由甲状旁腺癌引发甲状旁腺功能亢进症患者的术前预测因子价值分析
孙芸 沈林强 付晓瑾 高丹丹
[摘要] 目的 探讨由甲状旁腺癌(PC)引发甲状旁腺功能亢进症(PHPT)患者的术前预测因子价值,为PC的早期诊断提供理论和临床依据。 方法 选取2014年5月~2018年3月我院收治的原发性PHPT患者135例,经实验室检查和手术病理证实,96例为甲状旁腺腺瘤(PA),23例为甲状旁腺增生(PH),16例为PC。比较PA组患者与PC组患者的临床特征,并使用受试者工作特征(ROC)曲线对PC的术前预测因子进行分析。 结果 PC组患者血钙、血清校正钙、PTH、AKP和CRE水平均高于PA组患者(P<0.05);PC组患者肿瘤直径更大(P<0.05)。两组患者其余临床特征比较,差异无统计学意义(P>0.05)。PC与血清校正钙(r=0.335,P=0.000)、PTH(r=0.305,P=0.001)、AKP(r=0.225,P=0.017)和肿瘤直径(r=0.248,P=0.009)相关。血清校正钙诊断阈值为3.20 mmol/L,AUC为0.721,约登指数为0.446;PTH诊断阈值为958.00 pg/mL,AUC为0.786,约登指数为0.421;AKP诊断阈值为55.70 IU/L,AUC为0.741,约登指数为0.709;肿瘤直径诊断阈值为3.20 cm,AUC为0.689,约登指数为0.361。 结论 与PA患者相比,PC患者的血清校正钙、AKP和PTH水平更高、肿瘤直径更大。ROC曲线分析显示,使用血清校正钙、AKP、PTH和肿瘤直径在术前对PC进行预测,具有一定临床价值,其中又以AKP预测的约登指数最高,PTH预测的AUC最大。
[关键词] 甲状旁腺功能亢进症;甲状旁腺癌;甲状旁腺素;碱性磷酸酶
[中图分类号] R736.2 [文献标识码] B [文章編号] 1673-9701(2020)34-0064-04
[Abstract] Objective To investigate the value of preoperative predictors in patients with primary hyperparathyroidism(PHPT) caused by parathyroid cancer(PC), and to provide theoretical and clinical basis for early diagnosis of PC. Methods A total of 135 patients with PHPT admitted to our hospital from May 2014 to March 2018 were selected. After laboratory examination and surgical pathology, a total of 96 cases were parathyroid adenoma(PA), 23 cases were hyperparathyroidism(PH) and 16 cases were PC. The clinical features of patients in the PA group and the PC group were compared, and the preoperative predictors of PC were analyzed by receiver operating characteristic(ROC) curve. Results The levels of serum calcium, serum adjusted calcium, PTH, AKP and CRE in the PC group were higher than those in the PA group(P<0.05). In addition, the tumor diameter in the PC group was larger(P<0.05). There was no statistically significant differences in other clinical features between the two groups(P>0.05). PC was correlated with serum adjusted calcium(r=0.335, P=0.000), PTH(r=0.305, P=0.001), AKP(r=0.225, P=0.017) and tumor diameter(r=0.248, P=0.009). The diagnostic threshold of serum adjusted calcium was 3.20 mmol/L, AUC was 0.721, and the Youden's index was 0.446. The diagnostic threshold of PTH was 958.00 pg/mL, AUC was 0.786, and the Youden's index was 0.421. The diagnostic threshold of AKP was 55.70 IU/L, AUC was 0.741, and the Youden's index was 0.709. And the diagnostic threshold of tumor diameter was 3.20 cm, AUC was 0.689, and the Youden's index was 0.361. Conclusion Compared with the PA patients, the PC patients have higher serum adjusted calcium, the AKP and PTH levels and larger tumor diameter. ROC curve analysis shows that serum adjusted calcium, AKP, PTH and tumor diameter have a certain clinical value in predicting PC before operation. Among them, and the Youden's index predicted by AKP is the highest, and the AUC predicted by PTH is the largest.
[Key words] Primary hyperparathyroidism; Parathyroid carcinoma; Parathyroid hormone; Alkaline phosphatase
甲状旁腺功能亢进症(Primary hyperparathyroidism,PHPT)一般表现为由骨吸收增高引起的骨骼病变、低磷血症、高钙血症或肾石病[1],但某些早期或轻型病例可仅表现为个别生化异常或完全无症状[2]。在西方国家,PHPT已被视为继甲状腺功能亢进症和糖尿病后的第三大内分泌疾病,而在我国,虽然该病的发病率较国外偏低,但近年来也有增高的趋势[3]。甲状旁腺癌(Parathyroid carcinoma,PC)尽管不是PHPT的常见病因,但因其组织学鉴别困难,约50%甲状旁腺癌患者出现远处转移后才被确诊,故提高对PC的认识,探寻能够有效、早期预测PC的因子,对降低PC导致PHPT患者的临床漏诊、误诊率具有重要意义[4]。本研究选取2014年5月~2018年3月我院收治的原发性PHPT患者135例,利用受试者工作特征曲线研究不同预测因子对PC的术前诊断价值,现报道如下。
1 资料与方法
1.1一般资料
选取2014年5月~2018年3月我院收治的原发性PHPT患者135例,其中男29例,女106例;年龄24~67岁,平均(47.5±10.5)岁。135例患者中,42例有高血压史,7例有冠心病史,18例有糖尿病史。纳入标准:①根据诊断标准[5]确诊为原发性甲状旁腺功能亢进症,合并皮肤瘙痒、骨关节痛、肌无力等临床症状;②全段甲状旁腺激素(iPTH)达到正常范围上限10倍以上(>620 pg/mL);③PC患者經病理诊断,合并甲状旁腺肿瘤侵犯血管、侵犯神经、侵袭邻近结构或淋巴结、远处转移之一的病理特征;④签署知情同意书。排除标准[6]:①经病理确诊为甲状旁腺增生;②合并重要脏器器质性病变;③合并精神类疾病,无法配合研究。经医院医学伦理委员会批准,将96例PA患者和16例PC患者纳入研究。PA组患者中,男19例,女77例;平均年龄(47.3±11.1)岁;84例患者接受血液透析(He-modialysis,HD),12例接受腹膜透析(Peritoneal dialysis,PD),透析龄46~121个月,平均(78.4±20.8)个月。PC组患者中,男4例,女12例;平均年龄(47.7±8.4)岁;14例患者接受HD,2例接受PD,透析龄42~118个月,平均(82.4±25.4)个月。两组一般资料比较,差异无统计学意义(P>0.05),具有可比性。
1.2 方法
两组患者均禁食、禁水12 h。第2天8:00抽取空腹静脉血20 mL,同时留尿,使用日立全自动7600生化分析仪(日本日立公司)对血磷(Serum phosphate,SP)、血钙(Serum calcium)、甲状旁腺素(Parathyroid hormone,PTH)、尿素氮(Blood urea nitrogen,BUN)、谷丙转氨酶(Aspartate aminotransferase,ALT)、谷草转氨酶(Alanine aminotransferase,AST)、尿酸(Uric acid,UA)、血肌酐(Blood creatinine,CRE)、碱性磷酸酶(Alkaline phosphatase,AKP)和24 h尿钙(24-hour urinary calcium,24 h-UC)进行检验测定。使用同时校正法(Simultaneously correction procedures,SC)计算血清校正钙。
1.3 统计学方法
数据应用SPSS20.1统计学软件进行分析,符合正态分布的计量资料用(x±s)表示,采用t检验;不符合正态分布的计量资料用M(P25,P75)表示,采用Mann-Whitney U检验;计数资料用[n(%)]表示,采用χ2检验;采用Spearman法进行相关性分析,采用ROC曲线对预测价值进行分析,P<0.05为差异有统计学意义。
2 结果
2.1 两组患者各项临床特征比较
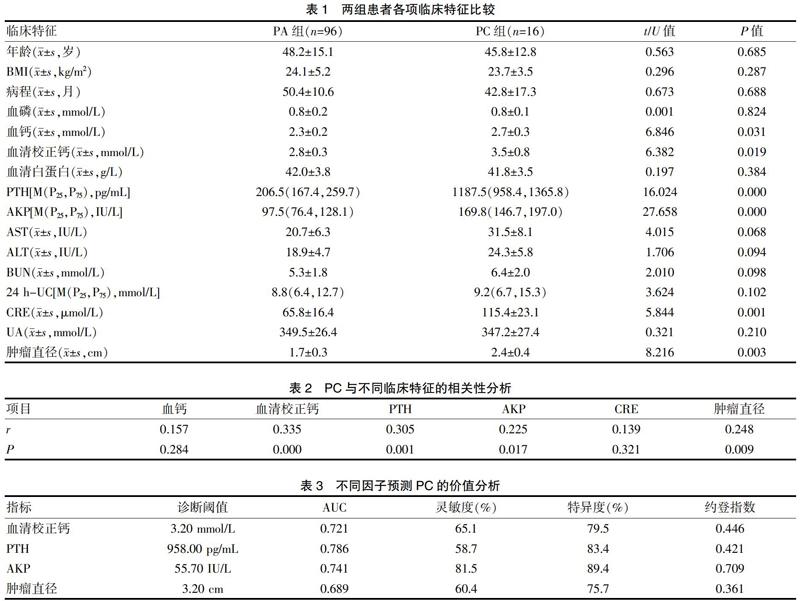
两组患者各项临床特征比较结果显示,PC组患者血钙、血清校正钙、PTH、AKP和CRE水平均高于PA组患者,PC组患者肿瘤直径更大,差异有统计学意义(P<0.05)。见表1。
2.2 PC与不同临床特征的相关性分析
将上述两组患者比较差异有统计学意义的6项因子(血钙、血清校正钙、PTH、AKP、CRE和肿瘤直径)与PC进行Spearman相关分析,结果显示PC与血清校正钙、PTH、AKP和肿瘤直径相关,而与血钙、CRE的相关性无统计学意义。见表2。
2.3 不同因子预测PC的价值分析
使用ROC曲线分析血清校正钙、PTH、AKP和肿瘤直径4种因子对PC的术前预测价值。见封三图4、表3。
3讨论
PHPT的病理类型可分为甲状旁腺增生、PA和PC,其中以PA最为常见[7]。有研究显示,PHPT患者中,甲状旁腺增生的比例占1.18%~24.17%,PA的比例占71.17%~98.63%,PC的比例占3.1%~12.53%[8]。PC尽管不是PHPT的常见病因,但因其组织学鉴别困难,约50% PC患者出现远处转移后才被确诊。由于良性PHPT与恶性疾病鉴别的困难性,临床医师往往在患者出现反复发生的顽固性高钙血症,甚至PTH依赖性高钙血症时,才会考虑PC的可能。在疾病早期,PC患者缺乏特异度高的临床症状、实验室检查及影像学检查,细针穿刺抽吸组织学检查的准确度也不尽人意。国外有研究显示,近年来PC的发病率呈明显增高趋势[9]。本研究中,经手术病理证实的135例PHPT患者中,甲状旁腺增生为23例(17.04%),PC为16例(11.85%),PA为96例(71.11%),与上述研究结果基本一致。
相较于甲状旁腺的良性疾病,PC发病率低,临床表现多样,包括恶心、呕吐、病理性骨折、尿路结石、骨关节痛甚至精神躁狂或抑郁,其特点不明显,故诊断和治疗有难度[10]。目前,PC最好的治疗方法是在早期完整切除原发性肿瘤,但该类患者预后易受术前和术中医师判断的影响,故医师在术前和术中的诊断尤其重要。关于PC的预后因素和分期系统目前尚存争议[11]。影像学检查、实验室检查结合临床特点是识别PC的常用手段。美国学者通过分析癌症数据库资料发现,PC患者年龄在15~89岁之间,中位年龄57岁[12]。本研究中,PC患者平均年龄为(51.8±3.8)岁,与上述研究结果相近。有报道称,PC患者PTH水平增高明显[13],本研究中的PC患者术前PTH水平为1187.2 pg/mL,显著高于PA患者。还有相关研究显示,PC患者血清校正钙水平为1.77~3.83 mmol/L[14],本研究中PC患者术前血清校正钙为(3.5±0.8)mmol/L,与上述研究结果相符。另有研究结果显示,PC患者肿瘤直径为2.5~5.4 cm[15],本研究结果为1.8~5.4 cm,符合上述研究。此外,本研究中PC患者的AKP水平有所增高这一结果亦与其他相关文献报道相符[16]。
研究结果显示,PHPT患者的AKP水平和甲状腺病变的大小可能成为PC的预测因子[16-17],甲状旁腺病变直径为3.0 cm和AKP水平为285 IU/L分别为该因子的最佳截点值。回顾性分析结果显示,甲状旁腺病变直径>1.5 cm可帮助诊断PC[18]。本研究结果显示,PC与患者的肿瘤直径、PTH、血清校正钙、AKP有关。血清校正钙3.20 mmol/L是最佳截点值,与国外学者的研究结果相似[17-20]。PTH诊断PC的灵敏度和特异度分别为58.7%和83.4%,AKP诊断PC的灵敏度和特异度分别为81.5%和89.4%。
综上所述,与PA患者相比,PC患者的血清校正钙、AKP和PTH水平均更高,肿瘤直径更大,ROC曲线分析显示,使用血清校正钙、AKP、PTH和肿瘤直径在术前对PC进行预测具有一定临床价值,其中又以AKP预测的约登指数最高,PTH预测的AUC最大。下一步可考虑将AKP和PTH水平进行联合检测以分析其术前预测价值,还有待于大样本多中心研究。
[参考文献]
[1] Guerin C,Paladino NC,Lowery A,et al.Persistent and recurrent hyperparathyroidism[J].Updates in Surgery,2017, 69(2):161-169.
[2] Eidman KE,Wetmore JB.Managing hyperparathyroidism in hemodialysis:Role of etelcalcetide[J].Int J Nephrol Renovasc Dis,2018,17(11):69-80.
[3] Brabyn P,Capote A,Belloti M,et al.Hyperparathyroidism diagnosed due to brown tumors of the jaw:A case report and literature review[J].Journal of Oral & Maxillofacial Surgery,2017,75(10):S0278 239 117 303 312.
[4] Okada M,Tominaga Y,Hiramitsu T,et al.Development of severe hyperparathyroidism despite short-term renal replacement therapy[J].World Journal of Surgery,2018,42(2):425-430.
[5] 中华医学会内分泌分会代谢性骨病学组.原發性甲状旁腺功能亢进症诊疗指南[J].中华骨质疏松和骨矿盐疾病杂志,2014,16(3):187-198.
[6] Plas WYVD,Engelsman AF,zyilmaz A,et al.Impact of the introduction of calcimimetics on timing of parathyroidectomy in secondary and tertiary hyperparathyroidism[J].Annals of Surgical Oncology,2017,24(1):15-22.
[7] Guarnieri V,Seaberg RM,Kelly C,et al.Erratum to:Large intragenic deletion of CDC73(exons 4-10) in a three-generation hyperparathyroidism-jaw tumor(HPT-JT) syndrome family[J].Bmc Medical Genetics,2017,18(1):99.
[8] Magorzata K,Pazińska MT,Witold C,et al.Comparison of scintigraphy and ultrasound imaging in patients with primary,secondary and tertiary hyperparathyroidism-own experience[J].Journal of Ultrasonography,2017,17(68):17-22.
[9] Dale AG,Holbrook BD,Sobel L,et al.Hyperparathyroidism in pregnancy leading to pancreatitis and preeclampsia with severe features[J].Case Reports in Obstetrics and Gynecology,2017,2017(3):1-3.
[10] Tsvetov G,Hirsch D,Shimon I,et al.Thiazide treatment in primary hyperparathyroidism-a new indication for an old medication?[J].J Clin Endocrinol Metab,2017,102(4):1270-1276.
[11] Kageyama K,Ishigame N,Sugiyama A,et al.A case of hyperparathyroidism due to a large intrathyroid parathyroid adenoma with recurrent episodes of acute pancreatitis[J].Case Reports in Endocrinology,2017,2017(4):1-5.
[12] Yuan L,Liu J,Kan Y,et al.The diagnostic value of 11C-methionine PET in hyperparathyroidism with negative 99mTc-MIBI SPECT:A meta-analysis[J].Acta Radiologica,2017,58(5):558-564.
[13] Idrees SM,Khan M,Humayun M,et al.Multiple osteosclerotic lesions:A rare presentation of hyperparathyroidism secondary to hypovitaminosis D[J].Journal of the College of Physicians and Surgeons-Pakistan:JCPSP,2017, 27(9):S80.
[14] Guerin C,Romanet P,Taieb D,et al.Looking beyond the thyroid:Advances in understanding of pheochromocytoma and hyperparathyroidism phenotypes in MEN2 and of non-MEN2 familial forms[J].Endocrine-Related Cancer,2017,25(2):535.
[15] Pradeep PV,Srikanth BR.Comment on:Eucalcemic parathyroid hormone elevation after parathyroidectomy for primary sporadic hyperparathyroidism:Risk factors,trend,and outcome[J].Annals of Surgical Oncology,2017, 24(3):1.
[16] 胡亞,廖泉.甲状旁腺癌分子机制研究现状及临床应用前景[J].中华内分泌代谢杂志,2020,36(6):537-540.
[17] 陈思行,孔晶,王鸥,等.以反酸、腹泻、腰痛为表现的甲状旁腺癌一例报道[J].中华内分泌代谢杂志,2019,35(4):341-344.
[18] 姚晓爱,姜涛,魏伯俊,等.甲状旁腺癌的临床特征和术前预测因子分析[J].中华肿瘤杂志,2018,40(6):428-432.
[19] Palla B,Burian E,Fliefel R,et al.Systematic review of oral manifestations related to hyperparathyroidism[J].Clinical Oral Investigations,2017,22(10):1-27.
[20] Assimos DG.Thiazide treatment in primary hyperparathyroidism-A new indication for an old medication?[J].Journal of Urology,2017,198(1):138.
(收稿日期:2020-07-06)

