Review of abdominal solid organ transplantation in Jehovah's Witness patients
Rodrigo S Figueiredo, Rohan G Thakkar, Paul R Ainley, Colin H Wilson
Rodrigo S Figueiredo, Rohan G Thakkar, Paul R Ainley, Colin H Wilson, Department of Hepatopancreatico-biliary and Transplant Surgery, Freeman Hospital, Newcastle upon Tyne NE7 7DN, United Kingdom
Abstract
Key words: Anaemia; Blood transfusion; Informed consent; Jehovah's Witness;Transplantation
INTRODUCTION
Due to the doctrines of their faith, Jehovah's Witness (JW) patients will not accept transfusions of red blood cells, white blood cells, platelets or plasma, even if that is required to save their lives.This belief originates from a few biblical quotations, the most pertinent being, “You are to abstain from food sacrificed to idols, from blood,from the meat of strangled animals, and from sexual immorality”[1].In addition to not accepting the four main constituents of blood, decisions on other fractions of blood are a matter of personal choice dependent on their conscience.Critical to their adherence to this is their belief in apocalypticism, whereby armageddon is imminent.Thus, according to the Watch Tower publication, blood transfusions “may result in the immediate and very temporary prolongation of life, but at the cost of eternal life for a dedicated Christian”[2].
The limitations on transfusion, understandably lead to apprehension in performing complex surgical procedures in JW patients, as it would inherently carry an increased risk.It is therefore essential that patients are adequately assessed pre-operatively, any strategies for optimisation of haemoglobin are adopted, and a thorough discussion is undertaken with the patient to determine exactly what blood products and blood conservation technologies they will accept (Table 1).There are individual case reports and small series published on experience with solid organ transplantation in JW patients and the strategies adopted to facilitate that.
PRE-OPERATIVE ASSESSMENT AND OPTIMISATION
JW patients, who undergo major abdominal surgery such as solid organ transplantation without a blood transfusion, are likely to suffer a period of transient anaemia, which could potentially be profound depending on surgical blood loss.A patient's fitness to withstand this should be assessed pre-operatively, in particular with regards to cardio-respiratory reserve.One option would be to perform cardiopulmonary exercise testing or a cardiac stress test.Provided they are assessed to be fit enough to withstand transient severe anaemia, one must also ensure that the patient's haemoglobin is at an adequate level pre-operatively.Certainly, operating on JW patients who are already anaemic should be avoided except in emergency situations.
Standard options utilised in other areas of medicine to increase haemoglobin concentration can be adopted pre-operatively, but will often take several weeks to have their full effect.These include recombinant human erythropoietin (RhEpo), iron,B12 and folic acid.The use of RhEpo is particularly useful although patients must be aware of the risks associated with infusion, including the risk of sudden death due to anaphylaxis[3].Also, some formulations of RhEpo are suspended in human albumin,and therefore this should be specifically discussed with JW patients.Iron can be supplemented orally or intravenously (IV), although IV infusion is associated with relatively high rates of anaphylaxis and hypersensitivity reactions[4].Vitamin B12 and folic acid supplementation provide a more subtle increase in haemoglobin, but are useful adjuncts.
PLASMA DERIVATIVES
Cryoprecipitate
Standard cryoprecipitate supplied by National Health Service Blood and Transplant contains Factor VIII: C, von Willebrand Factor, fibrinogen, Factor XIII and fibronectin and is produced by further processing of fresh frozen plasma (FFP)[5].As such, it provides a multi-modal approach as a rescue therapy to minimise or control bleeding.The most common uses for cryoprecipitate are disseminated intravascular coagulation(DIC), liver disease or other causes of hypofibrinogenaemia.It has been used in JW patients undergoing cardiac surgery but not solely, making it difficult to appraise its individual effect[6].It is not appropriate to use cryoprecipitate in prophylaxis of bleeding if the patient is not depleted in coagulation factors.
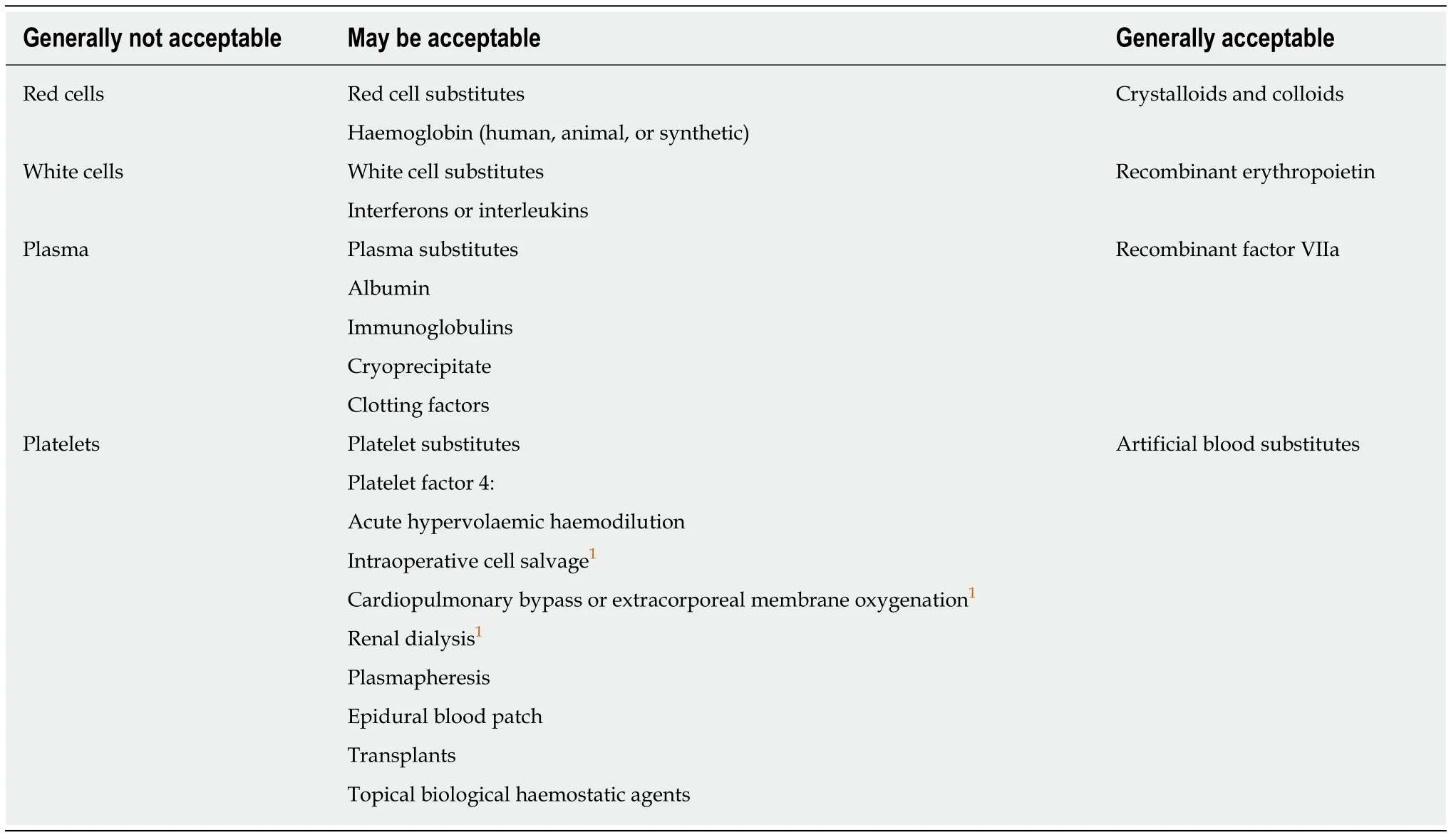
Table 1 Acceptability of different products by Jehovah's Witnesses
Fibrinogen concentrate
Fibrinogen concentrate is produced from pooled human plasma.It is used primarily in cases of congenital hypofibrinogenaemia but is also used for treatment of bleeding when there is an acquired deficiency such us in liver failure or DIC.It has advantages over FFP and cryoprecipitate for replacement of fibrinogen in that it is stored as a powder, with a standard dose, at room temperature.This can quickly be reconstituted in small volumes and does not require ABO cross matching.Furthermore, during manufacture, viral inactivation steps are commonly carried out.These characteristics allow more accurate dose administration and reduce risk of fluid overload,transfusion related acute lung injury and risk of viral infection when compared to FFP and cryoprecipitate.An observational study found it to be as efficacious as cryoprecipitate in massive obstetric haemorrhage[7].Additionally, it is also associated with a significant reduction in red cell loss, FFP and platelet administration[8].Its highly refined manufacturing process may make it more acceptable to JW patients (it can be used to treat dilutional coagulopathy when high volumes of crystalloids/colloids are used to restore circulating volumes).
Coagulation factors
Coagulation factor replacement therapy may be in the form of single factor concentrates or prothrombin complex concentrates (PCC).PCC will be discussed below.Single factor concentrates may be either plasma derived or produced through recombinant DNA techniques.Factors VII, VII, IX and XIII are used most commonly to treat patients with haemophilia or other inherited coagulation factor deficiencies.Plasma derived factor concentrates are produced from pooled plasma by chromatography and undergo viral reduction.As they originate from human blood,they are not accepted by all JW patients, but this is left to personal decision.More recently, coagulation factors have been produced using recombinant DNA techniques,and these have been more widely accepted by JW patients.
Due to the reduction of coagulation factors through large volume blood loss, there is a role for their replacement in the bleeding patient.Factor XIII, for example, may be administered to improve clot stability.Prophylactic use of factor IX concentrate has been described for use in the JW patients undergoing complex cardiothoracic surgery in combination with other therapies such as acute normovolaemic haemodilution[9].Use of recombinant factor VIIa has been reported in JW patients receiving liver transplantation, and studies have shown it to be beneficial in controlling bleeding during surgery or trauma[9,10].
Prothrombin complex concentrates
PCC contain a mixture of vitamin K dependent proteins.They are produced through further refinement of cryoprecipitate following the removal of anti-thrombin and factor XI.PCC can be found in three factor (II, IX and X) and four factor (II, VII, IX and X) concentrates.Originally developed for treatment of haemophilia, it is now most commonly used to reverse warfarin.PCC may be used to treat dilutional coagulopathy resulting from use of crystalloids to maintain circulating volume following massive blood loss.Like fibrinogen concentrate, the refinement process of PCC may make it more acceptable to JW patients; it can be kept in the pharmacy rather than blood bank.It has shown to be effective along with cryoprecipitate in cardiac surgery[6].
The main risks associated with the use of PCC are increased incidence of thrombotic events such as stroke, myocardial infarction and pulmonary embolism.These risks, however, are low and reduced further by the inclusion of therapeutically effective levels of protein S and C as well as the reduction in the use of activated coagulation factors.Unlike FFP, PCC is not associated with the risk of transfusion related acute lung injury as antibodies associated with this are removed during its production.
Intravenous immunoglobulins (Anti-D)
IV immunoglobulins (IVIg) are derived from plasma pools of thousands of screened donors and are highly refined through use of cold alcohol fractionation and ion exchange chromatography.They are used in the treatment of primary and secondary immune deficiencies as well as autoimmune inflammatory conditions.The use of antihepatitis B hyperimmunoglobulin became standard practice in the 1990s to reduce recurrence of hepatitis B in liver transplant patients[11].Increasing numbers of studies have shown improved survival rates and reduced levels of graft dysfunction and rejection in patients receiving IVIg[12].These benefits are thought to be due to more than simply the clearing of pathogenic antibodies.Although not completely understood, it is believed that IVIg provides a combination of immune-supporting and immuno-suppressive properties.
Amongst these immune-modulatory properties, IVIg has been seen to reduce circulating levels of pro-inflammatory cytokines, such as tumour necrosis factor,whilst upregulating anti-inflammatory cytokines, for example interleukin 11.It has also been found to interfere with the maturation and differentiation of dendritic cells,which are associated in the pathogenesis of allograft rejection[11,12].IVIg have been included in protocols to desensitize patients prior to ABO incompatible transplants to be performed.Studies looking at this approach have been small, but evidence available indicates significant improvement in outcome with use of IVIg in ABO incompatible liver transplant[13].
DRUGS
Aprotinin
Aprotinin is an anti-fibrinolytic molecule that has been used to reduce bleeding in major surgery.Its usage was fairly widespread in liver and heart surgery prior to a study demonstrating increased mortality[13].Following this, its distribution was temporarily suspended, but the European Medicines Agency recommended lifting this suspension in 2012[14].Dosage described for use in JW patients for prevention of excessive blood loss is 2000000 KIU, followed by 500000 KIU/h[15].
Tranexamic acid
Tranexamic acid is a synthetic analogue of lysine and has anti-fibrinolytic actions.Some areas of medicine have adopted fairly widespread use of tranexamic acid,including trauma and obstetrics.There are case reports on the use of tranexamic acid specifically in JW patients in combination with other strategies[16-20].
Desmopressin
Desmopressin is a synthetic replacement for vasopressin.It has a variety of uses, but in the case of JW patients is useful as it stimulates the release of von Willebrand Factor, and has been used to facilitate major surgery in JW patients[21].However,caution should be used to avoid significant systemic hypotension[22].
Red cell substitutes
No red-cell substitute is yet available for widespread clinical use, although some perfluorocarbons have been used in trials.Blood substitutes may be derived from human haemoglobin, in which case JW patients may not accept them.
TOPICAL BIOLOGICAL HAEMOSTATIC AGENTS
A variety of topical preparations are available on the market to stop or minimise bleeding intra-operatively.These often contain human plasma derivatives, which should be discussed with the patient.
Cellulose pads
Cellulose-based agents are formed into mesh, gauze or sponges.In the presence of blood, it forms a gelatinous mass similar to a synthetic clot, helpful for haemostasis.An example is Kaltostat (ConvaTec, Greensboro NC, United States), which also has antimicrobial properties.
Fibrin glues and sealants (Tisseel)
These are often available in pre-filled syringes or vials for mixing.They are effective either over a broad surface such as a cut liver or a specific bleeding point.Tisseel(Baxter Healthcare, Deerfield IL, United States) consists of two components - a sealer containing human fibrinogen and a synthetic anti-fibrinolytic (aprotinin) and a human thrombin solution.
Collagen
Sponge matrices embedded with human fibrinogen and/or thrombin, such as Vitagel(Stryker, Kalamazoo MI, United States) are also available.In addition to the active biological component, they promote platelet aggregation and provide a framework for thrombus formation.This is particularly effective if the patient is on antiplatelet therapy.
BLOOD CONSERVATION TECHNOLOGIES
Most JW patients feel that the external tubing of a cardiopulmonary bypass circuit,dialysis tubing or cell salvage equipment is an extension of their own circulation, as long as an unbroken circuit is maintained.
Cell salvage
Cell salvage is generally acceptable to JW patients, although again should be explicitly discussed pre-operatively.A small number of JW patients will only accept cell salvage if continuous auto-transfusion is performed and will not accept batched preparation for transfusion.However, most feel that so long as a continuous circuit is maintained,batched preparation is acceptable.A number of machines are available for cell salvage(e.g., Haemonetics Cell Saver, Munich, Germany), although to our knowledge only the CATS machine by Fresenius AG (Bad Homburg, Germany) provides continuous autotransfusion.
There are some limitations to the use of cell salvage, such as the presence of malignant or infective sources.If either of these are present, then auto-transfusion into the systemic circulation may well be detrimental to the patient.In small bowel or pancreas transplantation, cell salvage should be stopped at the time that the small bowel is opened.If liver transplantation is being performed for hepatocellular carcinoma, one could argue against its usage, but a balanced approach to the risks is required.
Acute normovolaemic haemodilution
This is a blood conservation strategy employed by anaesthetists at the time of surgery,whereby between one and three units of whole blood are drained from the patient in the anaesthetic room, and an equal volume of crystalloid or colloid is replaced into their circulation.These units of whole blood can then be transfused to the patient during or after surgery.However, most JW patients will only accept this if the bags of blood and tubing remain connected at all times (closed circuit)[23].This is particularly useful in patients with a high pre-operative haemoglobin.
ALTERNATIVE STRATEGIES
Whole-body cooling has previously been performed to reduce oxygen consumption and thereby allow permissive anaemia.However, this is no longer recommended due to other detrimental effects, including coagulopathy, impaired wound healing and increased wound infection rates[24].Hypotensive anaesthesia has been shown to reduce blood loss in major surgery[25]; however, its use remains controversial.Hyperbaric oxygen has been utilised on a few occasions as a rescue therapy in extreme anaemia to reverse tissue hypoxaemia[26,27].However, there are obvious logistical limitations to this.
CONSENT
Although some doctrines are fixed within the JW faith, some beliefs relevant to blood products are more variable from person to person.It is therefore essential to take the time to have a detailed, frank discussion with the patient about their beliefs.Ideally, a specific standardised consent form should be utilised for JW patients undergoing surgery, in which they must declare whether they will accept or decline each of the blood products or interventions detailed above.This consent process should be performed in the presence of an independent witness, and the patient may wish to discuss the issues with the Elders of the Witness community or consult the JW Hospital Liaison Committee, who often provide a useful intermediary role.No assumptions should be made, and it is important to ask candidly whether they will truly wish to decline a blood transfusion even if it costs their life.Eventualities should be discussed, in the event that they later need further procedures or interventions and are not fit to consent (e.g., renal dialysis whilst unconscious).
PUBLISHED EXPERIENCE
Liver transplantation
A number of case reports and series have been published demonstrating experience in liver transplantation in JW patients.The first published case of successful liver transplantation in a JW patient without the use of blood products was in 1996[28].The added complication in liver transplantation is the fact that many patients requiring a transplant may be coagulopathic, have portal hypertension or thrombocytopaenia.
Jabbouret al[29]published the largest series of liver transplantation in JW patients,with 27 transplants over a 5-year period.Pre-operative management included RhEpo,iron and folic acid for blood augmentation.Intra-operatively, cell salvage was used in all patients, and all living donor recipients had also had acute normovolaemic haemodilution.They reported two deaths, one from primary non-function, and the second died from severe anaemia and coagulopathy[29].Another series included nine patients in Liege, Belgium, where cell salvage and high-dose aprotinin were used.Two patients required transfusion, one with permission from the family, and the other (6-year-old child) against the family's wishes.There is also a published series of 4 patients in Brazil[30]and 2 in Australia[31].
Living related liver transplantation has also been performed where donor and recipient were both JW.In one such case, splenic embolisation, RhEpo, iron, cell salvage and aprotinin were used[32].In another case, the recipient hepatectomy was performed in two stages due to a hypertrophied, enlarged left lobe of the liver, which was excised 2 wk after receiving the liver transplant[33].Jabbouret al[34]also published a series of eight successful liver transplants in JW patients, all with RhEpo, cell salvage and acute normovolaemic haemodilution.
Splenic embolisation may also be utilised to control hypersplenism and portal blood flow in an effort to improve thrombocytopaenia and minimise operative blood loss[35].Some centres have also reported that strategies to avoid blood transfusions in JW patients has had a positive impact by reducing overall blood use in non-JW patients undergoing liver transplantation as well[36].
Pancreas transplantation
Decisions to proceed to pancreas transplantation may be more complex than liver transplantation as the original condition will often be less imminently life threatening,therefore the surgical risks involved may not be outweighed by the benefit.There is also the option of islet transplantation, which may be performed by open rather than percutaneous approach to minimise the risk of bleeding.
There are two series published in the literature.Boggiet al[37]performed six simultaneous pancreas and kidney transplants.All patients recovered, however, one was readmitted with unexplained anaemia and became haemodynamically unstable.This patient received a blood transfusion.A second series of five patients is also published with successful outcomes[38].Both centres used pre-operative RhEpo, iron and B12 as well as cell salvage.
Kidney transplantation
Surgical blood loss tends to be less problematic in kidney transplantation compared with liver and pancreas, as such the operative risks to JW patients are likely to be less.Published experience in renal transplantation in JW patients dates back to the 1980s.Kaufmanet al[39]published an early series demonstrating comparable outcomes in JW patients, although there were two deaths due to a combination of severe anaemia and early rejection episodes.More recently, a case of successful human leukocyte antigenincompatible living donor kidney transplantation has been reported[40], where cryoprecipitate was required due to fibrinogen depletion following four sessions of pre-operative plasma exchange.
CONCLUSION
The global experience in abdominal solid organ transplantation in JW patients remains fairly limited, although some case series have been published for each organ.It is clear that such patients require the surgical team to dedicate more time to ensure their safe management.This begins with a thorough, detailed consent of exactly which products and interventions they will or will not accept.Based on this, planning must begin weeks before surgery if possible.Their cardiopulmonary fitness must be assessed in context of being able to withstand severe anaemia.Preconditioning the patient with RhEpo, iron, B12 and folic acid optimises their condition for the time of surgery.Interventions such as acute normovolaemic haemodilution and cell salvage should be utilised to minimise the effective surgical blood loss.Each case must be assessed individually, but provided they meet fitness requirements, there are no absolute contraindications to abdominal organ transplantation.
