Experiences of new family physicians finding jobs with obstetrical care in the USA
Aimee R Eden, Tyler Barreto, Elizabeth Rose Hansen
ABSTRACT Objective This study aimed to explore how new family medicine graduates who want to include obstetrics in their scope of practice identify and select jobs and to understand how employment influences scope of practice in family medicine, particularly the ability to provide maternity care and deliver babies.Design Mixed-methods study including a survey and qualitative interviews conducted in 2017.Setting We electronically surveyed US family physicians and followed up with a purposeful subsample of these physicians to conduct in-depth, semistructured telephone interviews.Participants 1016 US family medicine residency graduates 2014-2016 who indicated that they intended to deliver babies in practice completed a survey; 56 of these were interviewed.Main outcome measures The survey measured the reasons for not doing obstetrics as a family physician.To identify themes regarding finding family medicine jobs with obstetrics, we used a team-based, immersioncrystallisation approach to analyse the transcribed qualitative interviews.Results Survey results (49% response rate) showed that not finding a job that included obstetrics was the primary reason newly graduated family physicians who intended to do obstetrics were not doing so.Qualitative interviews revealed that family physicians often find jobs with obstetrics through connections or recruitment efforts and make job decisions based on personal considerations such as included geographical preferences, family obligations and lifestyle. However,job-seeking and job-taking decisions are constrained by employment-related issues such as job structure,practice characteristics and lack of availability of family medicine jobs with obstetrics.Conclusions While personal reasons drove job selection for most physicians, their choices were constrained by multiple factors beyond their control, particularly availability of family medicine jobs allowing obstetrics.The shift from physician as practice owner to physician as employee in the USA has implications for job-seeking behaviours of newly graduating medical residents as well as for access to healthcare services by patients;understanding how employment influences scope of practice in family medicine can provide insight into how to support family physicians to maintain the scope of practice they desire and are trained to provide, thus, ensuring that families have access to care.
INTRODUCTION
With a growing obstetric provider shortage and maldistribution in the USA,1family physicians who provide obstetric care are crucial to ensuring access.2-4However, the declining number of family physicians including obstetric care in their practice has been well documented, and today, fewer than 10% of currently practising family physicians are delivering babies.5-7Researchers have identified significant gaps between training and practice of maternity care and between intention and practice of obstetrics. A recent study showed that while over 90% of 2013 family medicine graduates reported that they were adequately prepared in maternity care, just 25% of these physicians doing outpatient continuity care were providing any maternity care in 2016.8Of 2014-2016 family medicine graduates, 23% intended to include obstetric deliveries in practice, yet fewer than 10%were doing so.5
Many explanations for this decline have been considered, including cost of malpractice, lifestyle constraints, difficulty getting and maintaining privileges and inadequate training.9-15These reasons do not tell a complete story. Contrary to previous research,1015of 2013 family medicine residency graduates who were interested in delivering babies but who were not doing so in practice 3 years later (n=856), few reported malpractice costs (24%) or privileging challenges (15%) as barriers to doing deliveries.However, 60% indicated that there was no opportunity to do deliveries in the practice they joined,16raising questions about constraints placed on family physicians by employers or hospitals.
Shifts in physician employment, from practice ownership to becoming employees of hospitals or medical groups, have been documented over the past decades. The 2016 Survey of America’s Physicians found that just 33% of physicians identified as independent practice owners or partners, a significant decline from just 4 years earlier in 2012, when almost 49% were practice owners. Conversely, the 2016 data showed that 58% were employed either by a hospital or a medical group, up from 44% in 2012.17An analysis of the American Medical Association 2016 Physician Practice Benchmark Survey found that 50% of family physicians were employees rather than owners of the practices in which they worked.18The decline in practice ownership is underlined by evidence that in 2016,younger physicians are less likely to have an ownership stake in their practice (28% among physicians under the age of 40) than older physicians (55% among physicians age 55 and older), and correspondingly, younger physicians were more than three times as likely as older physicians to be employed by hospitals (14% vs 4%).18Employed physicians likely face different challenges than those practising in physician-owned offices, and it is unknown the extent to which employers might influence the scope of practice of family physicians. For new family medicine graduates seeking employment, it is unknown how the ability to practice full scope family medicine, including obstetrics, may be impacted by the organisational structure and culture of potential employers.
Previous studies have explored the characteristics of physicians who practice in rural areas1920and family physicians and residency programme characteristics for those who intend to provide maternity care.21None have investigated how broader health system shifts or other external factors may impact family physician ability to practice maternity care. Similarly, previous research has investigated how physicians choose their specialty post-medical school,22-26but to our knowledge, none have focused on how physicians identify and choose jobs post-residency,the factors that constrain and facilitate their decisions or their experiences in the process. This qualitative study aimed, in part, to better understand the complexities and experiences of finding a job that includes obstetrics as a family physician.
METHODS
This mixed-methods exploratory study, conducted in 2017, included a brief electronic survey and individual,semistructured interviews. A five-question survey was sent to all 2098 family physicians who graduated from residency between 2014 and 2016 who reported intention to include obstetric deliveries in practice on the American Board of Family Medicine (ABFM) Certification Examination Registration Practice Demographic Questionnaire (full survey analysis and findings have been reported elsewhere27). Family physicians in the same cohort who did not indicate intention to include obstetrics in practice were excluded from the study(n=7451). The data analysis for this paper was generated using SAS software (V.9.4).
The qualitative portion of the study included semistructured interviews with a sample of physicians who had responded to the survey and agreed to participate in a follow-up interview and provided contact information. Of those who agreed to be interviewed, we selected physicians who were and were not including deliveries in their current practice, aiming for a sample of half who were delivering babies and half who were not. To ensure we interviewed a diverse group, we purposefully identified physicians based on responses to survey questions: for those who were delivering, we recruited physicians who reported different volumes of obstetrical deliveries and for those who were not delivering, we recruited physicians who gave different reasons for not doing so. In all cases, we tried to ensure geographic variation in our sample: physicians practising in different regions, and accounting for rurality/urbanicity using Rural Urban Commuting Area codes associated with current practice address from ABFM demographic data.28We sent email invitations to a subsample to participate in an interview.
We used a semistructured interview guide that included questions about residency maternity care training, job-seeking strategy and decision-making,experience obtaining hospital privileges and malpractice insurance and current practice scope and structure.This paper focuses on questions about how physicians found their current position and how they made the decision to apply for and take their current position.Experienced researchers (AE, TB, EH) conducted 45-60 min interviews by telephone. Interviews were recorded and professionally transcribed. Informed consent was obtained from each participant prior to conducting the interviews.
The ‘immersion-crystallisation’ approach, which involved cycles of concentrated textual review of data,was applied to first code data using a priori codes aligned with the interview guide and based on previous research, and to generate emergent codes as they arose in through the iterative process.29We then subcoded where the original coding was too broad to make sense of physician experience or where further nuanced themes or patterns were identified. Where possible, we grouped codes into meaningful categories to further organise the data and identify patterns and themes. We employed qualitative data analysis software, MAXQDA software (V.2018, VERBI Software, Berlin, Germany),to manage the coding process. The authors met on a weekly basis to ensure inter-rater agreement. In the early phases of data analysis, all three team members(AE, TB, EH) coded the same interviews independently,meeting regularly to compare coded segments to ensure uniformity and to discuss and refine the codes and code definitions. We were consistently applying the codes after seven independently coded interviews, after which we divided the remaining interviews among us to code,continuing to meet weekly to discuss questionable or newly emerging themes. All interviews were fully coded using our final codebook, though after 18 interviewshad been coded, no new themes were identified, indicating that we had reached thematic saturation.

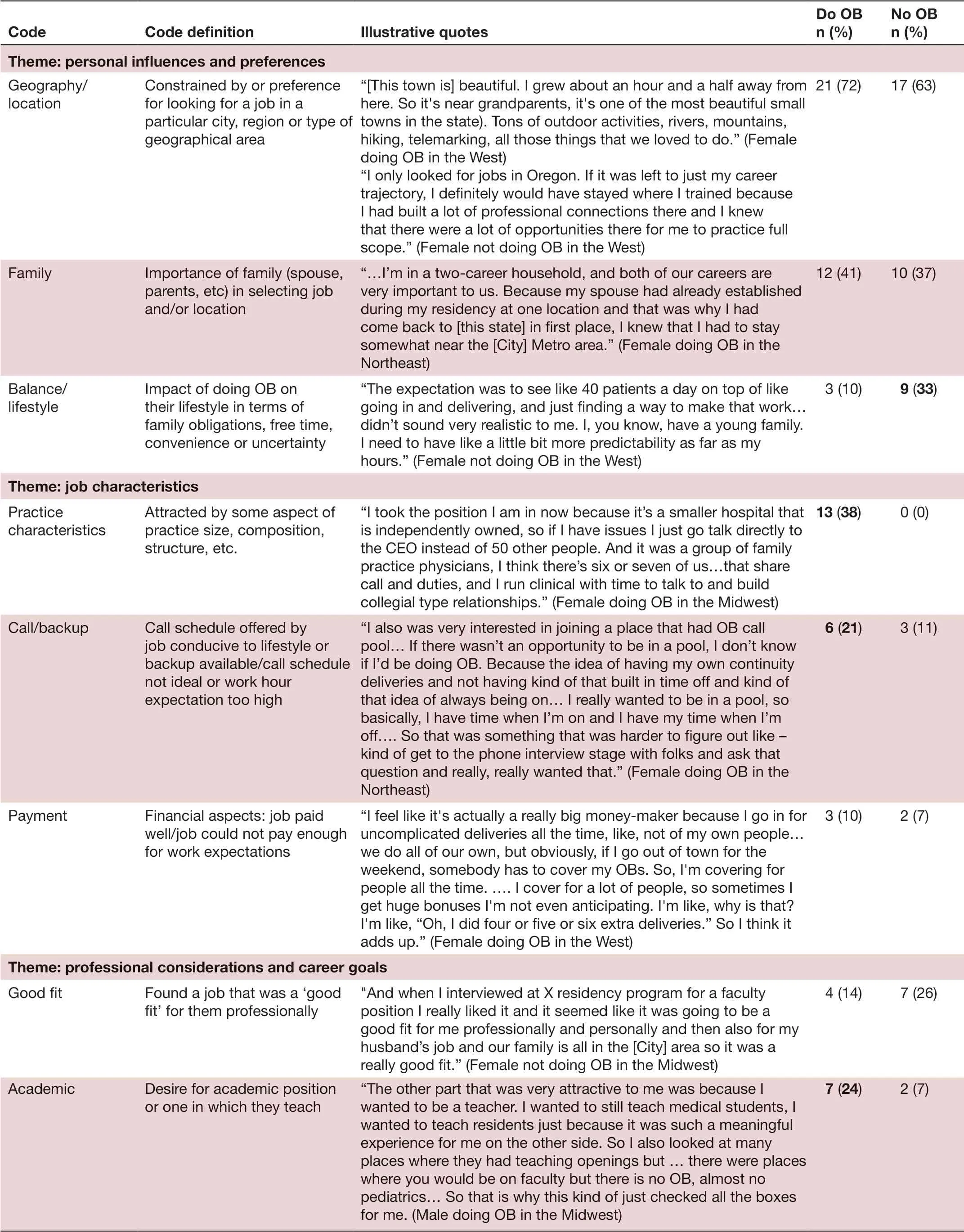
TabIe 1 Personal and practice characteristics of interviewees by provision of obstetrical deliveries
RESULTS
Of 1016 survey respondents (an almost 50% response rate),31% reported they are not currently including obstetric deliveries in their practice; of these 41% reported that finding a job without OB was in the top three reasons for not currently practising obstetrics; 26% reported it as the number one reason. Of the physicians who completed the five-question survey, 56% (n=565) indicated willingness to be interviewed. While those currently including obstetric deliveries were significantly more likely to agree to be interviewed than those not including obstetrics (63.7%and 40.5%, respectively, p<0.001); we interviewed (N=56)a balanced sample from each group, 29 currently delivering babies and 27 not currently delivering babies. Table 1 includes demographic information about the interviewees(more detailed survey findings are reported elsewhere27).The themes that emerged from the interviews regarding identifying and selecting a job post-residency fell into three primary categories: the mechanism through which family physicians identified a job (how they found a job);the factors that went into decisions around identifying and taking a job (why they took a job); and challenges faced by family physicians when trying to find a job including obstetrics.
Job identification mechanism
Interviewees discussed various mechanisms through which they identified jobs (figure 1), including connections (personal contacts or professional connections such as an advisor or mentor), recruiters or recruitment agencies, word-of-mouth or online (including National Health Service Corps listings, state level listings or other online job search formats). Five family physicians were military,so their placements were assigned for them, with generally minimal physician control over job scope; four of them were not currently doing deliveries. Connections,whether personal or professional, were the most common mechanism for identifying a job for family physicians doing and not doing deliveries. However, more physicians doing deliveries discussed connections helping them to identify a job than those not doing deliveries. The use of recruiters or recruiting agencies was the second most commonly discussed mechanism for finding a job;however, only 11 physicians mentioned this method.
Job decision-making factors
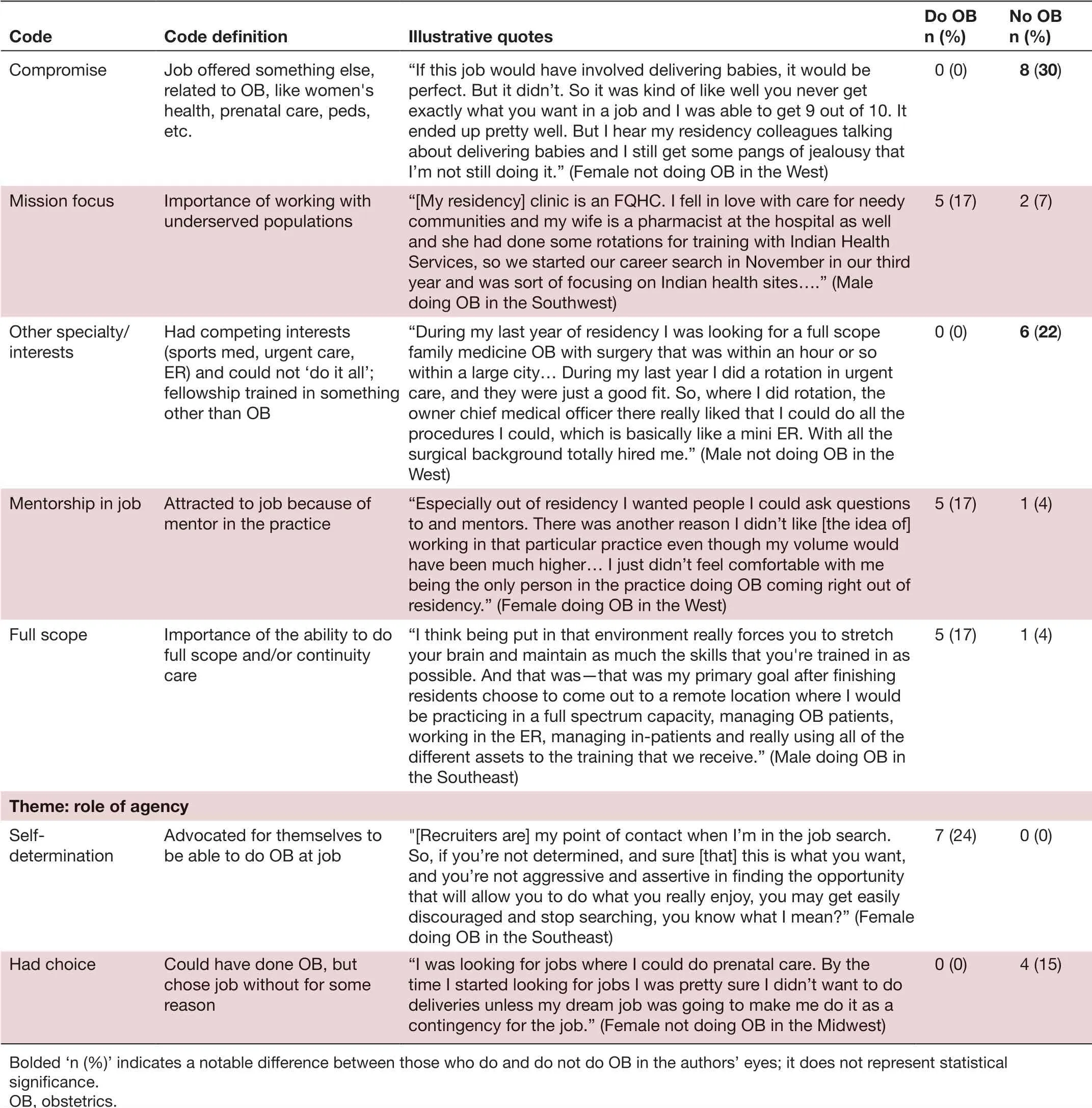
The reasons physicians gave for taking a job were nuanced and often interrelated. These factors were grouped into four themes, described below and defined in table 2 with corresponding illustrative quotes.
Personal influences and preferences
By far, personal influences were the most frequently expressed considerations for taking a job, including geography or location, family and lifestyle or balance. Both family physicians doing deliveries and those who were not mentioned location as a key constraint or consideration,whether looking for a job in a particular city, region or geography. Similarly, family or spousal influences were discussed equally by physicians doing and not doing deliveries. Often, family considerations drove the geographical choice.
Job characteristics
Issues directly related to the job structure or other job characteristics, which interviewees did not perceive to be open for negotiation or under their control, came up in many interviews. For physicians doing obstetrics, practice features (size, structure, composition) were an important factor in deciding to accept a job, as was a call schedule conducive to their lifestyle. When call was discussed by those not doing obstetrics, it was in the context of non-ideal call schedules or lack of a call sharing method.A few physicians mentioned financial considerations such as getting paid enough or too little to include obstetrics in their practice.
Professional considerations and career goals

Figure 1 Job identification mechanism: themes and illustrative quotes. OB, obstetrics.
Individual professional considerations also contributed to job search and choice for many physicians. While related to job characteristics described above, unlike fixed job factors, these elements were characterised by a sense of control over their own career path. Some physicians not doing obstetrics discussed making a compromise of giving up obstetrics while retaining the ability to do other rewarding and related work, such as abortions, women’s health, prenatal care or paediatrics. Another group indicated that other competing professional interests drove their decision to take a job without obstetrics. These physicians had done fellowships or had strong residency training in urgent care, sports medicine or emergency medicine and claimed that they could not ‘do it all’.Physicians doing obstetrics sometimes discussed professional considerations such as the ability to practice full scope family medicine as a driver in considering a job.Those doing obstetrics were also more likely to discuss being mission focused, to want to work in an academic setting and to seek mentorship in their job.
Role of agency
A small number of physicians indicated that personal agency played a role in selecting their job. Agency is the capacity as an individual to act independently, to make their own free choices and thus demonstrate individual power.3031Agency arose in different ways for those who were doing obstetrics compared with those who were not.Seven family physicians doing obstetrics discussed assertiveness or self-advocacy in asking for obstetrics to be part of their job. Four physicians who were not doing obstetrics indicated that they could have done so, either in their current job or in their current location, but chose not to or chose a job without obstetrics.
Challenges
Family physicians who were not currently including obstetrics in practice, as well as those who were, discussed the various ways in which it was difficult to identify or obtain a family medicine job with obstetrics (table 3). Nine physicians doing obstetrics and eight of those not encountered a lack of availability of jobs with obstetrics in the vicinity of their search. Some were told there were no jobs with obstetrics available, others were actively discouraged by recruiters or employers. Relatedly, physicians described the challenge of needing to overcome the perception or belief that family physicians do not do obstetrics.
Another challenge faced by family physicians wanting to do deliveries in practice included a ‘bait-and-switch’offer from an employer that made the physician think that they would be able to do deliveries, but once they were working in the position, they realised that they could not do obstetrics. When newly graduating family physicians took jobs that did not include obstetrics (often taking temporary jobs or doing locums), it became nearly impossible for them to later do obstetrics. Nine of our interviewees not doing obstetrics described a loss of skill or confidence in their ability to do obstetrics as a barrier;two of these described residency programme failure in adequately training or advising.
Almost none of the interviewees identified malpractice as a barrier to doing deliveries. On the contrary, a female physician not doing obstetrics in the West said:
TabIe 2 Job decision-making for new family physicians who intend to do obstetrics: themes and illustrative quotes
TabIe 2 Continued
It wouldn’t be a reason for me to not do it [obstetrics], because if I were to do it, it would be through some larger organization that would take care of the malpractice and liability.
Another female physician doing obstetrics commented:…they cover all of our malpractice; like all of us who do anything but certainly it includes all of us who do OB. … the clinic just does that, like it was never an issue, like it was never anything that was even discussed. It was always covered.
While credentialing took some time and effort for most family physicians doing obstetrics, it was generally not discussed as an unreasonable or significant challenge. For example, a physician in the Midwest commented on the privileging process:
It was actually quite extensive, and we had to do 20 observed C-sections before they would give us full privileges. They required an attending during those surgeries. They had to approve our operative logs and submit those from residency and as well as vaginaldeliveries to be able to get privileges. I also believe that the physician we trained under the most had to write a letter of recommendation as well.… [But] I thought it was reasonable. The last thing that you really want is someone who says they can do something that they can’t.

TabIe 3 Challenges finding family medicine jobs with obstetrics: themes and illustrative quotes
DISCUSSION
Interviews with early career family physicians who intended to include maternity care in practice demonstrated that they identified and chose jobs after residency in complex and multifactorial ways, with the ability to do obstetrics being one of many factors. Their job-seeking behaviours and choices were constrained by both personal factors as well as larger institutional and systems level factors. In terms of finding a job with or without obstetrics after graduation, besides personal considerations like location and family,different themes emerged from physicians currently practising obstetrics versus from physicians not practising obstetrics.
Our interviews confirmed previous research that identified geographical location, personal time and lifestyle as the primary considerations for residency graduates when identifying a job.32However, the nuances of what lifestyle and personal time really mean to physicians and how larger contextual factors like job and practice characteristics play a role in those have not been addressed in the existing literature. Our study showed that geographical location, family or spousal influence and lifestyle considerations were important to most physicians when searching for and accepting a job, but practice characteristics and job structure can mediate these. For example, a job that offers call sharing that reduces scheduling uncertainty can reduce negative impacts on lifestyle and family obligations. For many family physicians, a job structured to support work-life balance is necessary for them to include obstetrics in their practice.
Recruitment of family physicians who do obstetrics was not a common theme among our participants, despite a survey of medical residents that showed they are intensely recruited, with 89% contacted by recruiters from hospitals, medical groups or recruiting firms at least 10 times during training.32When recruitment was brought up by our interviewees, it was sometimes portrayed as a barrier rather than a facilitator in finding a job that includes obstetrics, indicating that recruiters may not be the best way for family physicians to identify full-scope jobs with obstetrics. It also suggests that employers who choose to use recruiters might better educate the recruiters to fill family medicine-obstetrics positions.
Physicians’ freedom to make decisions about what job to take may be constrained by a multitude of job-related issues and professional and personal constraints. Thus, agency and self-efficacy to advocate for desired job scope that includes obstetrics within existing structures is one way family physicians who want to do obstetrics may be able to navigate the system without making professional compromises. Ideally,however, professional and job-related constraints should be minimised so that full-spectrum practice is possible in geographical locations where physicians want and/or need to be given their personal constraints.
This study has several limitations. The sample first self-selected by taking the short survey and further self-selected by agreeing to participate in an interview. It is possible that physicians who did not complete the survey or did not agree to be interviewed had different kinds of experiences than those who made up our interview sample. In addition, because the survey and interview participants were at most 3 years from residency graduation, their experiences only reflect those of early-career physicians, whose careers are not always yet stable. Several interviewees had already changed jobs since graduating.
CONCLUSIONS
Our findings suggest ways that residency programmes and employers can better support family physicians in maintaining the scope of practice they desire. A recent survey showed that 56% of residents had not received formal career or business instruction, and another study demonstrated the value of formalised career advising for medical students, which may be extended to residency graduates.3233Supporting our finding that connections play an important role in identifying desirable jobs, a study on how physicians search for jobs found that 88% of surveyed physicians rated personal or professional referrals as useful in their search for a job.3234Given the challenges of finding jobs that not only include obstetrics but support balance, a more deliberate approach to career advising and a more active role by academic faculty to connect new physicians to jobs with obstetrics may increase the number of family physicians including obstetrics in their practice.
Our data suggest that while employers can alleviate certain challenges faced by family physicians doing obstetrics as cited previously in the literature (by providing malpractice insurance and covering its cost and having a system in place to assist in the privileging process), the physician employment trend may negatively impact physicians looking for jobs that include obstetrics by restricting their ability to do so due to an unfriendly family medicine-obstetrics culture, or if practice characteristics and job structure are not supportive.Employers can further support family physicians who want to include obstetrics by improving call sharing structures and implementing other organisational changes that support work-life balance.
Key points
Question
►How do new US family medicine graduates who want to include obstetrics in their scope of practice identify and select jobs?
Finding
►While newly graduating US family physicians make job decisions based on personal considerations such as geographic preferences,family obligations and lifestyle, their job-seeking and job-taking decisions are constrained by factors beyond their control, such as job structure, employer/practice characteristics and lack of availability of family medicine jobs with obstetrics.
Meaning
►The shift from physician as practice owner to physician as employee in the USA has implications for job-seeking behaviours of newly graduating medical residents. Because employment influences scope of practice in family medicine, particularly the ability to provide maternity care and deliver babies, it is important to address employer-related barriers.
AcknowledgementsThe authors would like to thank Lars Peterson for reviewing drafts and providing insightful feedback and Audrey Brock for editing and formatting assistance. We greatly appreciate our participants’ time and thoughtful responses to our many questions. Aimee Eden had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
ContributorsAll authors contributed to research design, data collection, data analysis and/or writing the manuscript.
FundingMaterial support was provided by the American Board of Family Medicine.
Competing interestsTwo authors are or were employed by the ABFM during data collection and analysis: ARE and ERH.
Patient consent for publicationNot required.
Ethics approvalThis study was approved by the American Academy of Family Physicians Institutional Review Board.
Provenance and peer reviewNot commissioned; externally peer reviewed.
Open accessThis is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially,and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http:// creativecommons. org/ licenses/by-nc/4.0/.
 Family Medicine and Community Health2019年3期
Family Medicine and Community Health2019年3期
- Family Medicine and Community Health的其它文章
- Response to letter by Zhijie Xu: Why should mixed methods matter to primary care physicians a n d other providers?
- Study of type 2 diabetes management among patients in a Macau primary care setting
- Factors influencing the intention of Indonesian nursing students to work in rural areas
- Glycaemic control, antidiabetic medications and influenza vaccination coverage among patients with diabetes in Udine, Italy
- What do Iranian general practitioners expect from family physician contracts?
- Antimicrobial dispensing practices and determinants of antimicrobial resistance: a qualitative study among community pharmacists in Pakistan
