalbumin, urinary immunoglobulin G, transferrin,etc.; and (2) Renal tubule markers, which reflect the status of tubular damage, including urine medium- and low-molecular-weight proteins (such as urine α1 microglobulin, urine β2 microglobulin, urine retinol-binding protein,etc.) and urine enzymes (such as NAG enzyme, lysozyme,etc.). In addition,some nonspecific indicators, such as alkaline phosphatase and GGT, can be used as supplementary markers for detecting proximal tubule injury.
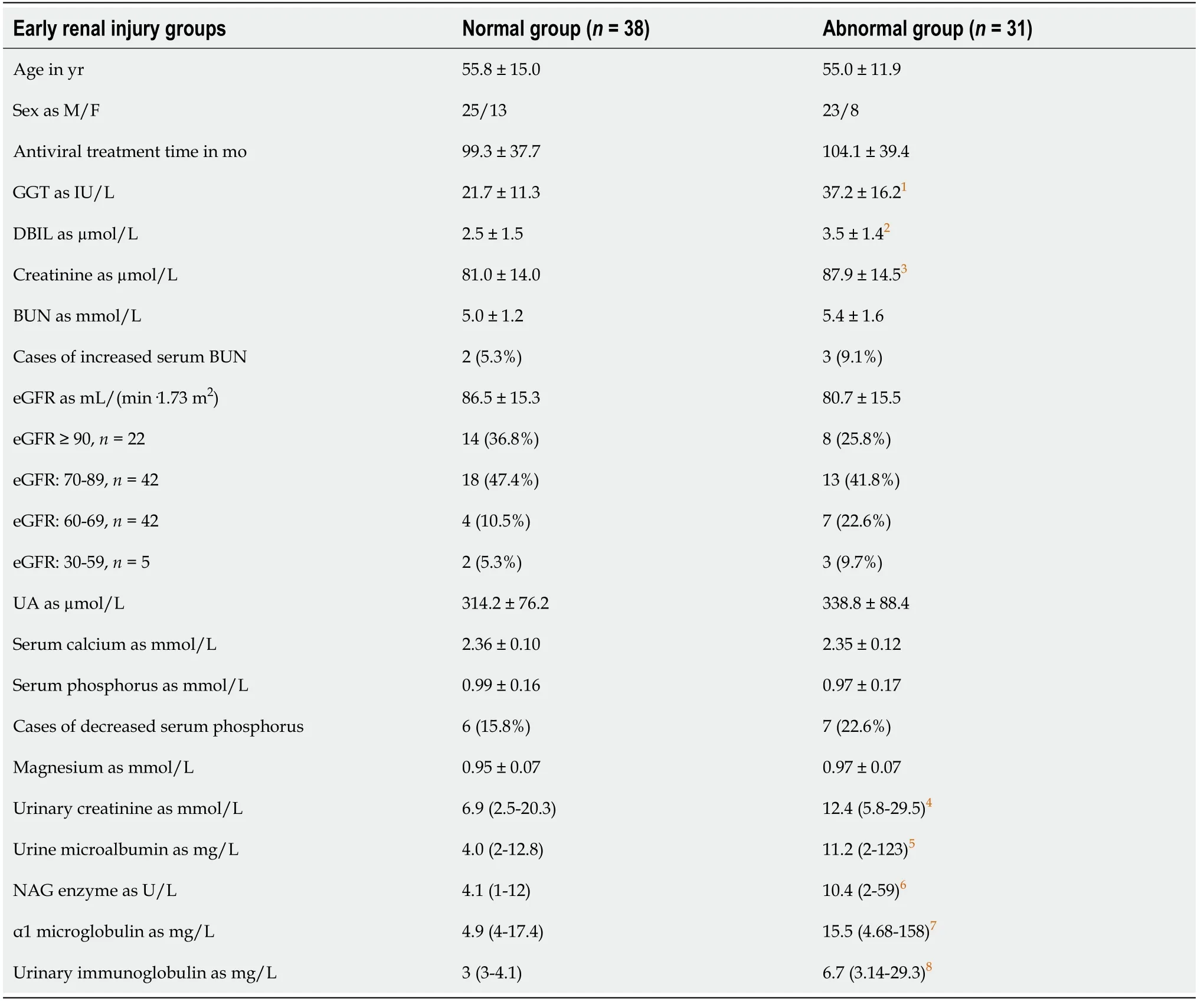
Table 3 Examination results of patients with or without early renal injury
Previous clinical research has mainly focused on reporting renal tubule damage caused by NAs. Of the 69 patients with CHB in our study, a total of 31 (44.9%) patients had abnormal early renal injury indicators, indicating the development of early renal damage, including 9 cases of abnormal urine microalbumin, 7 cases of abnormal urine globulin, 6 cases of abnormal urinary transferrin, 14 cases of abnormal NAG enzyme,and 19 cases of abnormal α1 microglobulin. This result suggested that long-term treatment with NAs had potential toxicity to tubule function as well as glomerulus function, but the probability of renal tubular injury was relatively high. There were no significant differences in the mean values of age, sex, BUN, eGFR, serum uric acid,serum calcium, serum phosphorus, and serum magnesium in patients with or without early renal damage; however, the levels of urinary creatinine, NAG enzyme, α1 microglobulin, and urinary immunoglobulin of patients with early renal damage were significantly higher than those of patients without early renal damage (P< 0.05). While the serum creatinine values and routine urine test results were normal in all patients,early renal injury could be seen in the patients with eGFR ≥ 90, 60-89, and 30-59 mL/(min·1.73 m2), and the incidence of early renal damage was 36.4%, 47.6%, and 60%, respectively. This proved that, compared with traditional renal function indicators, early renal injury indicators could be more sensitive and used earlier to screen for mild renal injury in patients with CHB with NA treatment. Logistic regression analysis results showed that GGT, DBIL, serum creatinine, and age were independent predictors of early renal injury.
CONCLUSION
In summary, the results of this study showed that long-term treatment with NAs had potentially toxic effects on the glomerulus and tubules of the kidney, but renal tubule injury was more common. The incidence of early renal injury reached 44.9%, which should arouse sufficient attention by clinical doctors. Compared with traditional renal function indicators, early renal injury indicators had higher sensitivity and could be used to screen early renal injury in patients with CHB with long-term NA therapy.
ARTICLE HIGHLIGHTS
Research background
Patients with chronic hepatitis B (CHB) with long-term nucleos(t)ide (NA) therapy may experience renal insufficiency. Traditional renal function indicators, such as urine protein, serum urea nitrogen (BUN), and serum creatinine, are normal when early mild lesions occur. Therefore, more sensitive renal function indicators are needed.
Research motivation
To identify more sensitive renal function indicators.
Research objectives
To investigate the significance of early renal injury indicators in evaluating renal injury in patients with CHB with long-term NAs.
Research methods
We collected the clinical data of 69 outpatients with CHB at Peking University First Hospital from March 2018 to January 2020 who had been treated with long-term NA therapy and analyzed the results of early renal injury indicators. Continuous normal distribution data were analyzed by the t-test to determine the difference between two groups. Continuous nonnormally distributed data were analyzed by the Mann-Whitney U-test between two groups. The Kruskal-Wallis H test was used to determine the differences among multiple groups. Enumeration data were analyzed by the chisquare test. The related factors of early renal injury indicators were analyzed by logistic regression analysis.
Research results
The average treatment duration with NAs of the 69 patients with CHB was 99.7 ± 28.7 mo. The cases of patients with elevated BUN and hypophosphatemia were 6 (8.7%)and 13 (18.8%), respectively; 31 (44.9%) patients had abnormal early renal injury indicators, including 9 patients with abnormal urine microalbumin, 7 patients with abnormal urine immunoglobulin, 6 patients with abnormal urine transferrin, and 19 patients with abnormal α1 microglobulin. There were no significant differences in the mean values of age, sex, BUN, estimated glomerular filtration rate (eGFR), serum uric acid, serum calcium, or serum phosphorus between the two groups of patients with and without early renal injury indicators. However, the mean levels of serum creatinine and urine creatinine, NAG enzyme, α1 microglobulin, and urine immunoglobulin in the former group of patients were significantly higher than those in the latter group of patients (P< 0.05). The incidence of early renal injury in patients with eGFR ≥ 90, 60-89 and 30-59 mL/(min·1.73 m2) was 36.4% (8/22), 47.6% (20/42),and 60% (3/5), respectively. Logistic regression analysis results showed that gammaglutamyl transpeptidase [odds ratio (OR) = 1.05 (1.008-1.093),P= 0.020], direct bilirubin [OR = 1.548 (1.111-2.159),P= 0.010], serum creatinine [OR = 1.079 (1.022-1.139),P= 0.006], and age [OR = 0.981 (0.942-1.022),P= 0.357] were independent predictors of early renal injury.
Research conclusions
Patients with CHB treated with long-term NA therapy had a high probability of early renal injury, and early renal injury indicators were highly sensitive and could be used to monitor early renal impairment.
Research perspectives
Retrospective analysis of CHB patients with deteriorating renal function undergoing NAs therapy can be performed to compare the predictive value of different early renal injury indicators for drug toxicity in renal.
ACKNOWLEDGEMENTS
The authors would like to sincerely thank Professor Lu HY (Peking University First Hospital) for his guidance with the study.
 World Journal of Clinical Cases2020年24期
World Journal of Clinical Cases2020年24期
- World Journal of Clinical Cases的其它文章
- Primary duodenal tuberculosis misdiagnosed as tumor by imaging examination: A case report
- Successful endovascular treatment with long-term antibiotic therapy for infectious pseudoaneurysm due to Klebsiella pneumoniae: A case report
- Idiopathic adulthood ductopenia with elevated transaminase only: A case report
- Takotsubo cardiomyopathy associated with bronchoscopic operation: A case report
- Extracorporeal shock wave therapy treatment of painful hematoma in the calf: A case report
- Rare case of drain-site hernia after laparoscopic surgery and a novel strategy of prevention: A case report
