髓内钉与锁定钢板治疗胫骨AO42-C型骨折的对比研究
焦玉爽 杜红杰 张宗召


【摘要】目的 比较采用髓内钉技术和锁定钢板技术治疗胫骨AO 42-C型骨折的疗效差异。方法 将55例胫骨骨折患者分为髓内钉组(29例)及锁定钢板组(26例),术中分别采用髓内钉及锁定钢板作为内固定物,比较2组手术及并发症情况,使用Johner-Wruhs评分评价手术疗效。 结果 所有患者手术过程顺利。髓内钉组浅表感染、下肢疼痛发生率均低于锁定钢板组(P均< 0.05)。髓内钉组畸形发生率高于锁定钢板组(P < 0.05)。髓内钉组Johner-Wruhs评分优于锁定钢板组(P < 0.05)。2组骨折愈合时间、剧烈活动受限及发生步态改变的情况比较差异均无统计学意义(P均> 0.05)。结论 采用髓内钉技术治疗胫骨AO 42-C型骨折在降低术后浅表感染、下肢疼痛发生率及提高Johner-Wruhs评分等方面优于锁定钢板技术。
【关键词】胫骨;骨折;髓内钉;锁定钢板
【Abstract】Objective To compare the clinical efficacy of intramedullary nail (IMN) and locking compression plate (LCP) fixation in the treatment of AO 42-C tibial fracture. Methods Fifty-five patients with complex tibial fractures were enrolled and allocated into the IMN (n = 29) and LCP groups (n = 26). Intraoperatively, IMN and LCP were utilized for internal fixation. Surgical conditions and postoperative complications were statistically compared between two groups. Surgical efficacy was assessed by Johner-Wruhs evaluation criteria. Results All patients successfully completed the surgery. In the IMN group, the incidence rate of superficial infection and lower limb pain was significantly lower, the incidence rate of deformation was remarkably higher, and the Johner-Wruhs evaluation score was considerably higher compared with those in the ICP group (all P < 0.05). The fracture healing time, severe activity limitation and gait changes did not significantly differ between two groups (all P > 0.05). Conclusion IMN is superior to LCP fixation with a lower incidence of superficial infection and lower limb pain, and higher Johner-Wruhs evaluation score in the treatment of AO 42-C fracture.
【Key words】Tibia;Fracture;Intramedullary nailing;Locking compression plate
脛骨干骨折在临床中较为常见,其发病率约为0.6%[1]。目前临床中常选择胫骨髓内钉或锁定钢板进行固定。对于胫骨AO 42-A、B型骨折(胫骨干简单骨折),多数学者认为髓内钉固定优于锁定钢板固定,而对于胫骨AO 42-C型骨折(胫骨干粉碎性骨折),由于复位困难,采用髓内钉固定后骨折部位常遗留不同程度的短缩、成角畸形,造成术后双下肢不等长及下肢力线改变[2-4]。因此,对于胫骨AO 42-C型骨折,选择何种内固定系统仍是术者所要慎重思考的问题,但笔者见目前相关的研究较少,故拟对髓内钉和锁定钢板技术治疗胫骨AO 42-C型骨折术后患肢功能恢复与并发症情况进行研究,以比较2种内固定物的疗效差异,从而为临床决策提供指导。
对象与方法
一、研究对象
本研究选择2016年1月至2019年1月在我院就诊的胫骨骨折患者。纳入标准:①年龄> 16岁;②AO骨折分型为42-C型骨折;③同意行胫骨髓内钉或锁定钢板治疗。排除标准:①严重的开放骨折;②并发相邻关节及股骨、足部骨折或大面积软组织损伤;③合并糖尿病等严重内科疾病;④患有神经肌肉系统疾病;⑤病理性骨折或二次骨折。所有患者对手术知情同意,并签署知情同意书。
将患者分为髓内钉组和锁定钢板组。经筛查,最终纳入55例患者。髓内钉组29例(1例合并尺骨鹰嘴骨折,2例合并掌骨骨折),其中男20例、女9例,年龄41.0(33.5,49.5)岁,受伤至手术平均时间为5.0 (4.0,6.0)d;锁定钢板组26例(1例合并肱骨骨折),其中男20例、女6例,年龄40.0 (32.5,46.8)岁,受伤至手术平均时间为6.0(4.8,7.0)d,上述资料2组比较差异均无统计学意义(P均> 0.05)。
二、方 法
1.术前准备
本研究所纳入的患者入院后均接受常规术前检查和抗凝、消肿等治疗,并行跟骨牵引以纠正下肢长度及力线。待患者基本状况及皮肤条件允许后行手术治疗。
2.手术方法
2组均采用硬膜外阻滞。髓内钉组沿髌韧带正中切开髌韧带。在C型臂X光机透视下行手法复位骨折后,依次钻入导针,开口器手动开口。插入金手指至骨折端,顺入导丝。在C型臂X光机透视下测量患肢髓腔长度及直径,选择合适型号主钉,并扩髓直至大于主钉直径1 mm。沿导丝插入主钉,透视见成角及旋转畸形得到纠正后,分别锁定远、近端横行锁钉及尾帽。冲洗、修复髌韧带并缝合切口。锁定钢板组采用前外侧或前内侧入路切开皮肤,分离软组织暴露骨折端。复位骨折块后使用克氏针临时固定骨折块。根据骨折情况选择合适的锁定钢板,于骨膜上建立软组织隧道。插入锁定钢板,使用持骨器维持钢板位置。经C型臂X光机透视见钢板长度及位置满意后,在骨折两端分别打入3 ~ 4枚锁定螺钉。冲洗切口后,逐层缝合切口。
3. 术后处理
患者术后第2日开始功能锻炼并限制负重,术后1个月依据耐受情况开始逐渐增加负重活动直至完全负重。术后观察手术切口有无红肿、渗出等浅表感染。嘱患者门诊随访骨折愈合情况、患肢功能及皮肤有无窦道、脓肿等深部感染,直至骨折愈合。
4. 疗效评价
我们将X线检查观察到大于50%的骨痂通过骨折线定义为愈合[5]。根据FDA标准,将在9个月后仍未愈合的骨折定义为骨不连。最后1次隨访时使用Johner-Wruhs评分,从是否存在骨折不愈合、是否存在感染及血管神经损伤、是否存在畸形及患肢活动度等方面评估患肢的功能恢复及并发症,按由优到劣,将其分为优、良、中、差[6]。Johner-Wruhs评分标准见表1。
三、统计学处理
应用SPSS 19.0处理数据。正态分布计量资料采用表示,组间比较采用独立样本t检验;非正态分布计量资料采用中位数(下四分位数,上四分位数)表示,组间比较采用Wilcoxon秩和检验。计数资料用例(%)表示,其中无序分类资料的组间比较采用χ2检验,等级资料的组间比较采用Wilcoxon秩和检验。P < 0.05为差异有统计学意义。
结果
一、髓内钉组与锁定钢板组手术一般情况及愈合情况比较
所有患者手术顺利,髓内钉组骨折愈合时间为(18.2±3.3) 周。锁定钢板组有1例发生骨不连,行自体髂骨植骨后愈合,其余患者骨折愈合时间为(19.5±5.0)周,2组骨折愈合时间比较差异无统计学意义(P > 0.05),见图1。
二、髓内钉组与锁定钢板组手术相关并发症比较
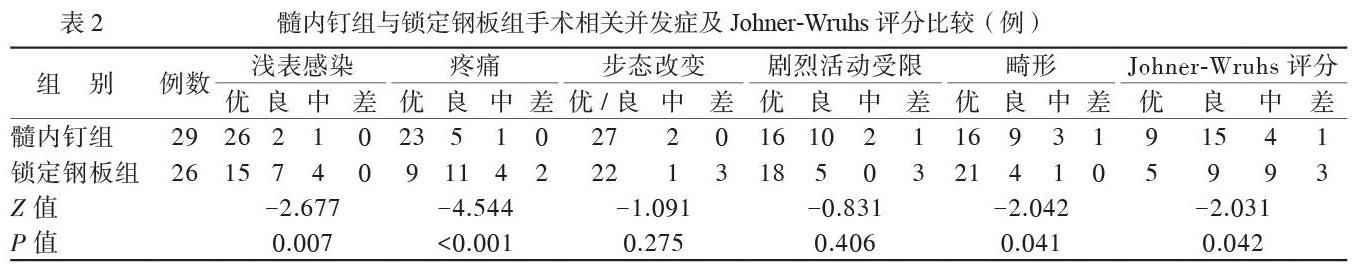
髓内钉组2例(6.9%)出现切口红肿、渗出等轻度感染,1例(3.4%)出现切口局部皮缘发黑,为中度皮肤感染;锁定钢板组7例(26.9%)出现轻度感染,4例(15.4%)出现中度皮肤感染,经抗炎、换药等治疗后所有患者切口均顺利愈合,并按时拆线。髓内钉组中5例(17.2%)出现轻度膝关节疼痛,1例为中度(3.4%);锁定钢板组中11例(42.3%)切口瘢痕处出现轻度疼痛不适,4例(15.4%)出现内固定物刺激导致的中度疼痛,2例(7.7%)患者疼痛较重。髓内钉组浅表感染、下肢疼痛发生率均低于锁定钢板组(P均< 0.05)。髓内钉组中13例(44.8%)可见胫骨畸形,锁定钢板组有5例(19.2%),前者畸形发生率高于后者(P < 0.05)。髓内钉组2例(6.9%)发生步态改变,13例(44.8%)出现不同程度剧烈活动受限;锁定钢板组4例(15.4%)发生步态改变,8例(30.8%)出现剧烈活动受限,2组比较差异均无统计学意义(P均> 0.05),见表2。
三、髓内钉组与锁定钢板组Johner-Wruhs评分比较髓内钉组Johner-Wruhs评分优于锁定钢板组(P < 0.05),见表2。
讨论
髓内钉和钢板固定是目前治疗胫骨AO 42-C型骨折的2种重要内固定方式,然而两者术后效果孰优孰劣,仍存在较大争议[7-11]。本研究拟分析采用髓内钉与锁定钢板内固定治疗胫骨AO 42-C型骨折的效果,以初步探究胫骨AO 42-C型骨折的最佳固定方式。
胫骨AO 42-C型骨折多为高能量损伤所致,常伴有下肢皮肤软组织不同程度的损伤,骨折周围的手术切口可造成皮肤及其血供的进一步破坏,大大增加浅表感染、骨不连、骨髓炎等并发症的发生[12-14]。本研究中髓内钉组的感染率低于锁定钢板组,术后下肢疼痛发生率也低于锁定钢板组。髓内钉内固定的术后下肢疼痛多由术中操作不当及内固定物对髌韧带及髌前脂肪垫等软组织的刺激所致,故术者在手术操作时应注意使用软组织保护套,并选择合适长度的髓内钉,以减少术后下肢疼痛的发生率[15]。
本研究显示2组患者骨折的愈合时间虽无统计学差异,但相比锁定钢板组,髓内钉组仍显示出骨折愈合时间缩短的倾向,Foux等[16]也提出了相关的理论支持。骨折的愈合受多方面因素影响,其中内固定物的刚度为重要因素[17-18]。锁定钢板虽然可提供维持骨折复位所需的强度,但其刚度远远大于骨组织,会产生应力遮挡效应,降低断端之间的应力刺激[19]。髓内钉中轴线弹性固定可提高其抗折弯、抗旋转的能力,能更有效地将应力载荷转移至骨折断端,为骨痂的生成提供了适度的应力刺激[20]。
曾有研究显示髓内钉维持骨折复位的能力比锁定钢板弱,术后骨折移位风险较大[21]。然而有研究显示,随着髓内钉技术的发展,髓内钉维持骨折复位的能力甚至已经超过了锁定钢板[7, 22]。虽然有研究者发现采用髓内钉固定患者术后下肢畸形率高于采用锁定钢板固定者,但其并未发生明显骨折复位丢失,且在步态及剧烈活动等方面其效果与后者无差异[7, 22]。
綜上所述,采用髓内钉技术治疗胫骨AO 42-C型骨折在降低术后浅表感染、减轻下肢疼痛及提高Johner-Wruhs评分等方面明显优于锁定钢板技术,并具有缩短骨折愈合时间的倾向,是一种治疗胫骨AO 42-C型骨折安全、有效的方法。
参 考 文 献
[1] Schatzker J, Tile M. The rationale of operative fracture care. 3rd. Berlin: Springer-Verlag Berlin Heidelberg Gmbh,2005, 475-476.
[2] Saied A, Ostovar M, Mousavi AA, Arabnejhad F. Comparison of intramedullary nail and plating in treatment of diaphyseal tibial fractures with intact fibulae: a randomized controlled trial. Indian J Orthop, 2016, 50 (3): 277-282.
[3] Augat P, von Ruden C. Evolution of fracture treatment with bone plates. Injury, 2018, 49 (Suppl 1): S2-S7.
[4] Wajnsztejn A, Pires RES, Dos Santos ALG, Labronici PJ, Fernandes HJA, Ferretti M. Minimally invasive posteromedial percutaneous plate osteosynthesis for diaphyseal tibial fractures: technique description. Injury, 2017, 48 (Suppl 4): S6-S9.
[5] Panjabi MM, Walter SD, Karuda M, White AA, Lawson JP. Correlations of radiographic analysis of healing fractures with strength: a statistical analysis of experimental osteotomies. J Orthop Res, 1985, 3 (2): 212-218.
[6] Johner R, Wruhs O. Classification of tibial shaft fractures and correlation with results after rigid internal fixation. Clin Orthop Relat Res, 1983, (178): 7-25.
[7] Mukherjee S, Arambam MS, Waikhom S, Santosha, Masatwar PV, Maske RG. Interlocking nailing versus plating in tibial shaft fractures in adults: a comparative study. J Clin Diagn Res, 2017, 11 (4): RC08-RC13.
[8] Daolagupu AK, Mudgal A, Agarwala V, Dutta KK. A comp-arative study of intramedullary interlocking nailing and minimally invasive plate osteosynthesis in extra articular distal tibial fra-ctures. Indian J Orthop, 2017, 51 (3): 292-298.
[9] Costa ML, Achten J, Griffin J, Petrou S, Pallister I, Lamb SE, Parsons NR, Fix DTTI. Effect of locking plate fixation vs intramedullary nail fixation on 6-month disability among adults with displaced fracture of the distal tibia: the UK FixDT randomized clinical trial. JAMA, 2017, 318 (18): 1767-1776.
[10] Vallier HA. Current evidence: plate versus intramedullary nail for fixation of distal tibia fractures in 2016. J Orthop Trauma, 2016, 30 (Suppl 4): S2-S6.
[11] Janssen KW, Biert J, van Kampen A. Treatment of distal tibial fractures: plate versus nail: a retrospective outcome analysis of matched pairs of patients. Int Orthop, 2007, 31 (5): 709-714.
[12] Yoon RS, Bible J, Marcus MS, Donegan DJ, Bergmann KA, Siebler JC, Mir HR, Liporace FA. Outcomes following combined intramedullary nail and plate fixation for complex tibia fractures: a multi-centre study. Injury, 2015, 46 (6): 1097-1101.
[13] Lakhotia D, Sharma G, Khatri K, Kumar GN, Sharma V, Farooque K. Minimally invasive osteosynthesis of distal tibial fra-ctures using anterolateral locking plate: evaluation of results and complications. Chin J Traumatol, 2016, 19 (1): 39-44.
[14] Loughenbury PR, Gledhill RA, Evans N. Tibiofibula tran-sposition in high-energy fractures. Case Rep Emerg Med, 2016, 2016: 6718679.
[15] Jankovic A, Korac Z, Bozic NB, Stedul I. Influence of knee flexion and atraumatic mobilisation of infrapatellar fat pad on incidence and severity of anterior knee pain after tibial nailing. Injury, 2013, 44 (Suppl 3): S33-S39.
[16] Foux A, Yeadon AJ, Uhthoff HK. Improved fracture healing with less rigid plates. A biomechanical study in dogs. Clin Orthop Relat Res, 1997, (339): 232-245.
[17] Braly HL, OConnor DP, Brinker MR. Percutaneous autologous bone marrow injection in the treatment of distal meta-diaphyseal tibial nonunions and delayed unions. J Orthop Trauma, 2013, 27 (9): 527-533.
[18] Wenger R, Oehme F, Winkler J, Perren SM, Babst R, Beeres FJP. Absolute or relative stability in minimal invasive plate osteo-synthesis of simple distal meta or diaphyseal tibia fractures? Injury, 2017, 48 (6): 1217-1223.
[19] Strauss EJ, Alfonso D, Kummer FJ, Egol KA, Tejwani NC. The effect of concurrent fibular fracture on the fixation of distal tibia fractures: a laboratory comparison of intramedullary nails with locked plates. J Orthop Trauma, 2007, 21 (3): 172-177.
[20] Hak DJ, Toker S, Yi C, Toreson J. The influence of fracture fixation biomechanics on fracture healing. Orthopedics, 2010, 33 (10): 752-755.
[21] Georgiannos D, Lampridis V, Bisbinas I. Fragility fractures of the ankle in the elderly: open reduction and internal fixation versus tibio-talo-calcaneal nailing: short-term results of a prospective randomized-controlled study. Injury, 2017, 48 (2): 519-524.
[22] Mauffrey C, McGuinness K, Parsons N, Achten J, Costa ML. A randomised pilot trial of “locking plate” fixation versus intra-medullary nailing for extra-articular fractures of the distal tibia. J Bone Joint Surg Br, 2012, 94 (5): 704-708.
(收稿日期:2019-08-29)
(本文編辑:洪悦民)

