Takotsubo cardiomyopathy associated with bronchoscopic operation: A case report
Bi-Feng Wu, Jia-Ran Shi, Liang-Rong Zheng
Bi-Feng Wu, Jia-Ran Shi, Liang-Rong Zheng, Department of Cardiology, The First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou 310000, Zhejiang Province,China
Abstract BACKGROUND Takotsubo cardiomyopathy (TTC), a syndrome of acute left ventricular (LV)dysfunction, is characterized by transitory hypokinesis of LV apices with compensatory hyperkinesis of the LV basal region. The symptoms of TTC mimic acute myocardial infarction, without significant coronary stenoses on coronary angiography. Echocardiogram plays a key role in the diagnosis and prognosis of TTC. New indicators from echocardiograms may be helpful in disease evaluation.CASE SUMMARY A 67-year-old man with a 10-year history of non-small cell lung cancer was admitted to our hospital for emerging facial edema and dry cough. Bronchoscopic lavage, brushing, and biopsy were performed to evaluate tumor progression.During this procedure, he complained of left chest pain, nausea, and vomiting,with elevated troponin levels. Electrocardiogram showed sinus bradycardia with ST-segment elevation in I, AVL, and V4 to V6 leads. Coronary angiography revealed mild stenosis in the right coronary artery. Echocardiography showed hypokinesis of LV apices with compensatory hyperkinesis of the LV basal region.At the 7-d follow-up, echocardiographic pressure-strain analysis showed a normal LV ejection fraction, but partial recovery of LV myocardial work, which fully recovered 5 mo later.CONCLUSION This is a case of TTC caused by bronchoscopic operation. We strongly recommend noninvasive myocardial work measured by echocardiographic pressure-strain analysis as a necessary supplementary test for the long-term follow-up of TTC.
Key Words: Takotsubo cardiomyopathy; Bronchoscope; Left ventricular myocardial work;Case report; Non-small cell lung cancer
INTRODUCTION
Takotsubo cardiomyopathy (TTC), a syndrome of acute left ventricular (LV)dysfunction, is triggered by psychological or physiological stress. However, TTC induced by tracheoscopy is rare. A previous study has demonstrated its long-term risk of cardiogenic shock[1]. Typical TTC manifests as acute chest pain, dyspnea, or palpitation, accompanied by abnormal electrocardiograph and myocardial enzymes,which mimic acute myocardial infarction but no significant coronary stenoses. Routine echocardiography shows transitory hypokinesis of LV apices with compensatory hyperkinesis of LV basal regions. Novel markers derived from echocardiographic pressure-strain analysis may help to evaluate the progression of TTC.
CASE PRESENTATION
Chief complaints
A 67-year-old man with a 10-year history of non-small cell lung cancer (NSCLC) was admitted to our hospital for emerging facial edema and dry cough within the past 1 mo. No reduced activity tolerance, paroxysmal nocturnal dyspnea, or orthopnea was shown. Initial electrocardiogram (ECG) and myocardial enzymes were normal. To evaluate the progression of lung lesions, the patient accepted bronchoalveolar lavage,brushing, and transbronchial lung biopsy with a bronchoscope and endobronchial ultrasonography. Routine pre-medications (atropine, 0.6 mg, oral; 2% lidocaine aerosol inhalation) were given before the procedure. During this procedure, he complained of left chest pain, nausea, and vomiting. Electrocardiograph monitoring showed hypertension (180/94 mmHg). ECG showed sinus bradycardia with ST-segment elevation in I, AVL, and V4 to V6 leads. Troponin T level rose to 0.138 ng/mL(reference range < 0.06 ng/mL) within 1 h after operation, whereas it rose to 12.299 ng/mL 6 h later. Considering symptoms and laboratory results, the patient underwent emergency coronary angiography, but only mild stenosis in the right coronary artery was observed. Echocardiography showed hypokinesis of LV apices with compensatory hyperkinesis of the LV basal region.
History of present illness
The patient’s medical history was NSCLC and bronchiectasia. There was no other history of illness.
History of past illness
The patient was diagnosed with NSCLC (pT1N1M0) 10 years ago. After pulmonary resection, he successively received chemotherapy. Then he took gefitinib as the only treatment for 6 years. One month ago, he presented facial edema and dry cough.Computed tomography at a local hospital showed mild enlargement of tumor size in the right lower lobe as compared to former records. No cardiomyopathy, coronary heart disease, or arrhythmia was recorded before this hospitalization.
Personal and family history
The patient was a retired worker and had no family history of any major diseases.
Physical examination
Before the bronchoscopic operation, the patient’s blood pressure was 141/75 mmHg with a heart rate of 59 bpm. He breathed on room air smoothly with lower right lung breath sound. His heart examination was normal, and no murmurs or gallops were detected.
Shortly after bronchoalveolar lavage and lung biopsy, his blood pressure rose to 180/94 mmHg. He was anxious and his breath was rapid. His heart rate dropped to 48 bpm and improved rapidly after suspending the examination. On auscultation, no murmur, gallop, or wheeze was detected.
Laboratory examinations
Baseline troponin T and other myocardial enzymes were normal. As shown in Figure 1, the level of troponin T elevated at 0.138 ng/mL (normal range 0-0.06) 1 h later and rapidly elevated at 12.299 ng/mL 6 h later. The levels of creatine kinase,creatine kinase-MB, and hydroxybutyrate dehydrogenase mildly elevated 6 h later and lactic dehydrogenase elevated 12 h later (Figure 2).
Imaging examinations
The initial 12-lead ECG revealed a normal sinus rhythm with an appropriate rate (77 bpm). With the appearance of symptoms, the ECG showed an extensive elevation of ST-segment in I, AVL, and V4 to V6 leads (Figure 3).
In sum, the working hypothesis of ST-segment elevation myocardial infarction(STEMI) was considered. This patient underwent emergency coronary angiography(CA), which revealed mild stenosis in the middle segment of the right coronary artery.
Previous echocardiogram results were normal. A transthoracic echocardiogram(ECHO) was made 24 h after the initial symptoms (Figure 4). The results showed significant hypokinesis of LV apices with compensatory hyperkinesis of the LV basal region. LV ejection fraction (LVEF) was 49%. No abnormality was found in the chamber size or valvular. To assess his LV function, LV global myocardial work index(LVGWI), global myocardial work efficiency (LVGWE), global constructive myocardial work (LVGCW), global wasted myocardial work (LVGWW), and global longitudinal strain (LVGLS) derived from pressure-strain analysis and noninvasive blood pressure measurements were evaluated further (Figure 5). The LVGWI level was 729 mmHg%,the LVGWE level was 72%, the LVGCW level was 895 mmHg%, the LVGWW level was 284 mmHg%, and the LVGLS was 8%. The apical-to-basal strain ratio of the LV was 0.34, and the apical-to-basal work ratio was 0.42 (Table 1).
FINAL DIAGNOSIS
Based on all observations described in the previous sections, this patient was diagnosed with TTC.
TREATMENT
The patient was treated with oral furosemide, spironolactone, isosorbide mononitrate,diltiazem, aspirin, and clopidogrel, as well as oxygen uptake through a nasal catheter and electrocardiograph monitoring. After CA, the medication was adjusted to oral furosemide, spironolactone, and aspirin. Over the ensuing days, his symptoms improved, and he was free from oxygen therapy. Other medication included gefitinib for tumor lesions.
OUTCOME AND FOLLOW-UP
After aggressive treatment, the prior symptoms disappeared. At the 7-d follow-up, the patient reported an improvement in exercise tolerance without oxygen support. ECHO showed a partial recovery of LV apical contractility. The LVEF level was 62%, the LVGWI level was 940 mmHg%, the LVGWE level was 77%, the LVGCW level was1268 mmHg%, the LVGWW level was 369 mmHg%, and the LVGLS was 12%. The apical-to-basal strain ratio of the LV was 0.89, and the apical-to-basal work ratio was 0.71 (Table 1). At the 5-mo follow-up, his cardiac function fully recovered according to the results of ECHO (Table 1).
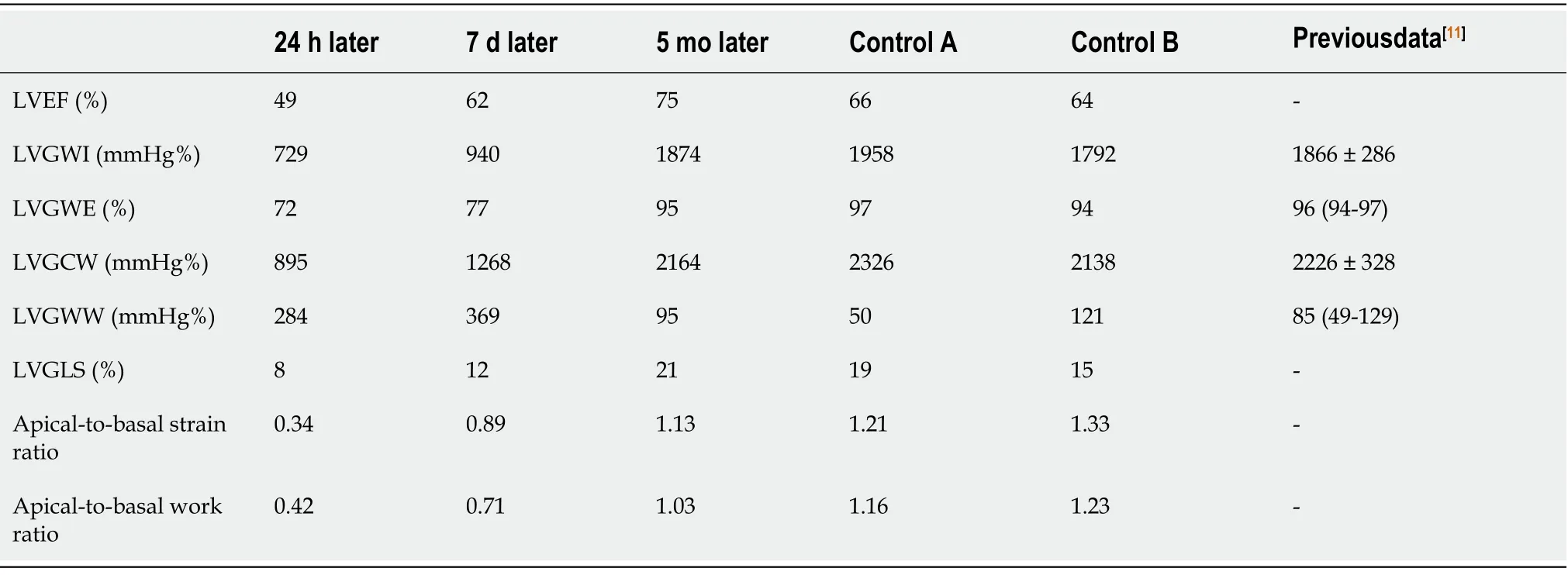
Table 1 Myocardial work of this patient in echocardiography after illness
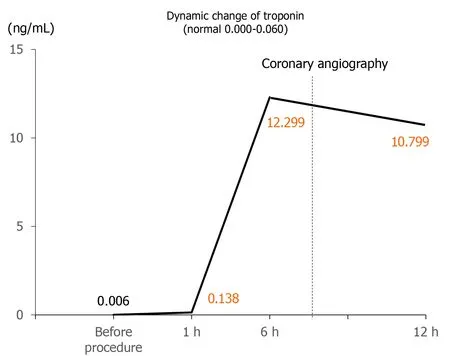
Figure 1 Dynamic change of troponin before and after illness.
DISCUSSION
TTC, also known as stress-induced cardiomyopathy, is characterized as an acute severe, but reversible LV dysfunction. TTC has symptoms similar to acute myocardial infarction with abnormal troponin and ECG. Inducement of TTC is caused mostly by psychological stress, however, TTC caused by physical irritation had been reported,increasing the difficulty of distinguishing it from other diseases. Patients with TTC and cardiogenic shock have high mortality during 5-year follow-up, although the proportion is lower than that in patients with myocardial infarction and cardiogenic shock[1].
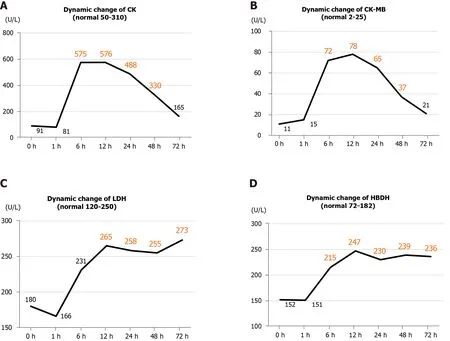
Figure 2 Dynamic changes of four myocardial enzymes before and after illness. A: Creatine kinase; B: Creatine kinase-MB; C: Lactic dehydrogenase;D: Hydroxybutyrate dehydrogenase. CK: Creatine kinase; CK-MB: Creatine kinase-MB; LDH: Lactic dehydrogenase; HBDH: Hydroxybutyrate dehydrogenase.
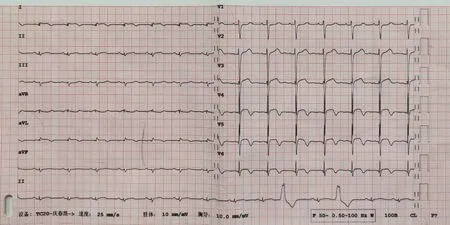
Figure 3 Twelve-lead electrocardiogram when symptoms appeared.
The pathophysiological mechanisms of TTC remain elusive. Although the association between TTC and catecholamine is wildly accepted[2], there are other participants in the progression of TTC. Myocardial edema was found in the acute stage of TTC by cardiac magnetic resonance imaging[3]. A recent study further revealed macrophage inflammatory infiltrate in the myocardium and confirmed a low-grade chronic inflammatory state in TTC patients, demonstrating that inflammation is pivotal in the pathophysiology and natural history of TTC[4].
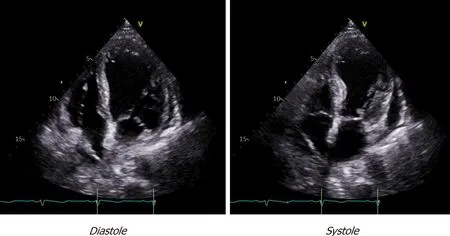
Figure 4 Transthoracic echocardiogram showing hypokinesis of left ventricular apices with compensatory hyperkinesis of left ventricular basal region in systole.
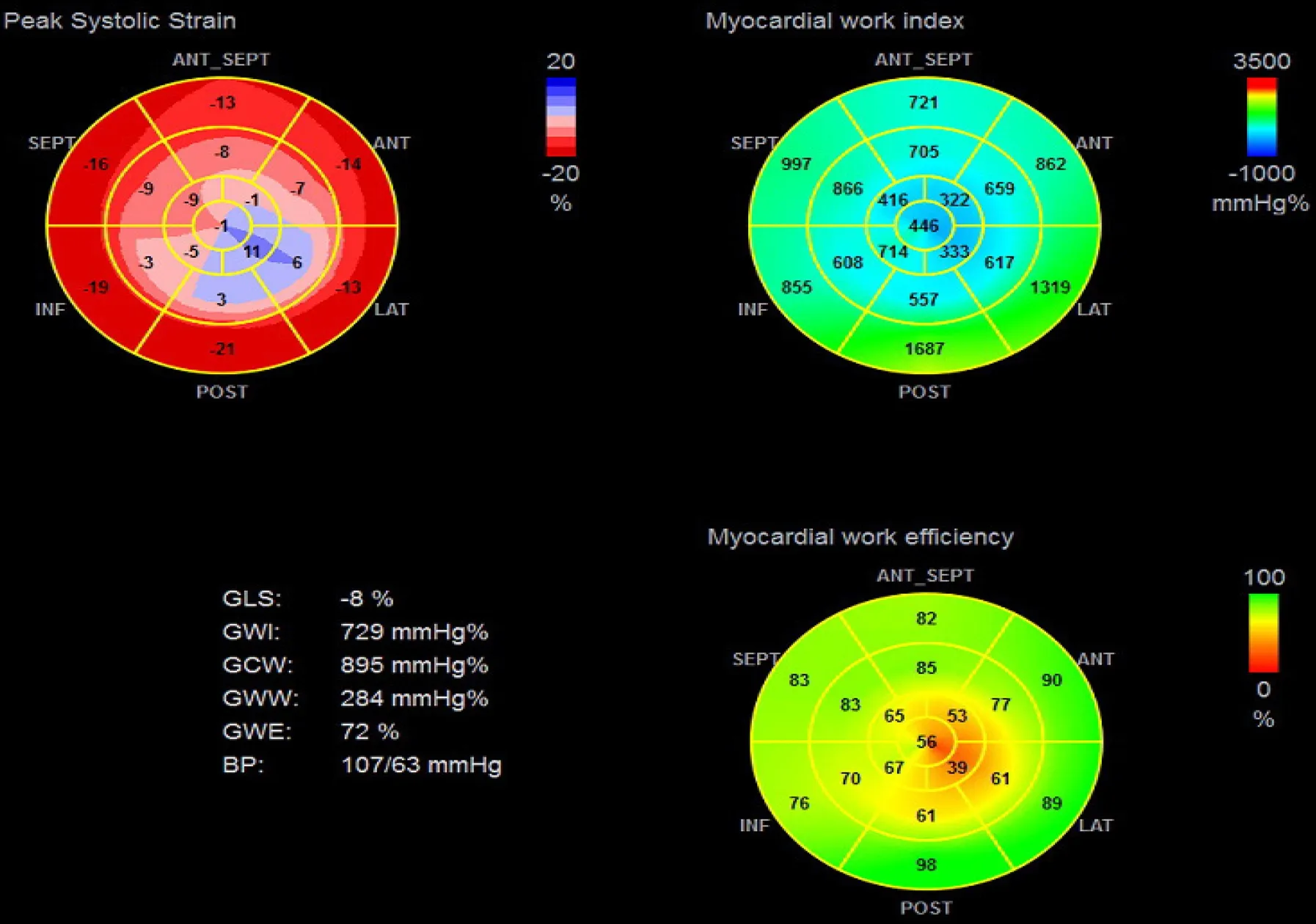
Figure 5 Echocardiographic pressure-strain analysis showing left ventricular peak systolic strain, myocardial work index, and myocardial work efficiency in bull’s eye map. GLS: Global longitudinal strain; GWI: Global myocardial work index; GCW: Global constructive myocardial work; GWW: Global wasted myocardial work; GWE: Global myocardial work efficiency; BP: Blood pressure.
In this case report, we present a patient who developed TTC during a bronchoscopic operation. He had been diagnosed with NSCLC and was presently treated with gefitinib. Previous studies had reported gefitinib-related cardiac dysfunction. One case presented fatal hypersensitivity myocarditis 1 wk after administration of gefitinib[5].Another case had gefitinib-induced cardiomyopathy 7 mo after administration, and the cardiac function recovered through aggressive treatment, as well as the discontinuation of gefitinib[6]. However, the patient in this case report had been using gefitinib for 6 years. Echocardiogram results and clinical symptoms before the bronchoscopic operation were not sufficient to establish a diagnosis of heart failure.More attention has been paid to the connection between cardiac disfunction and bronchoscopic operation. Rajwaniet al[7]reported five cases of TTC in patients who received bronchodilator therapy for chronic obstructive lung disease and reduced bronchospasm. Miyoshiet al[8]reported a case who underwent TTC after flexible bronchoscopy. A novel subgroup of bronchogenic stress-induced cardiomyopathies have been proposed as one of the main triggers of TTC. Although 2% lidocaine aerosol inhalation is administered routinely before the operation, increasing the risk of bronchospasm, dyspnea was relieved quickly after low-flow oxygenviaa nasal catheter. Therefore, we postulated that the discomfort or pain caused by the mechanical stimulation of the bronchoscope and the following physical and psychological pressure triggered this deterioration.
The patient’s symptoms improved during hospitalization, and the follow-up results also demonstrated the recovery of LVEF. However, hypokinesis in the local myocardium was the main disfunction of TTC, and LVEF may not accurately reflect the exhaustion or recovery of local myocardial kinesis. In this study, we have measured some novel markers to evaluate myocardial function, which have been reported as meaningful markers for heart failure caused by cardiac amyloidosis[9].According to the normal value from previous results[10]and our data, the myocardial mechanical energy and contraction in LV apices are only partially restored 7 d later. At the 5-mo follow-up, the results from ECHO showed full recovery of cardiac function including LV apical contraction. Many studies have reported an early recovery of left ventricular systolic function in TTC patients, from 48 h to 3 d[8,11]. It follows that the improvement of LVEF is “confusing”, causing less attention to these patients whose local myocardial function (mainly the apices) is still poor. This may be the reason for the poor prognoses of many TTC patients who “recover” in a short time, as defined by LVEF, with damaged local myocardial work[1]. Long-term monitoring of myocardial work is therefore necessary for TTC patients to accurately evaluate LV function.
CONCLUSION
In conclusion, we have reported a case of TTC caused by a bronchoscopic operation and strongly recommend noninvasive myocardial work measured by echocardiographic pressure-strain analysis as a necessary supplementary test for the long-term follow-up of TTC.
 World Journal of Clinical Cases2020年24期
World Journal of Clinical Cases2020年24期
- World Journal of Clinical Cases的其它文章
- Primary duodenal tuberculosis misdiagnosed as tumor by imaging examination: A case report
- Successful endovascular treatment with long-term antibiotic therapy for infectious pseudoaneurysm due to Klebsiella pneumoniae: A case report
- Idiopathic adulthood ductopenia with elevated transaminase only: A case report
- Extracorporeal shock wave therapy treatment of painful hematoma in the calf: A case report
- Rare case of drain-site hernia after laparoscopic surgery and a novel strategy of prevention: A case report
- Oral myiasis after cerebral infarction in an elderly male patient from southern China: A case report
