Therapies to modulate gut microbiota: Past, present and future
Akshita Gupta, Srishti Saha, Sahil Khanna
Abstract The human gut microbiota comprises of a complex and diverse array of microorganisms, and over the years the interaction between human diseases and the gut microbiota has become a subject of growing interest. Disturbed microbial milieu in the gastrointestinal tract is central to the pathogenesis of several diseases including antibiotic-associated diarrhea and Clostridioides difficile infection (CDI). Manipulation of this microbial milieu to restore balance by microbial replacement therapies has proven to be a safe and effective treatment for recurrent CDI. There is considerable heterogeneity in various aspects of stool processing and administration for fecal microbiota transplantation (FMT) across different centers globally, and standardized microbioal replacement therapies offer an attractive alternative. The adverse effects associated with FMT are usually mild. However, there is paucity of data on long term safety of FMT and there is a need for further studies in this regard. With our increasing understanding of the host-microbiome interaction, there is immense potential for microbial replacement therapies to emerge as a treatment option for several diseases. The role of microbioal replacement therapies in diseases other than CDI is being extensively studied in ongoing clinical trials and it may be a potential treatment option for inflammatory bowel disease, irritable bowel syndrome,obesity, multidrug resistant infections, and neuropsychiatric illnesses. Fecal microbiota transplantation for non-CDI disease states should currently be limited only to research settings.
Key words: Fecal microbiota transplantation; Microbial replacement therapies;Clostridioides difficile infection; Microbiome; Microbiota; Inflammatory bowel disease
INTRODUCTION
Over the past decade the interaction between human health and the microbiome has become a subject of growing interest. The human microbiome refers to the total number of microorganisms and their associated genetic material comprised within the body, whereas the term microbiota is defined as the entire population of microorganisms (bacteria, virus, fungi) in a given environment[1]. The human microbiome has co-evolved with humans throughout the millennia, with the development of specific communities of microbes occupying specific anatomical niches within the human body[2].
GUT MICROBIOTA
The human body harbours about 100 trillion microorganisms, which makes the number of microbial cells almost similar to the total number of human cells and 10-fold more than the number of nucleated human cells[3-5]. The majority of these reside in the human gastrointestinal tract which is colonized by anywhere between 500 and 2000 microbial species in its healthy state, thus forming a rich and diverse microbiome[6]. Among these, the four most common bacteria belong to the phyla Firmicutes, Bacteroidetes, Actinobacteria and Proteobacteria[7]. It is now well known that commensal microbiota are essential in maintaining homeostasis via production of metabolites that regulate immune responses, mucosal barrier function, suppression of pathogen overgrowth, vitamin and energy source generation[3,8]. The density of bacteria exponentially increases from the proximal to the distal gastrointestinal tract,reaching its peak in the colon. Furthermore, the microbiome evolves - with time, and in response to host as well as environmental factors[9]. The composition and diversity of microbiota within specific anatomical locations differs among people due to variations in hygiene, social behaviors, and genetics as well as in diet[10,11].Colonization with normal commensal organisms begins shortly after birth, and the introduction and reintroduction of flora continues throughout life from our routine interactions with each other. However, when imbalance occurs in this microbial ecosystem, it can contribute to a multitude of disorders. This disturbed microbial milieu is termed “dysbiosis”. Dysbiotic microbiota is associated with antibioticassociated diarrhea, Clostridioides difficile infection (CDI), inflammatory bowel disease(IBD), irritable bowel syndrome (IBS), multidrug-resistant infections, obesity,metabolic syndrome, non-alcoholic fatty liver disease, neuropsychiatric diseases,diabetes mellitus and systemic autoimmune diseases, amongst others[12-14].Conceivably, restoration of the gastrointestinal microbial composition could be useful in managing these conditions.
MICROBIAL REPLACEMENT THERAPIES
Microbial replacement therapy or fecal microbial transplantation (FMT) refers to the process of transferring gut microbiota from a healthy individual to one harboring a dysbiotic microbiome, with the aim of restoring eubiosis[15,16]. It is based on the rationale that manipulation of the microbiome could prove potentially therapeutic for disease states with an altered microbial composition. Probiotics have been used to treat conditions associated with a disrupted microbiome, but have shown limited efficacy. A plausible explanation for this could be a difference in the diversity of the organisms in the probiotics compared to microbes in the healthy human gut. Thus,FMT with representation of the entire naturally occurring gut microbiota, represents a potentially superior alternative to probiotics. It has rapidly emerged as a treatment option for recurrent CDI.
THE PAST
FMT was first described in the 4thcentury in China by Ge Hong, where a doctor administered human fecal suspension by mouth for food poisoning or severe diarrhea[17]. Li Shizhen described use of oral fresh or fermented fecal preparations for treating various gastrointestinal conditions like diarrhea, vomiting and constipation,in the 16thcentury Ming dynasty[17]. In the 17thcentury, an anatomist, Fabricius Aquapendente, used FMT in veterinary medicine[18]. Eiseman et al[19], in 1958,described the use of FMT in modern medicine by successfully treating four patients with pseudomembranous colitis from Micrococcus pyogenes by giving them fecal enemas. Initially, FMT was first used to successfully treat CDI in 1983 by retention enemas[20]. This remained the most common technique till the 1990s when newer methods of administration emerged, like infusion via nasogastric tube, upper endoscopic and colonoscopic techniques, as well as self-administered enemas[21].
THE PRESENT
FMT is being increasingly used to safely and effectively treat recurrent, and maybe refractory, CDI. It restores the diversity of the gut microbiota and has achieved cure rates of over 85%[22-24]. Its potential role in disease states other than CDI is also being studied extensively in ongoing clinical trials.
Indications
Fecal microbiota transplantation is gradually surfacing as a novel treatment modality for several disease states with an alteration in their gut microbial compositions including, but not limited to CDI, IBD, IBS, non-alcohol fatty liver disease, obesity,neuropsychiatric illnesses, multidrug resistant organisms, etc.[25-27]. However, microbial replacement therapies are currently only considered for treatment of CDI in clinical practice, while data regarding other diseases is still insufficient and should be used only in research settings.
CDI
CDI is the leading cause of nosocomial diarrhea and its incidence is on the rise in the community as well in the past few decades. Commonly associated risk factors are antibiotic exposure, hospitalization, gastric acid suppressing medications and comorbidities such as immunocompromised states[28-30]. Since the pathophysiology of CDI mainly revolves around changes in the gut microbiome, hence FMT, by restoring the normal diversity and composition of the microbiota can conceivably prevent further infection[23]. There is some evidence to suggest that even host secretions or microbial metabolites alone, rather than the bacteria itself may be sufficient for treatment, as was seen when sterile stool filtrates transferred to recipients resulted in improvement of symptoms in five CDI patients[31].
Oral antibiotics are efficacious in over 85% patients with mild-moderate CDI,however the recurrence risk is 25% (up to 60% with subsequent recurrences)[32,33]. FMT is proving to be a novel and successful technique in treating CDI with numerous clinical trials having shown more than 85% cure[34,35]. With regard to CDI, FMT is indicated for preventing recurrences, treating refractory cases and possibly for primary CDI as well[36].
In the first open-label randomized controlled trial performed by van Nood et al[37],FMT was administered via nasoduodenal route for recurrent CDI which showed an 81% cure rate for patients who received FMT compared to only 31% resolution in patients treated with vancomycin alone. Higher cure rates of 92% were seen in patients with recurrent CDI who were given vancomycin combined with FMT (via colonoscopy/nasojejunal tube) than those who received fidaxomicin or vancomycin only, in a randomized controlled trial[38]. However, the overall cure rate was slightly lower (76.1%) in a systematic-review and meta-analysis of 13 clinical trials- with randomized trials demonstrating lower rates (67.7%) than open-label studies(82.7%)[34].
Some studies have shown promising results of FMT in treating refractory CDI. In one such study, 91% of CDI patients who were refractory to antibiotics, showed a positive response to FMT, the rate being100% for severe CDI and 87% for severecomplicated CDI[39]. Another study showed a cure rate of 75% with single FMT infusion and 100% with multiple FMT infusions for severe CDI refractory to antibiotics[40].
One small randomized clinical trial (RCT) compared the efficacy of FMT in treating 20 patients with acute primary CDI, against metronidazole[36]. The rates of sustained primary full response with no recurrence at day 70 were similar between them. This suggests a possible role of FMT as a therapeutic modality for managing the first episode of CDI. This being said, the fact that only metronidazole was studied here,must be taken into consideration, as it is now proven to be less effective than other first-line treatment options.
SCREENING AND SELECTION OF DONOR AND RECIPIENT
Donor
Careful screening and selection of the donor is a crucial step in FMT. However, the current evidence-based guidelines are not well established and raise uncertainty in terms of: whether the donor should be related to recipient vs household contact vs standard donor, frequency of screening of donors, and criteria for standard screening[41]. A systematic review showed a higher rate of resolution of CDI in FMT done with related donors (93.3% of studies) than with unrelated donors (84% of studies)[42], while another study conducted to assess donor type found no difference in clinical outcome when the donor was patient-selected versus anonymous[22]. In order to decrease the risk of transmitting the disease from donor to the recipient, and the risk of adverse events from the stool transfer, donor screening protocols have outlined exclusion criteria and testing for the donors (Table 1). A complete medical and social history is completed, including active infection, significant gastrointestinal (GI)illnesses (IBD, IBS, chronic diarrhea/constipation), history of autoimmune illnesses,allergy history, recent antibiotic use and hospitalization, recent travel, obesity,metabolic syndrome, anxiety, depression as well as detailed social risk assessment.This is done to identify any risk factors associated with conditions which have a disrupted microbiome. Subsequently, stool and blood testing for bacteria, viruses and parasites is done among the potential donors[43]. With the rapidly growing significance of FMT as a therapeutic method, it would be beneficial to standardize the protocols for donor selection, recruitment and screening in the long run.
Recipient
Currently, FMT is recommended for recurrent CDI with its use for other disease states still under investigation[44]. Potential microbiota transplant recipients include those with ≥ 3 CDI episodes, having a positive C. difficile stool assay and failed prior firstline treatments (vancomycin, metronidazole, or fidaxomicin). Sometimes, if CDI patients having refractory disease, moderate to severe in intensity, fail one week of oral vancomycin, they may be considered to receive FMT[43]. A pre-requisite is the recipient's ability to give consent for upper and lower GI endoscopy, undergo the procedure safely and ability to stop concomitant antibiotics as well as gastric acid suppressants. Although guidelines are not well established, it is recommended that recipients should be screened for infectious blood-borne diseases like viral hepatitis and human immunodeficiency virus[43]. In addition to this, one may consider screening the recipients in vulnerable populations such as immunocompromised patients to carefully balance the risks and benefits of FMT in them.
METHODS OF MICROBIAL REPLACEMENT THERAPY
FMT can be done via several routes - oral, nasogastric, nasojejunal, enema,colonoscopy or capsules, each having its own benefits and risks, with inconsistent reporting of use of specific methods[45]. Despite the widespread use of FMT as an effective therapeutic option, there is a concern about the lack of standardization of the process. There is heterogeneity at every stage: screening of the donor, type of donor(related vs unrelated), single stool sample vs pooled stool, site-specific donors vs stool banks, processing of stool as well as its quantity to be infused, whole stool vs enriched sample, fresh vs frozen vs lyophilized stool), number of doses of FMT and method of administration[45]. Ongoing research in this area has led to emergence of new data in terms of efficacy - lyophilized stool is inferior to fresh and frozen stool, which are both
equivalent[34,46,47]; lower GI routes are more efficacious than upper GI routes (95% and 88% respectively), while colonoscopy is better than one-time enema (87% and 66%respectively)[34,35,48,49]. In view of this wide variability, standardized microbiota replacement therapies are opening up a promising new avenue, which is superior with regard to decreased invasiveness and more regulation of the procedure.
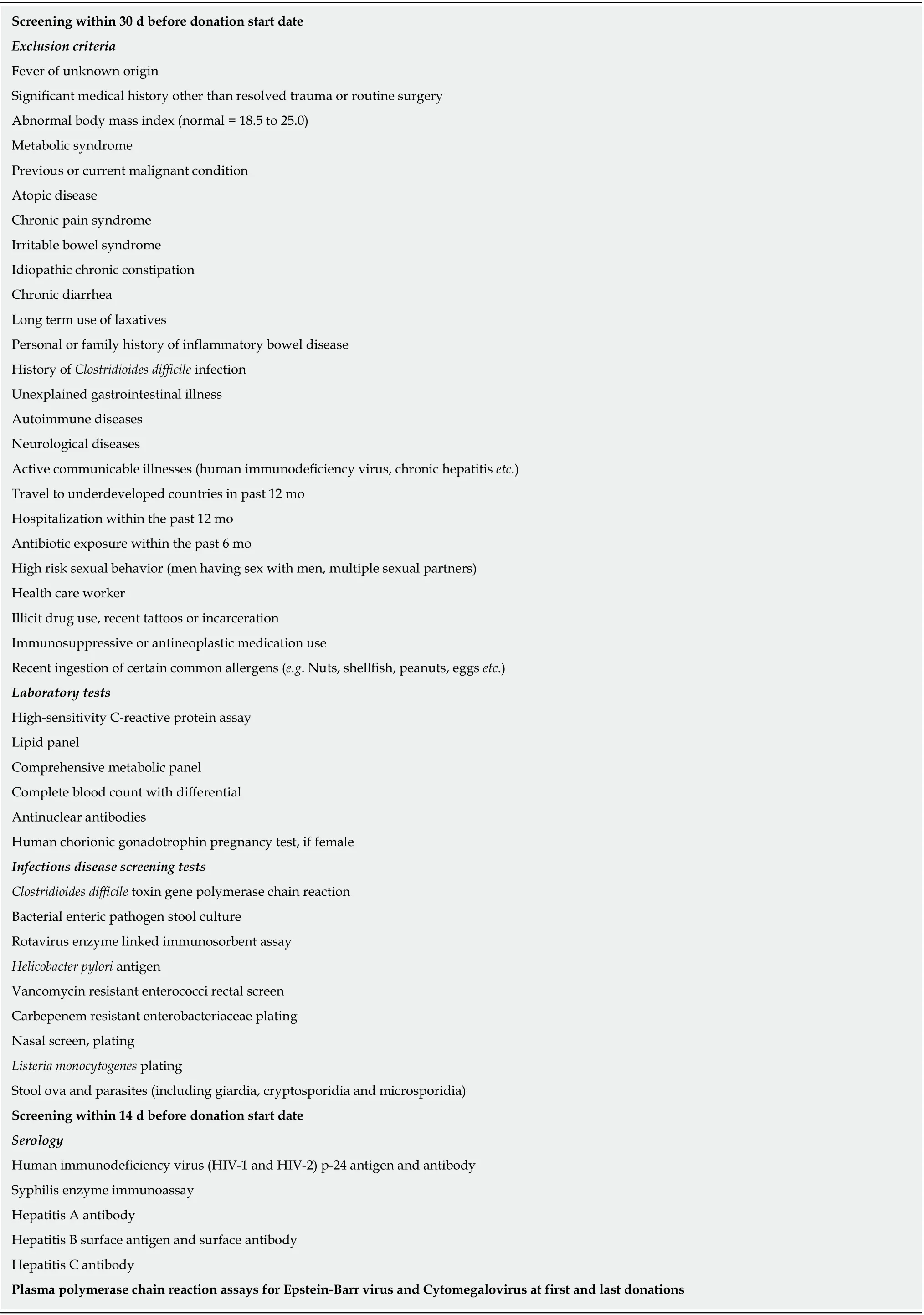
Table 1 Donor screening criteria[15,90]
The cost and logistics of setting up an infrastructure often limits availability of FMT. Standardized microbiota replacement therapies are an attractive alternative,potentially reducing the heterogeneity of product processing and administration as described above. A standardized product would potentially be widely available,without constraints related to infrastructure, logistics and economic considerations.
Several such products are currently undergoing clinical trials: (1) Enema-based microbiota replacement, RBX2660, a standardized stool-derived microbiota-based suspension (kept frozen, thawed before use and administered as an enema) is being studied in clinical trials. It underwent an open-label phase I trial which demonstrated safety and 87.1% efficacy. When given to recurrent CDI patients via enema, a single dose of RBX2660 showed superiority to placebo with efficacy of 67% compared to 46%, in the phase II study[50,51]. FMT administered by such enema-based methods is safe overall - with minimal transient gastrointestinal adverse events and no concerns for serious adverse events[50,51]. RBX2660 is currently undergoing Phase III trials; and(2) Capsule-based microbiota replacement. Capsule-based products are forms of oral FMT that are rapidly gaining popularity because they are less expensive, have fewer adverse events, and are easier to administer than microbiota replacement via endoscopy. An RCT showed oral capsules to be equally efficacious, but with a more favorable safety profile when compared to colonoscopy[52]. With a treatment response rate of 82% in CDI patients after a single treatment, and its subsequent rise to 91%with two treatments, oral capsules have demonstrated efficacy in 180 patients in an open label study[53]. Several such novel therapeutics are in the pipeline. SER-109, a frozen oral capsule, contains 50 species of Firmicutes spores derived from purified and enriched human stool specimens from healthy donors. Although its phase I trial showed some positive outcomes[54], SER-109 failed to demonstrate superiority to placebo in treating recurrent CDI in a phase II randomized double-blinded study.Phase III trials for SER-109 are in progress (Clinicaltrials.gov: NCT03183128). RBX7455 is a lyophilized oral capsule that is derived from stool, is non-frozen and stable at room temperature, and is currently being studied by Rebiotix, Inc. in a phase I clinical trial to assess safety (Clinicaltrials.gov: NCT02981316). There are also ongoing phase II placebo-controlled trials for CP101 (Finch therapeutics), an oral capsule defined as full spectrum microbiota. These aim to study the associated adverse events as well as see what proportion of CDI patients remain recurrence-free at 8 and 24 wk(Clinicaltrials.gov: NCT03110133).
SAFETY AND ADVERSE EVENTS
Based on current evidence, microbiota replacement is overall a safe therapy; with most adverse events (AEs) being minor, rarely associated with serious AEs[18,55,56]. A study reported that FMT administered via upper GI route had a higher frequency of minor AEs (43.6% vs 17.7%) as compared to lower GI route where serious AEs)occurred three times more frequently[57]. A 28.5% incidence rate of FMT associated AEs was reported in a meta-analysis, including 9.2% serious AEs; death (3.5%) and infection (2.5%) were rare. Typically, the associated adverse events are mild gastrointestinal symptoms like abdominal discomfort, nausea/vomiting (especially if FMT is administered orally), flatulence, or bloating. Endoscopy and sedation often account for the serious complications (e.g., bleeding, perforation, aspiration etc.).Although some individual reports of peripheral neuropathy, Sjogren syndrome,microscopic colitis, contact dermatitis, rheumatoid arthritis, and ulcerative colitis flare after FMT do exist, there is no proven causation[58-60]Recently, the Food and Drug Administration reported development of invasive infections caused by extendedspectrum beta-lactamase-producing Escherichia coli in two immunocompromised adults who received investigational FMT, resulting in the death of one individual. The donor stool that was administered to these 2 patients had not been tested for extended-spectrum beta-lactamase-producing bacteria prior to use and was later found to be positive. This raises concerns about the potential risk of serious or lifethreatening infections with the use of FMT and highlights the importance of donor screening. Despite the existing widespread literature on the efficacy of FMT, the scarcity of long-term safety data is a major concern. Thus, a long term follow-up registry has been set up by the American Gastroenterological Association for a comprehensive evaluation of the adverse events from FMT.
MICROBIAL REPLACEMENT FOR INDICATIONS OTHER THAN C. DIFFICILE
IBD
IBD is a chronic inflammatory gastrointestinal disorder wherein alteration of the microbiota in the GI tract is central to disease causation. A decrease in the populations of Bacteroides and Firmicutes, and an increase in Actinobacteria and Enterobacteriaceae contribute towards microbial dysbiosis in IBD[61]. A remission period, although variable in duration, can be induced by FMT in patients after failure of conventional IBD therapies, as was shown in studies by Borody and colleagues[62,63]. A systematic review by Coleman and Rubin demonstrated a higher response rate with FMT in CD(60.5%) than in UC (22%)[64]. A number of RCTs conducted to evaluate the efficacy of FMT in ulcerative colitis alone have shown equivocal results[65-67]. A plausible explanation for the less impressive outcomes of microbial replacement therapies in IBD could be the contribution of others factors towards disease exacerbation like impaired mucosal barrier function, inflammation, genetics and environmental factors[68]Additional, large scale randomized, double-blinded, placebo controlled studies are needed, and the current role of FMT in the treatment of IBD remains unclear. Another concern with FMT is the risk of an IBD flare. Early studies reported up to 25% with flares; however recent data suggest a much lower risk[69,70].
IBS
IBS characterized by chronic abdominal pain and altered bowel habits. It is postulated that altered gut microbiome may contribute to the development as well as exacerbation of IBS[71]. Studies have shown decrease in the microbial diversity in the gut of patients with IBS compared to the normal gut[72]. One study with 55 patients showed complete resolution of symptoms in 36% patients of IBS undergoing FMT[62]while another small uncontrolled study of 13 patients demonstrated symptomatic improvement in 70% patients[73]. However, data on efficacy of FMT in IBS is still inconsistent and larger RCTs are required to before such therapy can be used in clinical practice.
Metabolic diseases
An area of increasing interest is the role of FMT in obesity and metabolic syndrome.Animal as well as human studies have suggested that gut microbiome plays a role in regulating energy homeostasis[74]. This was evident in several studies on mice -outcomes of weight gain and increased insulin resistance despite reduced intake were seen in germ free mice who received stool from conventionally raised mice[75]. FMT from obese donor mice resulted in more weight gain than from lean donors in germfree mouse models in another study[76]. One study demonstrated a transient increase in peripheral insulin sensitivity in obese patients who received FMT from lean unaffected donors, with an increase in butyrate-producing bacteria[77].
There is some evidence of the association between dysbiotic gut microbiome and liver diseases like non-alcohol fatty liver disease, alcoholic liver disease and hepatic encephalopathy. A small number of animal and human studies have shown mixed results regarding the usefulness of microbial replacement therapies in the management of these conditions[78-80]. This calls for additional, large scale, RCTs in this field.
There are several other conditions under investigation where FMT could have a potential role in treatment. In one study FMT was successful in eradicating vancomycin-resistant enterococci in almost three-quarters of vancomycin-resistant enterococci-positive patients with recurrent CDI[81]. Safety and efficacy of FMT in eradication of multi-drug resistant organisms from the gastrointestinal tract of patients with blood disorders has also been seen in a previous study[82]. FMT has been shown to decrease the frequency of recurrent urinary tract infections in patients with CDI and improve the antibiotic resistance patterns in subsequent urinary tract infections causing pathogens[83]. Other possible, less well studied indications for FMT applications include autism, fibromyalgia, myoclonus dystonia, multiple sclerosis,Parkinson disease and idiopathic thrombocytopenic purpura[84-88].
THE FUTURE
Microbiota replacement therapies are gaining popularity as a treatment option for diseases with an altered gut microbiome. However, there are several aspects of FMT that need to be further investigated before it can be incorporated as the standard of care. Currently, FMT for indications other than CDI should be performed only in research settings. Although it is known that microbial dysbiosis is associated with a number of infectious and non-infectious conditions other than CDI, the question is whether it is implicated in causation of disease, or is a result of the underlying disease state. Moreover our understanding of the exact nature and timing of the perturbation of the gut microbiota in such conditions is still limited. When microbial dysbiosis is triggered in an individual with predisposing factors (genetic/environmental), the subsequent host-microbiota interactions that take place are abnormal. These then contribute towards exacerbation of the underlying disease, as is evident in IBD,setting up a vicious cycle. Microbiota restoration therapies remain a major challenge,which need to be explored in-depth for these conditions, in order to control the underlying disease or to regulate the host-microbiota interactions. Several clinical trials in this field are underway. A major concern that makes the study of FMT in these conditions more complicated is that unlike CDI, where there is no donor or stool preparation effect on FMT success rates, the effectiveness and possibly the safety of microbial replacement in disease states other than CDI will probably be influenced by the type of donor , underlying disease status, other treatments the patient is receiving,pre-procedure bowel preparation and antibiotics, as well as by how the stool is processed and delivered. This was seen in IBD and hepatic encephalopathy where the success of FMT was influenced by donor effect[64,79]. Moreover, there is a need to define precise endpoints and follow up for these therapies for non-CDI indications.
With the ongoing interest in the broader applications of FMT there is a need to define standardized guidelines for donor screening and recruitment. The goal is to minimize safety risks from transfer of stool from potentially healthy donors to patients. With regard to donor screening for FMT in non-CDI indications, areas that should specifically be assessed for include microbial richness, diversity and metabolite production. Furthermore, it is essential to understand how related vs unrelated donors affect the outcomes of microbial restoration therapies with more research in this field. Maintenance of stool banks, donor compensation and cost of donor screening are other questions that still remain to be answered. There are several factors that need to be taken into account while considering a recipient for FMT in non-CDI indications: pre-procedure disease severity, bowel preparation, administering antibiotics like rifaximin or changing concomitant medications, as well as the timing and ultimate goal of treatment (inducing remission vs maintaining it vs preventing flares). Further studies are required to elucidate the dosing frequency of FMT and to find out whether microbial restoration has the potential to become the stand-alone standard of care or can it be used only as an adjunctive form of treatment for diseases.
Microbiota replacement therapies are overall a relatively safe procedure as has been described previously, with few, mild adverse events. However, data on the long term outcomes related to changes in the microbiome, and its safety profile in the long run is lacking. A complete evaluation of FMT complications will require ongoing,prospective studies.
In the future, there may be a possibility to individualize microbial replacement therapies to patients and conditions, and there may be opportunities for donor-recipient matching or defined microbial consortia for FMT. With expanding knowledge of host-microbiota interactions, therapies maybe tailor made such that they are based upon the deficits or excess of specific microbial taxa (bacterial, viral or fungal) in patients, which would ultimately be a more effective mode of treatment.There is also a question about the efficacy of using alternatives to donor stools, such as synthetic stool formulations or live bacterial products generated in vitro by fermentation, for administration to patients to prevent or treat specific diseases. These novel therapies are called biotherapeutics. There are several preparations (SER-262,NTCD-M3, VE303) currently undergoing clinical trials, and have immense potential as treatment options in the future[89].
CONCLUSION
Alterations in gut microbiota are central to the pathogenesis of several diseases.Manipulation of this microbial dysbiosis to restore balance by microbial replacement therapies has been effective in treating CDI and is being explored for patients with other conditions as well. The role of FMT for these non-CDI indications is currently limited to research settings. As our understanding of the interaction between human health and microbiota increases, there is immense potential for microbial replacement therapies to emerge as standardized treatments for patient care in the future.
 World Journal of Gastroenterology2020年8期
World Journal of Gastroenterology2020年8期
- World Journal of Gastroenterology的其它文章
- Promising key genes associated with tumor microenvironments and prognosis of hepatocellular carcinoma
- Downregulation of orosomucoid 2 acts as a prognostic factor associated with cancer-promoting pathways in liver cancer
- Neoadjuvant chemotherapy vs upfront surgery for gastric signet ring cell carcinoma: A retrospective,propensity score-matched study
- Haemoglobin, albumin, lymphocyte and platelet predicts postoperative survival in pancreatic cancer
- Prognostic value of preoperative weight loss-adjusted body mass index on survival after esophagectomy for esophageal squamous cell carcinoma
- Diverting colostomy is an effective and reversible option for severe hemorrhagic radiation proctopathy
