Analysis of factors potentially predicting prognosis of colorectal cancer
Li-Jun Jin,Wei-Bin Chen,Xiao-Yu Zhang,Jie Bai,Hao-Chen Zhao,Zun-Yi Wang
Abstract
Key words: Colorectal cancer; Prognosis; Influencing factors; Combination assessment
INTRODUCTION
The prognosis of colorectal cancer is poor,and its mortality rate ranks third among all malignancies in the world[1-3].Surgery is the main method of colorectal cancer treatment.Accurate assessment of surgical prognosis plays an important role in the treatment of colorectal cancer patients.Currently,studies on the factors affecting the prognosis of colorectal cancer are very popular.Studies have shown that high Glasgow prognostic score (GPS) in colorectal cancer is more likely to predict a poor prognosis[4-6].The results of Arfaet al[7]showed that tumor-node-metastasis (TNM)stage is associated with the prognosis of colorectal cancer.Studies by Kanemitsuet al[8]have demonstrated that histological type and degree of differentiation of tumors can affect their biological behavior and further affect clinical outcomes.In addition,studies have found thatin vivoinflammatory response can have an impact on the occurrence and development of tumors[9].Serum C-reactive protein[10,11],albumin[12,13],C-reactive protein/albumin ratio (CAR)[14-16],and neutrophil-lymphocyte ratio(NLR)[17,18]reveal the possibility of inflammation-related complications,and have certain predictive value for prognosis[19].However,there is no systematic analysis about the factors affecting the prognosis of colorectal cancer.Therefore,this study defined colorectal cancer patients as the research subjects.We statistically analyzed the influence of clinical data and serology and histology on the prognosis of patients with colorectal cancer,and assessed the accuracy of the combination of all indicators for the prognosis evaluation,aiming to find a more accurate assessment.This study is expected to provide a new method for predicting the prognosis of colorectal cancer in the early stage of clinical diagnosis and improve the prognosis of patients.
MATERIALS AND METHODS
Research subjects
A total of 374 patients with colorectal cancer who were admitted to Cangzhou Central Hospital from March 2012 to March 2015 were recruited.The inclusion criteria were:(1) Pathological diagnosis of colorectal cancer; (2) Patients who underwent radical surgery; (3) Complete clinical data,disease history,and family history data; and (4)Complete physical examination,routine blood tests,detection of tumor markers,and relevant laboratory examinations such as coagulation function within one week before surgery.The exclusion criteria were: (1) Other carcinomas combined; (2) Pre-operative infection or insufficient infection evidence but body temperature > 38 °C; (3) Patients combined with cardiovascular disease,cerebrovascular disease,and diseases of the liver,kidney,and other important organs; and (4) Undergoing radiotherapy,chemotherapy,biotherapy,or gene therapy before surgery.The study was approved by the Ethics Committee of Cangzhou Central Hospital.All patients included in the study had a detailed understanding of the research content and provided informed consent.
Research methods
Clinical data collection:After admission,complete clinical data,including age,gender,height,weight,family history (colorectal cancer in three generations of close relatives) and smoking history were collected.Body mass index (BMI) was calculated.All patients were staged by the TNM staging method and the improved Dukes staging method according to pathological findings[20].
Serological examination:All patients received carcinoembryonic antigen (CEA),carbohydrate antigen 199 (CA199),C-reactive protein,albumin,D-dimer,and fibrinogen detection as well as routine blood tests one week before surgery.CEA and CA199 were tested by chemiluminescence with a Roche kit.Routine blood tests were performed with a CC-3200 automatic blood tester and supporting kit.The numbers of neutrophil granulocytes,white blood cells,lymphocytes,and platelets were recorded,and NLR was calculated.C-reactive protein,albumin,D-dimer,and fibrinogen were detected using an Abbott C16000 automatic biochemical analyzer (Abbott Laboratories,Inc.).CAR was calculated.According to the results of C-reactive protein and albumin detection,GPS was calculated according to the following rules: (1)Increased C-reactive protein; and (2) Hypoproteinemia.Two points were recorded if both (1) and (2) were satisfied,1 point if (1) or (2) was satisfied,and 0 points if normal C-reactive protein and no hypoproteinemia were found.
1.3 统计学分析 采用SPSS 21.0软件进行数据处理,用率表示乳腺超声光散射成像与血清CA153、CEA联合检测对乳腺肿瘤的诊断结果与病理诊断结果对比、乳腺超声光散射成像与血清CA153、CEA单独和联合检测对乳腺肿瘤的诊断价值等计数资料,用χ2检验;用均数±标准差表示两组患者的MHC测定值、血清CA153、CEA水平等计量资料,用t检验,检验水准α=0.05。
Surgery and histological examination:Under general anesthesia,colorectal cancer radical surgery was performed.Tumor location,size,depth of invasion,lymph node metastasis,and distant metastasis were recorded.The excised specimens were flattened and fixed,and pathological examination was performed.The pathological tissues were serially sectioned,fixed with 10% formalin,and embedded in paraffin,followed by hematoxylin-eosin and immunohistochemical staining.All the sections were observed by two experienced pathologists.The pathological tissue classification and expression of proliferating cell nuclear antigen (PCNA) and p53 were observed.After surgery,patients' vital signs and wound oozing were closely observed.Antiinflammatory drugs and intravenous nutrition were given regularly.
Follow-up
A total of 374 patients who participated in the study were followed for 3 years.The first follow-up was performed 1 mo after the end of treatment,followed by every 3 mo within 2 years.After 2 years,follow-up was performed every 6 mo.The endpoint events were defined as adverse prognostic events during follow-up,including recurrence of colorectal cancer,increased stage,other organ metastases,and death from colorectal cancer and its complications.Patients' refusal to visit,halfway out,and death from other reasons unrelated to the study were defined as loss to followup.According to the follow-up results,patients with endpoint events were defined as a poor prognosis group,and the remaining patients were defined as a good prognosis group.Differences in clinical data,serology,and histology were analyzed.
Statistical analysis
Analyses were performed using Statistical Product and Service Solutions software.The measurement data are expressed as the mean ± standard deviation,and comparisons were performed using an independent samplet-test.The count data are expressed in case (percentage),and the chi-square test was used for comparison.Survival analysis was performed by the Kaplan-Meier method.The poor prognosis rate was calculated and the survival curve was drawn.Multivariate COX regression was used to analyze independent influencing factors for the prognosis of colorectal cancer.The receiver-operating characteristic (ROC) curve was used to evaluate the predictive value of each independent influencing factor and their combination for the prognosis of colorectal cancer.The difference was considered statistically significant atP< 0.05.
RESULTS
Patient follow-up results
A total of 374 patients were enrolled in the study.The Kaplan-Meier survival curve showed an increase trend in the number of adverse prognosis cases over time (Figure 1).At the end of follow-up,19 patients were lost to follow-up.There were a total of 355 patients with complete follow-up data,of whom 81 developed endpoint events.In these 81 patients,40 had recurrence of colorectal cancer (Figure 2A),26 had liver metastases (Figure 2B),and 15 had bone metastases (Figure 2C).The poor prognosis rate was 22.82%.
Comparison of indicators between the prognosis group and poor prognosis group
Of the 355 patients with colorectal cancer who received complete follow-up data,186 were male and 169 were female,with an average age of 59.83 ± 13.92 years and mean tumor size of 4.32 ± 2.56 cm.In terms of tumor location,there were 52 cases in the ascending colon,21 in the transverse colon,35 in the descending colon,106 in the sigmoid colon,and 141 in the rectum.In terms of TNM stage,there were 16 cases of stage I,251 stage II,54 stage III,and 34 stage IV.In terms of Dukes stage,there were 17 cases of grade A,225 grade B,and 112 grade C.Among the pathological types,there were 230 cases of adenocarcinoma and 125 cases of mucinous adenocarcinoma and signet ring cell carcinoma.
According to the prognosis results,the prognosis group included 274 patients and the poor prognosis group included 81 patients.The comparison of the indicators before treatment in the two groups of patients is shown in Table 1.The age,tumor diameter,TNM stage,PCNA index,GPS,C-reactive protein,albumin,white blood cell (WBC) count,NLR,CAR,D-dimer,fibrinogen,CEA,and CA199 in the poor prognosis group were significantly higher than those in the good prognosis group (P< 0.05).The gender,BMI,smoking proportion,alcohol abuse ratio,family history ratio,tumor location,tumor histology type,Dukes grade,proportion of positive P53,and platelet count were similar between the two groups (P> 0.05).
Multivariate COX regression analysis of the prognosis in patients with colorectal cancer
Further multivariate COX regression analysis was performed on the different indicators between the two groups.The results showed that the impact of age,tumor diameter,C-reactive protein,albumin,WBC count,fibrinogen,and CA199 on the prognosis was not significant (P> 0.05).TNM stage,PCNA,GPS,NLR,CAR,Ddimer,and CEA were independent influencing factors for the prognosis of colorectal cancer (P= 0.000) (Table 2).
Receiver operating characteristic curve analysis of potential indicators for predicting colorectal cancer prognosis
The ROC curve was used to further analyze the predictive value of TNM stage,PCNA,GPS,NLR,CAR,D-dimer,and CEA for the prognosis of colorectal cancer.The results showed that each indicator can predict the prognosis of colorectal cancer (AUC> 0.6 for all).Among them,NLR had the highest accuracy with an AUC of 0.925(95%CI: 0.860-0.966),sensitivity of 94.12%,and slightly lower specificity of 80.25%.Ddimer was the second,and its AUC was 0.879 (95%CI: 0.841-0.911),with a specificity of 100% and sensitivity of only 58.02%.GPS was the third,and its AUC was 0.872(95%CI: 0.832-0.905),with a sensitivity and specificity of 88.89% and 85.04%,respectively (Table 3 and Figure 3).
Each indicator had some limitations in predicting the prognosis of colorectal cancer,respectively.Therefore,this study attempted to establish a combination model based on logistic regression to predict the prognosis.The result showed that the accuracy of the combination of all indicators in predicting the prognosis of colorectal cancer was the highest (AUC = 0.973,95%CI: 0.950-0.987),which was significantly higher than that of any indicator alone (P< 0.05).The best diagnostic point was 0.206,with a sensitivity of 92.59% and specificity of 90.51% (Figure 4).
非营利组织一般都是以绿色营销模式为主,不断宣传和加强民众的绿色环保观念,非营利组织会要求在各种类型的公共服务以及产品的设计、研发、量化生产和消费等环节,都需要考虑到对环境的影响和社会公众的长远利益。所以,在低碳营销模式的发展过程中,非营利组织应该要积极配合有关政府部门的工作,以节约能源和保护环境为主旨,大力宣传低碳营销模式的理念。[4]从社会公众的角度考虑,非营利组织帮助消费者建立低碳消费观念,同时也帮助企业专注于低碳技术的研发生产和营销,促使消费者深入细致了解低碳营销模式的优势所在,更加自主地选择使用低碳产品,促使整个社会步入低碳经济的可持续发展的道路。

Figure 1 Survival curve analysis of patients with colorectal cancer (Kaplan-Meier).
DISCUSSION
The detection rate of colorectal cancer has increased recently[21].Because of the hidden symptoms in early stage,the prognosis of colorectal cancer is poor[22].Accurate assessment of patient outcomes is critical to the choice of clinical treatments.Currently,the prognosis of colorectal cancer is predicted mainly through CEA level,pathological typing,TNM staging,etc.[23-25],but the accuracy of prediction cannot be guaranteed due to different individuals[26].Recent studies have shown that GPS,Creactive protein,albumin,CAR,NLR and other inflammatory indicators can reveal the prognosis of malignant tumors,but the accuracy of different predictive indicators for the prognosis of colorectal cancer is uncertain[27].Therefore,this study recruited colorectal cancer patients and screened the clinical data and serology and pathology data to find the indicators that can accurately evaluate the prognosis.
Survival analysis of patients with colorectal cancer
The incidences of postoperative recurrence,metastasis,and tumor-related death are very high[28].A 3-year follow-up analysis in the study showed that the survival curves decreased significantly at 12-18 mo and 30-36 mo,respectively.It indicated that the number of patients with a poor prognosis increased rapidly at 12-18 mo and 30-36 mo.Among the patients with a poor prognosis,the incidence of colorectal cancer recurrence was the highest,accounting for 49.4% of all patients with a poor prognosis,followed by liver metastasis (32.1%) and bone metastasis (18.5%).The overall poor prognosis rate was 22.82%,which is similar to the recent finding of Shenet al[29](24.3%),and lower than the result of Lujanet al[30](38.3%-45.6%).The possible reason is that with the improvement of people's health awareness,the detection rate of early colorectal cancer is increased.More patients can receive timely treatment in early stage,in addition to the popularization of endoscopic and laparoscopic treatment techniques.Hence the prognosis of colorectal cancer is improved.
Multivariate regression analysis of the prognosis after colorectal cancer surgery
With the increase of age,the immune clearance ability and postoperative recovery ability of carcinoma are significantly reduced.The possibility of poor prognosis is gradually increased[31-33].Studies have revealed that gender,smoking history,family history,etc.can affect the incidence and outcome of carcinoma[34-36].Tumor location,size,TNM stage,Dukes stage,and pathological classification can indicate the progression of colorectal cancer and its invasion and metastasis ability.They are often utilized to predict the prognosis of colorectal cancer[37].PCNA and p53 are common clinical tumor-related detection indicators,and their abnormal expression levels may be associated with colorectal cancer recurrence and poor prognosis[38-42].Serological indicators such as neutrophils,lymphocytes,albumin,and C-reactive protein are commonly used indicators for monitoring inflammation in the body.Studies have shown that inflammation can promote tumor metastasis and recurrence[43-44].In addition,inflammatory factors can inhibit the body's immune response to tumors and stimulate tumor formation around the tumor,thereby promoting tumor growth and metastasis[45].
This study compared clinical,serological,and histological indicators of patients with different prognoses.It indicated that age,tumor diameter,TNM stage,PCNA index,GPS,C-reactive protein,albumin,WBC count,NLR,CAR,D-dimer,fibrinogen,CEA,and CA199 were possible risk factors for poor prognosis in patients with colorectal cancer.Further multivariate COX regression analysis of the above indicators showed that TNM stage,PCNA,GPS,NLR,CAR,D-dimer,and CEA were independent influencing factors for the prognosis of colorectal cancer.It suggested that when advanced TNM stage,high PCNA expression levels,GPS > 0,increase of NLR and CAR,or increase of D-dimer and CEA levels occurs,the possibility of poor prognosis should be guarded.In addition,early treatment,control of inflammation levels,and monitoring of D-dimer and CEA levels can prevent poor prognosis.It is worth noticing that NLR,CAR,and GPS are calculated by two serological indicators,which can simultaneously reveal changes of two indicators.Furthermore,TNM staging includes tumor diameter,lymph node metastasis,and distant metastasis.It indicated that multiple indicators are preferred when the accuracy of prognosis assessment based on single factor is poor to improve the accuracy of the evaluation results.
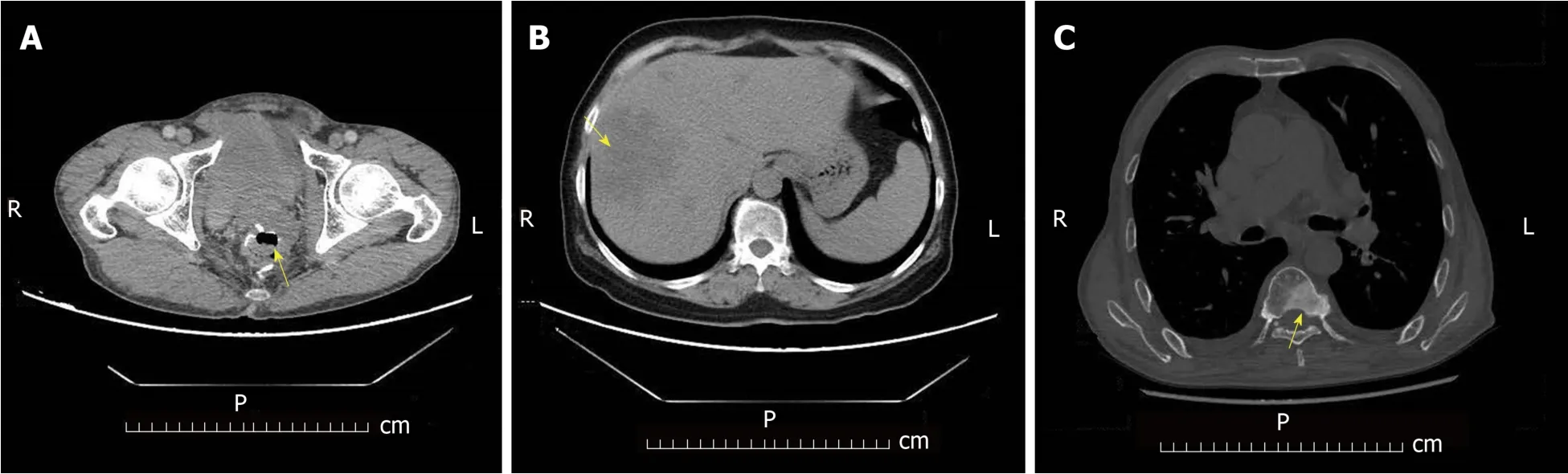
Figure 2 Endpoint events during postoperative follow-up of colorectal cancer patients.
Potential indicators predicting the prognosis of colorectal cancer
Based on COX regression results,this study evaluated the ability of TNM stage,PCNA,GPS,NLR,CAR,D-dimer,and CEA to predict the prognosis of colorectal cancer.According to the evaluation results,the accuracy of NLR,D-dimer,and GPS was significantly higher than that of TNM stage,PCNA,and CAR.Among them,NLR had the highest accuracy.The possible reason may be that NLR is the ratio of neutrophils to lymphocytes.Both of them are reliable indicators for the inflammatory responsein vivo.Neutrophils can release active factors to activate NF-κB,which is related to the formation of tumors.Also,it can inhibit the immunity of the body through the inflammatory reaction,and help tumor cells escape from immunization.In addition,it can promote tumor growth by promoting neovascularization.Hence,its increase is beneficial to tumorigenesis[43,44].As one of the main cells of the body's immunity,lymphocytes can produce an immune response to tumor cells,and the decrease of the lymphocytes leads to a decrease in the body's ability to inhibit tumors.Therefore,increased NLR is beneficial to tumor survival and associated with a poor prognosis.The hypercoagulable state of the blood is beneficial for the metastasis of malignant tumors[46].Studies have confirmed that preoperative D-dimer levels are associated with tumor prognosis[47-49].In this study,D-dimer had a higher predictive ability for poor prognosis of colorectal cancer,second only to NLR.GPS is determined by the level of serum C-reactive protein and whether it has hypoproteinemia,which can simultaneously indicate the inflammatory condition and nutritional status of the body.In this study,GPS also had a high predictive ability for poor prognosis of colorectal cancer,which is similar to the study by Windet al[50].

Table 1 Comparison of indicators between the good prognosis group and poor prognosis group before treatment
However,each indicator has a certain limitation in predicting the prognosis of colorectal cancer.Therefore,this study combined the independent risk factors to evaluate the accuracy for predicting the prognosis.It revealed that the accuracy of the combination in predicting the prognosis of colorectal cancer was significantly higher than the accuracy of individual indicators.It suggested that in the evaluation of surgical outcomes in patients with colorectal cancer,the combination of TNM stage,PCNA,GPS,NLR,CAR,D-dimer,and CEA has a higher accuracy.
Insufficient and prospects
This study is a single-center study and may have certain limitations.The follow-up time was short,and the indicators affecting long-term prognosis may be ignored.In future,multi-center research is considered to expand the sample size for improving the reliability of the research results.Meanwhile,the length of follow-up can be extended.The influencing factors on short-term and long-term prognosis of colorectal cancer should be analyzed respectively.
In conclusion,this study analyzed the clinical data and serological and pathological indicators that may affect the prognosis of colorectal cancer.It indicated that the independent influencing factors for the prognosis of colorectal cancer include TNM stage,PCNA,GPS,NLR,CAR,D-dimer,and CEA.Among them,NLR,D-dimer,and GPS have higher prediction capabilities.The combination of all independent factors can make a more accurate assessment of the prognosis of colorectal cancer.
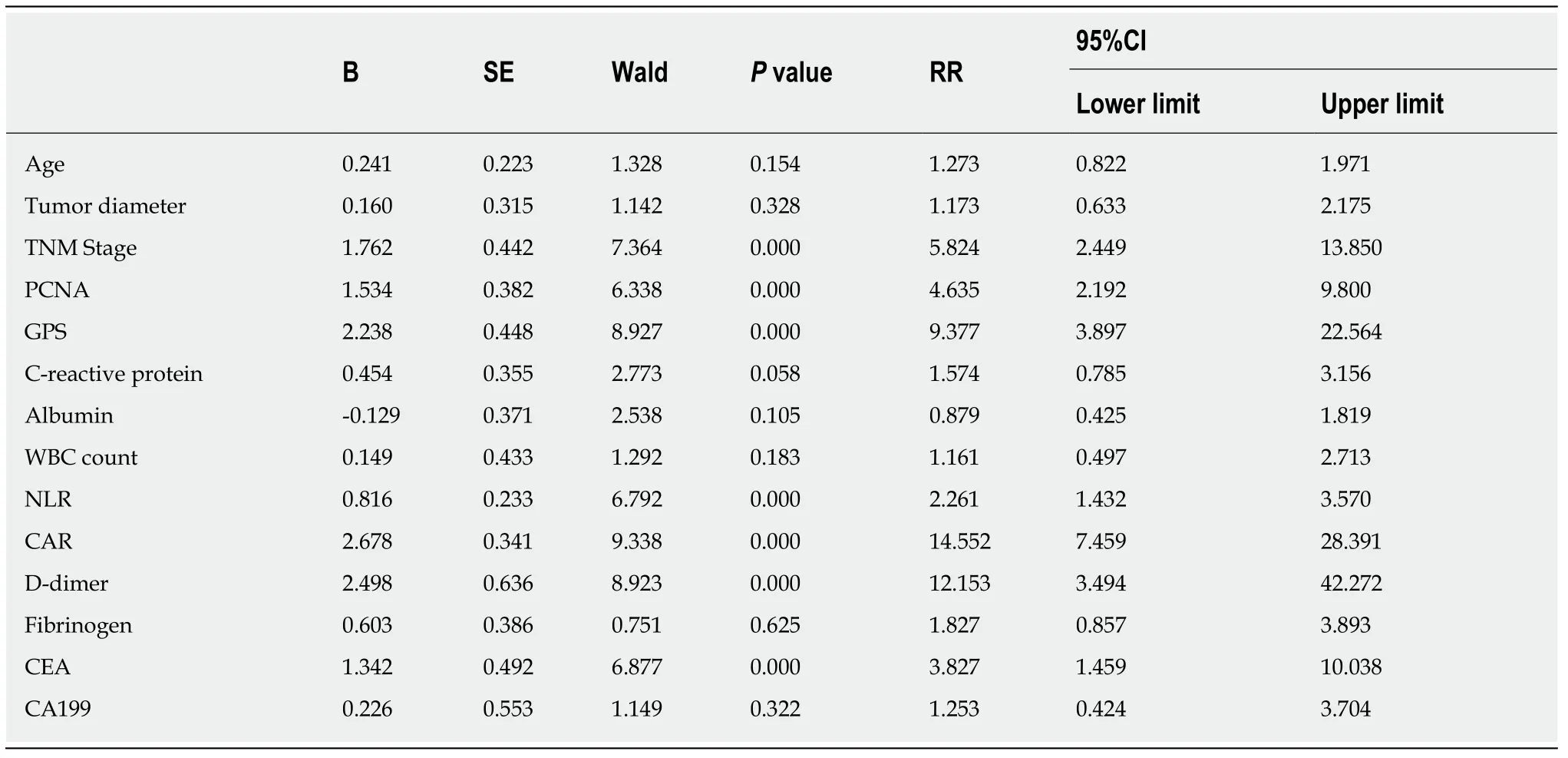
Table 2 COX regression analysis of influence factors on the prognosis of colorectal cancer

Table 3 Receiver-operating characteristic (ROC) curve analysis of potential indicators for predicting the prognosis of colorectal cancer

Figure 3 Receiver operating characteristic curve analysis of potential indicators for predicting the prognosis of colorectal cancer.
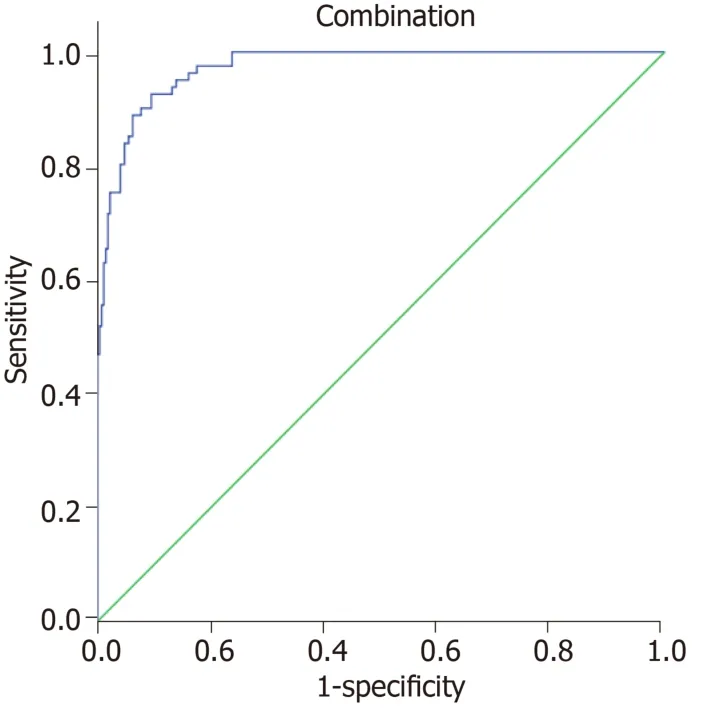
Figure 4 Receiver operating characteristic curve analysis of the combination assessment for predicting the prognosis of colorectal cancer.
ARTICLE HIGHLIGHTS
Research background
The prognosis of colorectal cancer is poor.Surgery is the main treatment for patients with colorectal cancer.Accurate assessment of surgical prognosis has an important impact on the choice of treatments for patients.Currently,there are many methods to evaluate the prognosis after colorectal cancer surgery,including tumor-node-metastasis (TNM) stage,Glasgow prognostic score (GPS) score and so on.However,the systematic analysis about the factors affecting the prognosis of col orectal cancer is still limited.
Research motivation
Currently,the prognosis of colorectal cancer is mainly predicted by carcinoembryonic antigen(CEA) level,pathological classification,and TNM stage.However,the accuracy of prediction cannot be guaranteed due to the influence of individual and environmental factors.Besides,studies have revealed that some inflammatory indicators are also related to the prognosis of cancer.
Research objectives
In this study,we analyzed the influence of clinical data,serology,and histology on the prognosis of patients with colorectal cancer,and assessed the accuracy of the combination of all indicators for the prognosis evaluation.The purpose of this study was to provide a new method for predicting the prognosis of colorectal cancer in the early stage.
Research methods
A total of 374 patients were recruited,and the patients were divided into a good prognosis group and a poor prognosis group.Relevant clinical indicators were recorded.The differences in clinical data,serology,and histology between the two groups were analyzed.Multivariate COX regression was used to analyze the independent influencing factors for the prognosis of colorectal cancer.The receiver operating characteristic curve was used to test the accuracy of different indicators and their combination for the prognostic evaluation of colorectal cancer.
Research results
The TNM stage,proliferating cell nuclear antigen (PCNA),GPS,neutrophil-lymphocyte ratio(NLR),C-reactive protein/albumin ratio (CAR),D-dimer,and CEA were independent influencing factors for the prognosis of colorectal cancer (P = 0.000).NLR,D-dimer,and GPS had the highest predictive power for colorectal cancer prognosis.But their accuracies were significantly lower than that of the combination of all indicators (AUC = 0.973; sensitivity,92.59%; specificity,90.51%).
Research conclusions
TNM stage,PCNA,GPS,NLR,CAR,D-dimer,and CEA are the independent influencing factors for the prognosis of colorectal cancer.Combined evaluation of independent factors is the most accurate method to predict the prognosis of colorectal cancer.
Research perspectives
On the purpose of avoiding the interference caused by the differences of individual and environmental factors,multi-center studies would be considered to enlarge the size of simple to improve the reliability of the research results.Besides that,long-term research is also planned to make up the ignorance of the factors affecting long-term prognosis in this study.
 World Journal of Gastrointestinal Oncology2019年12期
World Journal of Gastrointestinal Oncology2019年12期
- World Journal of Gastrointestinal Oncology的其它文章
- Current status of the genetic susceptibility in attenuated adenomatous polyposis
- Inflammatory pseudotumor-like follicular dendritic cell sarcoma: A brief report of two cases
- Deep learning with convolutional neural networks for identification of liver masses and hepatocellular carcinoma: A systematic review
- Multi-parameter ultrasound based on the logistic regression model in the differential diagnosis of hepatocellular adenoma and focal nodular hyperplasia
- Impact of regular enteral feeding via jejunostomy during neo-adjuvant chemotherapy on body composition in patients with oesophageal cancer
- Difference in failure patterns of pT3-4N0-3M0 esophageal cancer treated by surgery vs surgery plus radiotherapy
