Fanning the embers
Tinsley White Rucker
In a recent Annals of Family Medicine article,‘Colluding With the Decline of Continuity’, Dr John Frey was correct when he said, ‘Losing or designing away a focus on continuity of care in training and practice has real consequences for physicians and patients’.1He noted that lower hospitalisation rates, healthcare costs, patient trust and physician satisfaction are directly related to an ongoing relationship with a primary care physician. Unfortunately, family medicine struggles with recruiting applicants for training programmes and many graduated residents subspecialise in geriatrics, palliative care, women’s health, sports medicine,urgent care, emergency care, hospice care,hospital care and concierge care. Dr Frey asks if family medicine has now become part of the problem, not part of the solution. The larger question is whether family medicine can provide enough community-focused physicians to remain the backbone of primary healthcare in this country. Achieving this goal requires a fresh approach.
Public dissatisfaction with the state of medicine in 1969 led to the founding of family medicine as the 20th specialty in American medicine. Family medicine was more than a defined body of knowledge; it was a response to the public need for primary care that was comprehensive, accessible and continuous.2In an era of increasing subspecialisation,vertical integration, corporate medicine and increasing government intervention, it is still possible for family medicine to return to its roots and once again be a robust counterculture to reform medicine. With medical costs beyond the reach of many, the need for family medicine is more important today than it was in the 1960s. The key to success for family physicians is a willingness to step out of their comfort zones and to use their practices as laboratories of innovation to develop new and better ways to engage their patients and communities. Medical schools and their departments of family medicine should provide leadership for this effort by evaluating and addressing the needs of local indigent and rural communities. Medical students and residents should be part of this process.
University of Virginia (UVA) President Jim Ryan recently announced the university’s 10-year strategic plan and said, ‘In the future, universities will only be able to achieve true greatness by living their values and by adopting a broader view of their responsibility to employees, neighbours and society’.3Community access to healthcare is stressed in the plan. Departments of family medicine should be part of similar planning processes at their academic medical centres. Successful ideas and programmes can then be shared to the betterment of all. The CARE Clinic, a free clinic in Fayetteville, North Carolina, is one such success. The name CARE is an acronym for the four objectives of the clinic: compassion, assistance, referral and education.
HISTORY OF FREE CLINICS
In the 1960s, free clinics began appearing throughout the USA to care for those who could not afford traditional healthcare.4According to the National Association of Free and Charitable Clinics, there are now more than 1200 free and charitable clinics in the USA, and there continues to be a steady increase in patient demand despite full implementation of the Affordable Care Act.5An analysis of data collected by the National Health and Nutrition Examination Survey from 2007 to 2010 showed that US adults without health insurance coverage were more likely to use tobacco and to have poor fasting blood sugar, poor blood pressure control and poor level of physical activity. These findings were independent of age, sex and race.6The same study noted that community-level interventions may be the most effective intervention for the uninsured. Many studies have shown free clinics can significantly improve outcomes.7–9While free clinics are not the complete solution to complex issues of accessibility and affordability, they can help communities use their own unique resources and talents to supplement and augment the pre-existing healthcare system.

Table 1 Clinic visits (volunteer provided), 1993-2015
STARTING A FREE CLINIC
Local physicians and dentists had long cared for indigent patients in Fayetteville, North Carolina, but were hampered by the lack of a support network for laboratory tests, X-rays, medications and referrals. In 1992, Catholic Social Ministries arranged for Sister Jean Rhoads, a Daughters of Charity nurse, to come to Fayetteville to help establish a free clinic for the uninsured. Sister Jean put together a steering committee that evaluated the local uninsured situation, reviewed the literature and visited existing free clinics in Raleigh, North Carolina, Hilton Head, South Carolina, and Roanoke, Virginia. They concluded that a free clinic in Fayetteville was both needed and feasible.Eligible patients would be those without any insurance and a household income under 200% of the yearly adjusted federal poverty level. As a member of the initial steering committee and the volunteer medical director from 1993 to 2015, I was continuously impressed with how well the stakeholders—including four local hospitals, medical and dental providers, businesses, churches and civic organisations—worked together with one goal in mind: caring for our fellow residents. Over a quarter of a century later, the clinic continues to operate and has managed well over 100 000 clinic visits and referrals (table 1).10
FINANCING A FREE CLINIC
During an organisational meeting, board members were surprised when North Carolina State Senator Tony Rand recommended private fundraising because government grants could not be assured from year to year. He also said that private fundraising would ensure the clinic remained under local control. The CARE Clinic has continuously operated with mostly private and foundation funding,bolstered by three local fundraising events each year(table 2).10Provided services have never been charged to a patient or billed to a private or government insurance plan. Other than recent grants from the North Carolina Office of Rural Health, the clinic has never received government funding. Professional fundraisers have never been used because everyone involved actively participates in fundraising efforts. The executive director relentlessly seeks grants from nonprofit organisations, as well as otherdirect and in-kind contributions. Administrative and fundraising costs, from the start, have been kept under 16% of donated dollars, thanks to excellent business practices and a large volunteer staff.10
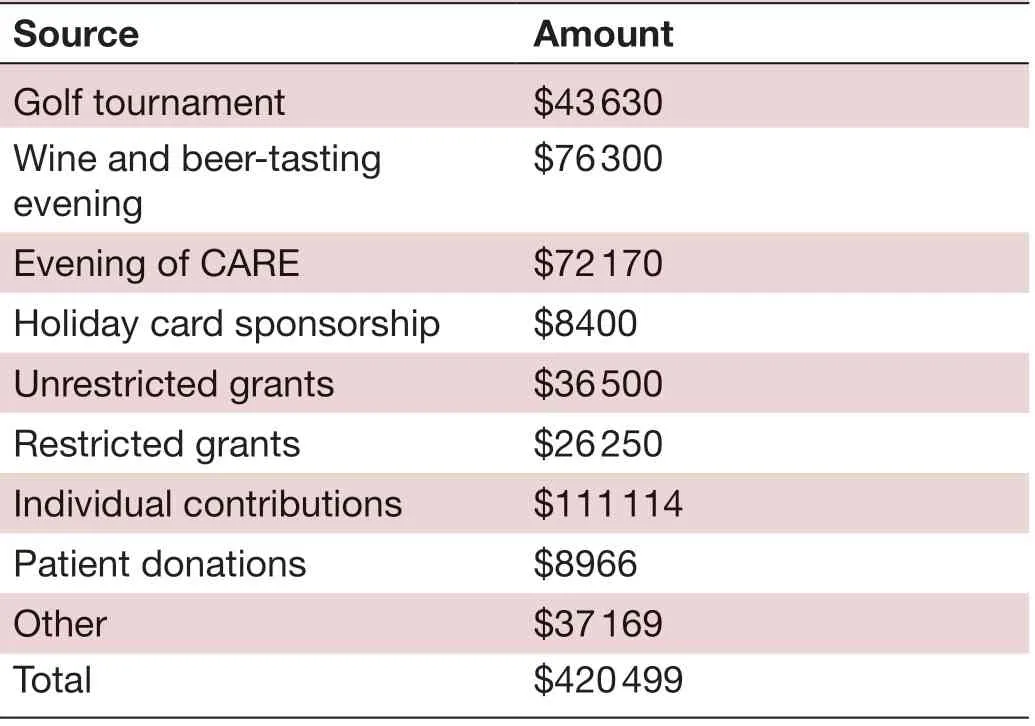
Table 2 2015 income (similar to previous years)
RECRUITING HEALTHCARE PROVIDERS
Providers and healthcare workers were recruited through outreach efforts to the healthcare community (table 3).10Presentations to medical and dental societies resulted in many physicians and dentists agreeing to either work in the clinic or accept referrals to their offices pro bono or at a reduced fee. New community physicians receive letters detailing the clinic’s mission. Several organisations, such as the Bangladesh Medical Association of North America,provide a significant number of volunteers and financial contributions. Nurses, social workers, dental technicians, nutritionists, chiropractors, laboratory technicians,pharmacists and other ancillary staff are recruited several ways: through presentations to churches, civic organisations, professional organisations, articles in the local newspaper and word of mouth.

Table 3 Volunteers, 1993-2015
The CARE Clinic found innovative ways to overcome regulatory barriers. Womack Army Medical Centre family medicine residents do their community medicine rotation at the clinic, enabling residents and their supervising physicians to work with out-of-state medical licences. They have worked in the clinic every Tuesday evening for more than 20 years. Physicians employed at Cape Fear Valley Medical Centre are covered under hospital malpractice coverage when working at the clinic. Medical Mutual of North Carolina, a medical malpractice insurance company, agreed that volunteer work done at The CARE Clinic would be covered by the clinician’s primary policy with the company. The clinic has a separate malpractice policy (with a tail-end clause) to cover any possible claim.To date, the clinic has not had a claim placed. These combined efforts increase the available physician staff.
The volunteer experience is important. Most volunteers work one evening clinic a month, and some have participated for over 20 years. Local churches donate evening meals, and volunteer clinic staff members ensure patients are ready to be seen when providers arrive. Compliance with provider plans is enhanced by readily available ancillary services, such as laboratory, X-ray, an onsite pharmacy and specialty backup. The clinic continues to have handwritten records augmented by a computer program for medication tracking. It is unrealistic to expect volunteers to learn another electronic record system. The volunteer medical director reviews and cosigns charts weekly for family medicine residents and midlevel providers. The medical director also reviews and initials all returned laboratory tests, radiological procedures and referrals. Letters of gratitude are regularly sent, and an annual appreciation dinner is held with awards given to outstanding volunteers. The local newspaper and other media outlets highlight key volunteers throughout the year. All these efforts prove helpful with recruiting and retaining clinician volunteers.
The CARE Clinic is an educational experience for future healthcare providers. Family medicine residents from Fort Bragg, medical students from nearby medical schools, students preparing for medical or physician assistant school and students at a nearby pharmacy programme rotate through the clinic. These future healthcare leaders see a wide diversity of patients and disease processes. They also learn how medical costs affect access to care and how community resources can be used to help people who fall through safety nets.
SUPPORT NETWORK
Clinic visits must be supplemented with a comprehensive network of ancillary services and specialists. Since The CARE Clinic was established in 1993, LabCorp has provided free routine laboratory tests. From 2012 to 2016,the total number of tests provided by LabCorp for CARE Clinic patients was nearly 12 000 (Williams J, personal communication, 2017). Routine X-rays and ultrasounds are provided at no cost by Cape Fear Valley Medical Centre and are read at no cost by local radiologists. Each facility in Fayetteville owning an MRI or CT scanner donates a few scans per month (table 4).10The limited pharmacy uses generic medications. From 1993 to 2015,147 357 prescriptions were provided.10For more costly medications, the Cumberland County Medication Access Programme completes paperwork for eligible patients who are then provided medication at no cost for 3 months,including refills. Many local specialists accept referrals in their offices at reduced or no cost. Four specialists(dermatology, orthopaedics, physical therapy and nutrition) conduct monthly clinics onsite. Two retired internists conduct weekly onsite clinics for chronic patients with diabetes and coronary artery disease. (table 5).10

Table 4 Total radiological procedures, 1993-2015
COMMUNITY BUY-IN
Community buy-in was initially achieved with presentations to churches, civic organisations, professional organisations, retired groups, local colleges, hospitals and the VA Hospital and local military organisations. Individuals from these groups served on the clinic board of directors. All believed in the mission of the clinic and were impressed by the low clinic overhead, which meant that 84% of donated dollars went to patient care.
PATIENT BUY-IN
Patient buy-in was achieved with outreach to local hospitals and the health department, as well as throughchurches, civic organisations and word of mouth. Patients were not charged but were asked to consider donating to help pay for the next patient. Patients sometimes became volunteers. Many patients continued their care there for more than 20 years.

Table 5 Most common referrals, 1993-2015
FANNING THE EMBERS
A recent survey of 2015 family medicine graduates had 2255 responses and confirmed the observation of Dr Frey about the decline of continuity in family medicine.11Survey results show 19% of respondents do not practice outpatient continuity care, 39% do not take after-hours call, 62% do not practice adult inpatient medicine, 86%do not deliver babies, only 8% practice in a community with a population under 20 000 and only 1% practice in a community under 2500. Significantly, 83% are fully employed and have no official ownership stake in their practice site. Surprisingly, 67% feel burned out at least a few times a month. Is this the future for family medicine?
With The CARE Clinic, I saw firsthand how healthcare professionals and community volunteers can work together to make a significant difference for their community. I also saw how future healthcare providers and leaders can be included in the process. When The CARE Clinic opened in 1993, most physicians in Fayetteville were in small private practices and saw involvement in a free clinic as a personal responsibility and obligation.The older physicians mentored this philosophy for new partners. Unfortunately, this professional mentoring may not be received by newly trained physicians, most of whom are now employed by hospitals, managed care groups and academic health centres.
On 18 April 2000, B. Lewis Barnett, Jr, MD, Emeritus Professor of Family Medicine, UVA School of Medicine,gave a presentation at the University of Oklahoma Health Science Centre titled ‘Live Coals and Embers’.12He spoke of the need for family medicine to fan the embers of idealism that are the soul of our profession and led my generation to choose this specialty many years ago.He said, ‘They should never be extinguished to satisfy the needs of modern medicine’. He stressed the need to simply listen to the patient and to ‘be there’ for them.According to Barnett, the shared existence between doctor and patient is special and is the antidote for burnout and dissatisfaction.
I currently work in a rural UVA School of Medicine family medicine clinic and regularly precept medical students and family medicine residents. They are as idealistic as my generation 40 years ago, and they want to make a difference. These future providers want and need to be trained and mentored in effective ways to use their clinics as laboratories of innovation for the development of new and better ways to engage their patients and communities.
For family medicine to remain the backbone of primary care in this country, family medicine residency programmes must take the lead by using all available community resources to provide accessible, affordable and continuous healthcare for their indigent and rural populations.This should be part of their core mission, and providers in training should be part of the process. Despite the best efforts to create a safety net through Medicare, Medicaid and other government programmes, there will always be people who will still be in need of assistance.
Now is the time to fan the embers of idealism that led to the founding of family medicine as a specialty in 1969.
AcknowledgementsSpecial thanks to Sister Jean Rhoads, DC, who helped bring a community together to address a community problem; Cathy Ory, the current Executive Director, who has been with The CARE Clinic from the beginning; Mr John Reichart, who collected the statistics; and the thousands of patients who were our partners in the success of The CARE Clinic.
FundingThe authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interestsNone.
Patient consent for publicationNot required.
Provenance and peer reviewNot commissioned; externally peer reviewed.
Open accessThis is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially,and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http:// creativecommons. org/ licenses/ by- nc/ 4. 0/.
 Family Medicine and Community Health2019年3期
Family Medicine and Community Health2019年3期
- Family Medicine and Community Health的其它文章
- Response to letter by Zhijie Xu: Why should mixed methods matter to primary care physicians a n d other providers?
- Study of type 2 diabetes management among patients in a Macau primary care setting
- Factors influencing the intention of Indonesian nursing students to work in rural areas
- Glycaemic control, antidiabetic medications and influenza vaccination coverage among patients with diabetes in Udine, Italy
- What do Iranian general practitioners expect from family physician contracts?
- Antimicrobial dispensing practices and determinants of antimicrobial resistance: a qualitative study among community pharmacists in Pakistan
