Laparoscopic left lateral sectionectomy in pediatric living donor liver transplantation by single-port approach: A case report
Hong-Yu Li, Lin Wei, Zhi-Gui Zeng, Wei Qu, Zhi-Jun Zhu
Hong-Yu Li, Lin Wei, Zhi-Gui Zeng, Wei Qu, Zhi-Jun Zhu, Liver Transplantation Center, Beijing Friendship Hospital, Capital Medical University, Beijing 100050, China
Abstract BACKGROUND Single-port laparoscopy has been used in a variety of abdominal operations. We report the first case of single-port laparoscopic left lateral sectionectomy in pediatric laparoscopic living donor liver transplantation.CASE SUMMARY A 28-year-old man volunteered for living liver donation to his daughter who was diagnosed with liver cirrhosis and portal hypertension after the Kasai procedure for biliary atresia. His body mass index was 20.5 kg/m2. Liver dynamic computed tomography showed: (1) Left lateral graft volume of 232.76 cm3 with a graft-torecipient weight ratio of 2.59%; and (2) Right hepatic artery derived from the superior mesenteric artery. A single-port access system was placed through a transumbilical incision, including four trocars: two 12-mm ports for a camera and endoscopic stapler and two 5-mm working ports. Liver parenchyma was dissected by a Harmonic and Cavitron Ultrasonic Surgical Aspirator, while bipolar was used for coagulation. The bile duct was transected above the bifurcation by indocyanine green fluorescence cholangiography. The specimen was retrieved from the umbilical incision. The total operation time was 4 h without blood transfusion. The final graft weight was 233.6 g with graft-torecipient weight ratio of 2.60%. The donor was discharged uneventfully on postoperative day 4.CONCLUSION Single-port laparoscopic left lateral sectionectomy is feasible in pediatric laparoscopic living donor liver transplantation in an experienced transplant center.
Key Words: Pediatric living donor liver transplantation; Laparoscopy; Single-port approach; Intraoperative indocyanine green fluorescence cholangiography; Treatment;Case report
INTRODUCTION
Laparoscopic hepatectomy has been proved to be a feasible and safe procedure in liver surgery in recent decades[1]. Since the first single-port laparoscopic hepatectomy was reported in 2010 by Kobayashiet al[2], single-port laparoscopy has been applied to a variety of abdominal operations, especially laparoscopic left lateral sectionectomy (LLLS)[3]. In 2002, Cherquiet al[4]first described L-LLS for adult-to-pediatric donation.The safety and feasibility of the technique was similar to those obtained by conventional approaches for both donors and recipients[5]. Nowadays, L-LLS is acknowledged as a standard practice in pediatric living donor liver transplantation(PLDLT)[6,7]. Decreasing donors’ perioperative risks is essential in LDLT. Compared to standard multiport laparoscopic hepatectomy, single-port laparoscopic hepatectomy has been adopted to reduce the number of ports and corresponding abdominal incisions, which may lead to rapid recovery and superior cosmetic results, conferring potential advantages over multiport procedures[8]. As a result, single-port L-LLS is considered to potentially benefit donors. We report the first case of L-LLS in PLDLT using a single-port approach.
CASE PRESENTATION
Chief complaints
The donor was a 28-year-old man who volunteered for living liver donation to his daughter. The recipient was a 14-mo-old girl who presented to our center with the complaint of repeated hematemesis for 2 wk.
History of present illness
The donor had no significant present medical condition. The recipient was diagnosed with biliary atresia 1 mo after birth. A Kasai operation was performed. Approximately 2 wk before presenting to our center, she suffered from repeated hematemesis three times. Hepatosplenomegaly and esophagogastric varices were detected after physical and endoscopic examination.
History of past illness
The donor and recipient had no other significant medical history. A history of hypertension, diabetes, coronary heart disease and other chronic disease was denied.
Personal and family history
The donor and recipient had no significant personal and family history.
Physical examination
The donor’s weight was 62 kg and height was 174 cm, with a body mass index (BMI)of 20.5 kg/m2. The recipient’s physical examination showed liver disease with mild jaundice, poor nutrition, abdominal swelling and hepatosplenomegaly. Her weight was 9 kg and height was 75 cm, with a BMI of 16 kg/m2.
Laboratory examinations
For the donor, laboratory examinations showed no abnormal results, and he was Child–Pugh Grade A (score 5). For the recipient, laboratory examinations on admission revealed a hemoglobin level of 91 g/L, platelet count of 163 × 109/L, white blood cell count of 7.66 × 109/L, alanine aminotransferase (ALT) 28 U/L, albumin 30.8 g/L, total bilirubin (TBIL) 16.78 µmol/L, direct bilirubin 7.61 µmol/L, and creatinine 22.9 µmol/L. Her prothrombin time was 14.50 s, and international normalized ratio was 1.29. Combined with imaging examination, she was Child–Pugh Grade B (score 7)and pediatric end-stage liver disease score was 8.
Imaging examinations
For the donor, liver dynamic computed tomography and magnetic resonance imaging showed: (1) Left lateral graft volume of 232.76 cm3with a graft-to-recipient weight ratio of 2.59%; (2) Right hepatic artery derived from the superior mesenteric artery;and (3) No anatomical variation in the portal vein, hepatic vein and bile duct(Figure 1).
FINAL DIAGNOSIS
The recipient was diagnosed with liver cirrhosis and portal hypertension after the Kasai operation due to biliary atresia.
TREATMENT
A single-port L-LLS was scheduled and performed on the donor for the following reasons: (1) the donor was thin with a BMI of 20.5 kg/m2, which facilitated hepatoduodenal ligament exposure during laparoscopy; (2) he had a shared arterial trunk of the middle and left hepatic arteries, while the right hepatic artery derived from the superior mesenteric artery, which made dissection and preservation easier;and (3) there was no anatomical variation in the left bile duct, portal vein and hepatic vein. Intraoperative indocyanine green (ICG) fluorescence cholangiography was used to determine the bifurcation and division point of the bile duct. The operation was approved by the Ethics Committee of Beijing Friendship Hospital, Capital Medical University.
Laparoscopy was performed under carbon dioxide pneumoperitoneum. The insufflation pressure was set at 13 mmHg throughout the surgery. The patient was placed in the supine position in the 30° left and 30° reversed Trendelenburg position.The surgeon stood by the patient’s right side and the assistant and scopist stood by the patient’s left side. A single-port access system was placed through a transumbilical incision, including four trocars: two 12-mm ports for a camera and endoscopic stapler and two 5-mm working ports. A small incision in the right side of the anterior axillary line for the surgical drain was used to place an additional 5-mm port for further assistance (Figure 2). The left portal vein and hepatic artery were temporarily clamped to control bleeding. The liver parenchyma was dissected by the Harmonic and Cavitron Ultrasonic Surgical Aspirator, while bipolar was used for coagulation. The bile duct was transected above the bifurcation by intraoperative ICG fluorescence cholangiography (Figure 3). A one-side linear stapler was used to transect the left hepatic vein. The specimen was retrieved from the umbilical incision. The total operation time was 4 h without blood transfusion. The final graft weight was 233.6 g with graft-to-recipient weight ratio of 2.60%.
OUTCOME AND FOLLOW-UP

Figure 1 Preoperative graft evaluation. A: Right hepatic artery derived from the superior mesenteric artery; B: Portal vein and hepatic vein; C: Bile duct.

Figure 2 Arrangement of trocars.
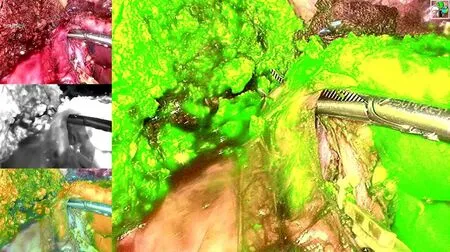
Figure 3 Intraoperative indocyanine green fluorescence cholangiography.
The patient-controlled analgesia pump was retrieved within the first 24 h after surgery. The donor’s ALT was 239 U/L, aspartate aminotransferase (AST) was 116 U/L, gamma-glutamyltransferase (GGT) was 22 U/L, and TBIL was 22.57 µmol/L on postoperative day 1, while ALT was 107 U/L, AST was 63 U/L, GGT was 26 U/L, and TBIL was 17.0 µmol/L on postoperative day 3. No complications were observed. The donor was discharged uneventfully on postoperative day 4 (Figure 4). The graft function almost recovered to normal in the recipient on postoperative day 14 (ALT: 44 U/L, AST: 25.9 U/L, GGT: 53 U/L and TBIL: 9.22 µmol/L) without any surgical complications, such as biliary and vascular complications that could theoretically have been caused by imperfect graft procurement.

Figure 4 Photograph of the cosmetic result of a single-port laparoscopic left lateral sectionectomy. A: Immediately after surgery; B:Postoperative day 4.
DISCUSSION
Due to the advantages of little trauma, reduced postoperative pain, rapid recovery,shorter hospital stay, and minimal incision, single-port L-LLS has been proved to be a safe and feasible approach in liver surgery when treating liver lesions, especially for benign, small and peripheral lesions[9,10]. A recent study revealed that single-port L-LLS incurred a shorter operating time and postoperative hospital stay compared to multiport surgery[11]. Cherquiet al[4]first reported a comparative analysis of L-LLS,resulting in a longer operating time in the laparoscopic group, with significantly decreased blood loss and a trend towards lower overall morbidity compared to the open surgery group. In another retrospective study, Kimet al[5]reported that the laparoscopic group had a significantly shorter hospital stay, whereas the operating time, blood loss, warm ischemic time, and out-of-pocket medical costs were comparable between the open and laparoscopic groups. After a propensity score matching analysis by Broeringet al[12], the L-LLS group showed a significant lower blood loss and overall donor complication rate, lower postoperative pain scores, and shorter hospital stay, whereas the operating time and warm ischemic time were significantly longer compared to those in the open group. Therefore, hypothetically,single-port L-LLS should be the most minimally invasive approach for donor surgery in LDLT, compared to either a multiport approach or open surgery.
Most previous comparisons between single-port and traditional multiport laparoscopic hepatectomy were based on liver tumor resection[3,10,11]. Although cirrhosis related to hepatitis virus infection and tumor proximal to major vessels might affect the surgical procedure, single-port procedures still show advantages over multiport approaches. In LDLT, with strict selection criteria, donors are volunteers with normal liver function and liver parenchyma. This might decrease the difficulty with dissection of the liver hilum and parenchyma. In addition, intraoperative bleeding can be controlled more effectively in the donor’s operation. Thus, single-port L-LLS should be an appropriate procedure in PLDLT.
Although the “chopstick effect” and loss of instrumental triangulation are the main barriers in developing single-port laparoscopic hepatectomy[13], according to a technical feature of the surgical intervention of the “caudal” approach, L-LLS should be a good indication for the single-port approach[14]. The parenchymal division can be completed “bottom-up” to the hepatic venous entry after liver mobilization and vessel dissection[14,15]. Compared to right hemihepatectomy or posterosuperior sectionectomy,because the resection can only be performed along the plane of a linear field of view,single-port L-LLS can be performed more easily and safely from the transumbilical incision, without the help of articulation of traditional laparoscopic instruments. This may not increase intraoperative risks in graft procurement.
According to the consensus when adopting a single-port approach in laparoscopic hepatectomy, a small incision is acceptable in the upper abdomen for the surgical drain and is used to place an additional 5-mm port for the safe preparation and resection of the liver[3,10,11]. In our case, in the right side of the anterior axillary line, an additional 5-mm trocar was placed to facilitate liver mobilization and exposure during the parenchymal division.
Donor safety is the primary concern in LDLT. Intraoperative bleeding control and bile duct transection are two major manipulations. Hypothetically, in the case of severe intraoperative bleeding, the transumbilical port could easily be converted into a hand-assisting port and thus be used for manual compression of the liver[3]. After mild dissection of the liver hilum, intraoperative ICG fluorescence cholangiography can be used to determine the bifurcation and division point of the bile duct[16].
An experienced and skilled surgical team (both for donor hepatectomy and advanced laparoscopic surgery) is important for this procedure. Our surgical team had extensive experience in PLDLT (> 1000 cases), laparoscopic liver resection (> 300 cases)and L-LLS (> 60 cases). In addition, L-LLS by the single-port approach should be adopted under strict selection criteria. A suitable donor should meet the following conditions: (1) A thin donor who facilitates better exposure and easier dissection of the hepatic hilum during laparoscopy; (2) Shared arterial trunk of the middle and left hepatic arteries, while the right hepatic artery is derived from the superior mesenteric artery, which makes it easier to be dissected and preserved; and (3) No anatomical variation in the left bile duct, portal vein and hepatic vein.
The success of PLDLT in our case was determined by the outcomes of both donor and recipient. The donor was discharged on postoperative day 4 without any complications, including liver dysfunction, bile leakage or postoperative bleeding. No incisional hernia was found after 3-mo follow up. The recipient’s liver function almost recovered to normal on postoperative day 14 and she was discharged on postoperative day 21 without biliary and vascular complications. The strict selection of donor and recipient and the experienced surgical team might have contributed to these results.
CONCLUSION
This is the first report of L-LLS for PLDLT using a single-port approach. However,large randomized controlled trials and large case-controlled comparative studies are needed to evaluate the techniques and potential benefits of single-port L-LLS.
 World Journal of Clinical Cases2020年23期
World Journal of Clinical Cases2020年23期
- World Journal of Clinical Cases的其它文章
- Novel triple therapy for hemorrhagic ascites caused by endometriosis: A case report
- Discontinuous polyostotic fibrous dysplasia with multiple systemic disorders and unique genetic mutations: A case report
- Primary breast cancer patient with poliomyelitis: A case report
- Symptomatic and optimal supportive care of critical COVID-19: A case report and literature review
- Multiple ectopic goiter in the retroperitoneum, abdominal wall, liver,and diaphragm: A case report and review of literature
- Acute celiac artery occlusion secondary to blunt trauma: Two case reports
