综合性康复介入辅助早期营养支持策略对早产儿营养状况及生长发育的影响
吴爱珍 蒋慧玲 高丽娟


[摘要] 目的 探討综合性康复介入辅助早期营养支持策略治疗对早产儿营养状况及生长发育的影响。 方法 选取2015年1月~2018年8月在我院妇产科出生的早产儿120例。将其分为观察组与对照组,每组60例。两组早产儿均予以早期营养支持策略,对照组予以婴儿常规体检并采用常规育儿方式进行养育;观察组在对照组基础上予以综合性康复介入辅助治疗。观察并比较两组早产儿2周内营养状况及生长发育指标变化情况。 结果 治疗2周后,两组早产儿血清PA和ALB水平均较出生时明显上升(P<0.05或P<0.01),且观察组早产儿上升幅度较对照组更明显(P<0.05);同时观察组早产儿体质量、头围增加速度和身长增长速率明显快于对照组(P<0.05)。结论 综合性康复介入辅助早期营养支持策略治疗用于早产儿不仅可显著提高血清PA和ALB水平,改善其营养状况;而且可加快早产儿的生长速率,促进其生长发育,降低生长迟缓发生率。
[关键词] 早产儿;早期营养支持策略;综合性康复介入;营养状况;生长发育
[中图分类号] R722.6 [文献标识码] B [文章编号] 1673-9701(2020)01-0056-03
Effect of comprehensive rehabilitation interventional combined with early nutrition support strategy on nutritional status, growth and development of premature infants
WU Aizhen JIANG Huiling GAO Lijuan
Department of Pediatrics, Lishui Central Hospital in Zhejiang Province, Lishui 323000, China
[Abstract] Objective To explore the effect of comprehensive nutritional rehabilitation interventional combined with early nutritional support strategy on nutritional status, growth and development of premature infants. Methods A total of 120 preterm infants born in our department of obstetrics and gynaecology from January 2015 to August 2018 were selected and divided into observation group and control group, with 60 patients in each group. Premature infants in both groups were given early nutrition support strategies, and the control group was given routine physical examination and adopted regular parenting methods for parenting. The observation group was given comprehensive rehabilitation interventional therapy based on the treatment of the control group. The changes in nutritional status, growth and development indicators were observed and compared between the two groups of preterm infants within 2 weeks. Results After 2 weeks of treatment, the serum PA and ALB levels of both groups increased significantly (P<0.05 or P<0.01), and the increase in the observation group was more obvious than that of the control group(P<0.05). At the same time, the body weight, head circumference increase rate and body length growth rate of premature infants in the observation group were significantly faster than those in the control group(P<0.05). Conclusion Comprehensive rehabilitation interventional combined with early nutritional support strategy for preterm infants can not only significantly improve serum PA and ALB levels, improve their nutritional status, but also accelerate the growth rate of premature infants, promote their growth and development, and reduce low growth retardation rate.
[Key words] Premature infants; Early nutritional support strategies; Comprehensive rehabilitation intervention; Nutritional status; Growth and development
早产儿由于在母体内发育时间短、自身营养储备不足等因素,不适当的营养供给极易发生宫外发育迟緩,影响器官结构和功能发育,严重时造成神经系统的损伤。因此,对早产儿进行积极营养支持干预纠正宫外发育迟缓,改善其营养状况显得尤为重要[1-2]。目前临床上对早产儿的早期营养支持策略主要包括静脉营养、母乳喂养及肠外营养支持等[3,4]。国外诸多研究发现,早产儿在早期营养支持策略基础上予以口部感觉及肌力训练、非营养性吸吮、早期微量喂养和新生儿抚触等综合性康复介入手段可提高营养支持的效果等[5,6]。本研究探讨综合性康复介入辅助早期营养支持策略对早产儿营养代谢及生长发育的影响,现报道如下。
1 资料与方法
1.1 一般资料
选取2015年1月~2018年8月在我院妇产科出生的早产儿120例。纳入标准[7]:①胎龄28~37周,出生体质量≤2000 g;②生命体征稳定,预计住院时间>2周。排除标准[8]:①先天性消化道疾病、遗传代谢性或心肺疾病者;②有手术史者。采用抛硬币法将早产儿分为观察组与对照组,每组60例。两组早产儿的性别、胎龄、出生体质量和5 min Apgar评分等比较差异无统计学意义(P>0.05),具有可比性。见表1。
1.2 方法
两组早产儿均予以早期营养支持策略,采用母乳喂养或鼻饲喂养,如母乳不足就补充早产儿专用配方奶喂养;同时在24 h内给予静脉营养支持,保证热量摄入在(250~335)kJ/(kg·d),予氨基酸3.5 g/(kg·d)和20%脂肪乳3 g/(kg·d),当肠内营养达到418.68 kJ/(kg·d)时停止静脉营养。对照组予以婴儿常规体检并采用常规育儿方式进行养育。观察组在对照组基础上予以综合性的康复介入辅助治疗,包括:①口部感觉及肌力训练:使用消毒棉签依次刺激唇周、舌尖、两侧面颊和舌面前2/3,5 min/次,3次/d;②非营养性吸吮:在喂奶前后予以早产儿型硅胶安抚奶嘴吸吮,10 min/次,3次/d;③新生儿抚触:用双手拇指和掌面依次抚触头部、胸腹部、四肢、手掌手指、足底脚趾和背部皮肤,20 min/次,3次/d。观察并比较两组早产儿2周内营养状况及生长发育指标变化情况。
1.3 观察指标
1.3.1 营养状况指标 采用血清前白蛋白(PA)和白蛋白(ALB)评估营养状况,采用全自动生化分析仪测定。
1.3.2 生长发育指标 包括体质量、头围增加速度和身长增长速率。
1.4 统计学处理
应用SPSS18.0统计学软件,计量资料以均数±标准差(x±s)表示,采用t检验,计数资料以[n(%)]表示,采用χ2检验,P<0.05为差异有统计学意义。
2 结果
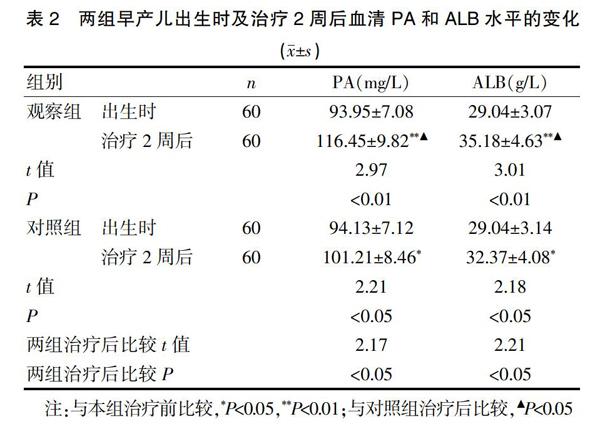
2.1 两组早产儿出生时及治疗2周后血清PA和ALB水平的变化
两组早产儿出生时血清PA和ALB水平比较差异无统计学意义(P>0.05);治疗2周后,两组早产儿血清PA和ALB水平均较出生时明显上升(P<0.05或P<0.01),且观察组早产儿上升的幅度较对照组更明显(P<0.05)。见表2。
2.2 两组早产儿生长发育情况比较
观察组早产儿体质量、头围增加速度和身长增长速率明显快于对照组,差异有统计学意义(P<0.05)。见表3。
3 讨论
近年来,随着新生儿重症监护技术不断进步,早产儿尤其是低出生体重儿的救治成功率大幅度上升[9,10]。但是由于早产儿呼吸和消化道发育尚不完善,早期吸吮、吞咽和协调功能较差,贲门括约肌发育欠完全并处于松弛状态,因此经口母乳喂养易发生胃食道反流、呼吸暂停或喂养不耐受等现象,这使得临床医生延迟经口母乳喂养或对加奶量比较谨慎,使得早产儿营养物质摄入不足[11-13]。以往临床上常采用肠外营养来满足早产儿的营养需求,但长时间的肠外营养不仅影响早产儿味觉、知觉的发育,且易引起胃肠黏膜萎缩和胆汁淤滞性黄疸等风险的增加。采用早期营养支持策略不仅降低了早产儿的早期营养缺失,有利于其肠道功能的早期建立,促进生长发育,降低早产儿宫外发育迟缓的发生比例,但由于部分早产儿予以早期营养支持策略后效果仍欠理想,因此,采取有效措施对早产儿早期营养支持策略进行积极干预,改善其营养状况显得尤为重要[14-17]。
本研究采用口部感觉及肌力训练、非营养性吸吮、早期微量喂养和新生儿抚触等综合性的康复介入辅助早期营养支持策略治疗用于早产儿取得了较好的效果,其中口部感觉及肌力训练,使得口腔肌肉的力量得到加强,有利于早产儿的吸吮;同时口部感觉训练通过感受器传递到中枢神经,加快中枢和周围神经的发育成熟,改善吸吮和吞咽功能[18]。非营养性吸吮是指不能接受经口喂养的新生儿在采用胃管喂养或全静脉营养时,给其吸空的橡皮奶头,这不仅促进早产儿口腔满足感,刺激其味觉和知觉的尽早发育,促进口腔舌脂酶的分泌释放,有利于吸吮反射的发育成熟,使得吸吮力逐渐增加,可兴奋迷走神经,促进胃肠道的生长发育及胃肠功能的成熟;还能改善早产儿生理、行为[19,20];新生儿抚触是一种通过触摸新生儿的皮肤和机体,刺激皮肤感受器上传到中枢神经系统,促进新生儿身心健康发育的科学育婴新方法;这不仅可以刺激早产儿感觉器官的发育,还可以增进早产儿的生理成长和神经系统反应,更可以增加早产儿对外在环境的认知,在触摸的过程中,也加深亲子之间的浓厚感情;同时可加强头、颈和肢体姿势的控制,为吞咽和呼吸更加稳定奠定基础,不仅减少停顿-吞咽-停顿状态,而且增加呼气-吞咽-呼气状态,改善早产儿经口喂养的技能,进一步完成吸吮、吞咽、呼吸的协调[21]。本研究显示,观察组早产儿血清PA和ALB水平上升的幅度较对照组更明显。提示综合性康复介入辅助早期营养支持策略治疗用于早产儿可显著提高血清PA和ALB水平,改善其营养状况;同时研究还发现,观察组早产儿体质量、头围增加速度和身长增长速率明显快于对照组。提示综合性康复介入辅助早期营养支持策略治疗用于早产儿可加快早产儿的生长速率,促进其生长发育。
总之,综合性康复介入辅助早期营养支持策略治疗用于早产儿不仅可显著提高血清PA和ALB水平,改善其营养状况;而且可加快早产儿的生长速率,促进其生长发育,降低生长迟缓发生率。
[参考文献]
[1] Tekgündüz K,Gürol A,Apay SE,et al. Effect of abdomen massage for prevention of feeding intolerance in preterm infants[J]. Ital J Pediatr,2014,40(14):89-94.
[2] Fucile S,Gisel EG,McFarland DH,et al. Oral and non-oral sensorimotor interventions enhance oral feeding performance in preterm infants[J]. Dev Med Child Neurol,2011,53(9):829-835.
[3] Unger S,Stintzi A,Shah Pl,et al. Gut microbiota of the very-low-birth-weight infant[J]. Pediatr Res,2015,77(1-2):205-213.
[4] Costa S,Maggio L,Sindico P,et al. Preterm small for gestational age infants are not at higher risk for parenteral nutrition-associated cholestasis[J]. J Pediatr,2010, 156(4):575-579.
[5] Kumar J,Upadhyay A,Dwivedi AK,et al. Effect of oil massage on growth in preterm neonates less than 1800 g:A randomized control trial[J]. Indian J Pediatr,2013,80(6):465-469.
[6] 張健芳,邓琼晖,邓智青,等. 早期不同喂养联合不同营养支持方式对早产儿生长与代谢的影响[J]. 吉林医学,2018,39(3):460-462.
[7] 倪文思,张永红,李婷,等. 早期康复介入降低早产儿宫外生长发育迟缓的研究[J]. 中国当代儿科杂志,2018, 20(2):97-101.
[8] Ng E,Shah V. Erythromycin for the prevention and treatment of feeding intolerance in preterm infants[J]. Cochrane Database Syst Rev,2008,16(3):1815-1816.
[9] 宋朝敏,杨长仪,王程毅,等. 早期营养支持策略对极低出生体重儿生长代谢及并发症的影响[J]. 中国新生儿科杂志,2013,28(6):379-384.
[10] Kamarudin NA,Manan MM,Zulkifly HH,et al. Amino acid dosing in parenteral nutrition for very low birth weight preterm neonates:An outcome assessment[J]. Asia Pac J Clin Nutr,2016,25(1):53-61.
[11] Bora R,Mukhopadhyay K,Saxena AK,et al. Prediction of feed intolerance and necrotizing enterocolitis in neonates with absentend diastolic flow in umbilical artery and the correlation of feed intolerance with postnatal superior mesenteric artery flow[J]. The Journal of Maternal-Fetal & Neonatal Medicine,2009,22(11):1092-1096.
[12] Vlaardingerbroek H,van Goudoever JB,van den Akker CH. Initial nutritional management of the preterm infants[J].Early Hum Dev,2009,85(11):691-695.
[13] Scott C Denne. Early nutritional support for extremely premature infants:What aminoacid amount should be given?[J]. AM J Clin Nutr,2016,103(8):1383-1384.
[14] Valentine CJ,Fernandez S,Rogers LK,et al. Early amino-acid administration improves preterm infant weight[J]. J Perinatol,2009,29(6):428-432.
[15] Jirapaet K,Jirapaet V,Sritipsukho S. Safety of initiating early enteral feeding with slow volume advancement in preterm infants[J]. J Med Assoc Thai,2010,93(10):1177-1187.
[16] Rodriguez NA,Meier PP,Groer MW,et al. A pilot study to determine the safety and feasibility of oropharyngeal administration of own mother's colostrum to extremely low-birth-weight infants[J]. Adv Neonatal Care,2010,10(4):206-212.
[17] Meier PP,Engstrom JL,Patel AL,et al. Improving the use of human milk during and after the NICU stay[J]. Clin Perinatol,2010,37(1):217-245.
[18] Fucile S,McFarland DH,Gisel EG,et al. Oral and nonoral sensorimotor interventions facilitate suck-swallow-respiration functions and their coordination in preterm infants[J]. Early Hum Dev,2012,88(6):345-350.
[19] 王梅芳. 非营养性吸吮促进早产儿胃肠道功能成熟的效果[J]. 江苏医药,2016,42(1):99-100.
[20] 经连芳,韦秋芬,李燕,等. 非营养性吸吮对早产儿营养胃肠道转运时间及喂养相关并发症的影响[J]. 中国妇幼健康研究,2017,28(1):16-17.
[21] Pepino VC,Mezzacappa MA. Application of tactile/kinesthetic stimulation in preterm infants:A systematic review[J]. J Pediatr(Rio J),2015,91(3):213-233.
(收稿日期:2018-12-27)

