举宫杯在腹腔镜下剖宫产瘢痕妊娠病灶清除术中的临床应用
杨树环 王志毅 蔡钰
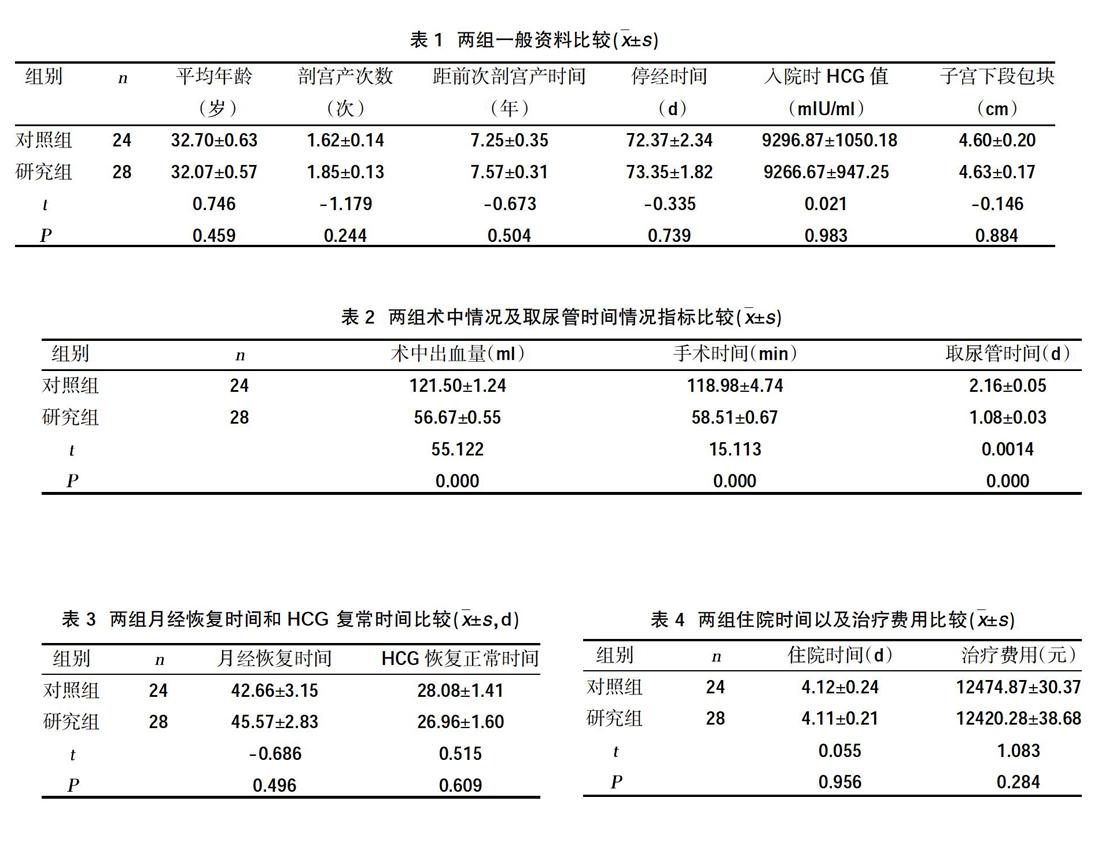
摘要:目的 探讨举宫杯在经腹腔镜下剖宫产瘢痕妊娠病灶清除术中的临床应用价值。方法 回顾性分析2016年1月~2018年6月在我院住院治疗的52例剖宫产瘢痕妊娠患者相关资料。根据治疗方式不同分组,将经安置举宫杯后行腹腔镜下剖宫产瘢痕妊娠病灶清除术的28例设为研究组,将未安置举宫杯直接行腹腔镜下剖宫产瘢痕妊娠病灶清除术的24例设为对照组。比较两组术中出血量、手术时间、术后月经恢复时间、HCG恢复正常时间、取尿管时间、术后疼痛、持续性切口妊娠发生、住院时间及费用。结果 研究组术中出血量(56.67±0.55)ml、手术时间(58.51±0.67)ml,取尿管时间(1.08±0.03)d均少于对照组的(121.50±1.24)ml、(118.98±4.74)ml、(2.16±0.05)d,具有统计学意义(P<0.05)。两组术后月经恢为复时间、HCG复常时间、术后疼痛、住院时间、住院费用、术后疼痛、术后持续性切口妊娠发生情况比较,差异无统计学意义(P>0.05)。结论 举宫杯在腹腔镜下剖宫产瘢痕妊娠病灶清除术中具有减少出血量、缩短手术时间等优点,对降低手术难度具有重要意义。
关键词:举宫杯;腹腔镜;剖宫产瘢痕妊娠
Abstract:Objective To investigate the clinical application value of the lifting cup in the laparoscopic cesarean scar pregnancy.Methods A retrospective analysis of 52 patients with cesarean scar pregnancy who were hospitalized in our hospital from January 2016 to June 2018 was retrospectively analyzed. According to different treatment groups, 28 cases of laparoscopic cesarean section scar pregnancy removal after placement of the uterus cup were set as the study group, and the laparoscopic cesarean scar pregnancy lesions were directly placed without the uterus cup. 24 cases of debridement were set as the control group. The intraoperative blood loss, operation time, postoperative menstrual recovery time, HCG recovery time, urinary catheter time, postoperative pain, persistent incision pregnancy, hospitalization time and cost were compared between the two groups.Results In the study group, intraoperative blood loss (56.67±0.55) ml, operation time (58.51±0.67) ml, and urinary catheter time (1.08±0.03) d were less than the control group (121.50±1.24) ml, (118.98±4.74). ) ml, (2.16 ± 0.05) d, with statistically significant (P<0.05). There were no significant differences in postoperative menstrual recovery time, HCG recurrence time, postoperative pain, hospitalization time, hospitalization cost, postoperative pain, and postoperative persistent incision pregnancy between the two groups (P>0.05).Conclusion The uterine cup has the advantages of reducing the amount of bleeding and shortening the operation time during laparoscopic cesarean scar pregnancy removal, which is of great significance for reducing the difficulty of surgery.
Key words:Uterine cup;Laparoscopy;Cesarean scar pregnancy
剖宮产瘢痕妊娠(caesarean scar pregnancy,CSP)是妊娠囊种植在剖宫产手术疤痕处的子宫肌层,是一种非常少见的异位妊娠。随着剖宫产率的不断升高,CSP的发生率亦有增高趋势[1]。子宫疤痕妊娠是剖宫产远期并发症,并且可能出现非常严重的并发症,甚至危及生命[2]。若孕囊向宫腔生长,常形成妊娠中晚期的凶险性前置胎盘;若向子宫肌层和浆膜层生长,可早期出现子宫切口瘢痕处破裂或大出血,严重者甚至需要切除子宫来挽救患者生命。目前,对于CSP尚无统一的治疗标准,主要还是根据瘢痕妊娠分型选择不同治疗方案,分型依靠阴道彩超及MRI评估[3-5],不同分型指导选择不同治疗方案[6]。但对Ⅱ、Ⅲ型子宫切口瘢痕妊娠选择手术治疗。随着医疗技术水平不断发展,微创技术的进步,目前已经从经阴道子宫疤痕妊娠病灶清除术发展到腹腔镜下子宫切口妊娠物清除术。对比前者手术方式,后者更具有直观、解剖更清晰、同时可修补子宫憩室等优点,临床应用也逐渐广泛。但如何更好地分离膀胱与子宫下段粘连,尤其是多次剖宫产患者,减少术中出血、减少副损伤等问题仍值得探究。本研究旨在探讨举宫杯在经腹腔镜剖宫产瘢痕妊娠病灶清除术中的效果,并与未安置举宫杯行腹腔镜下CSP病灶清除术进行比较,明确安置举宫杯是否在手术中具有优势,现报道如下。
本研究中的52例患者中,28例患者查见子宫切口孕囊,其中22例可见胚芽及心管搏动;余24例可见子宫下段切口处非均质回声团。52例患者子宫切口子宫肌层厚度为1~3 mm。子宫下段肌层薄,分离膀胱腹膜反折容易出血,且患者多有1次以上剖宫产史,粘连重,容易出现膀胱、输尿管损伤。寻找更合适的办法减少术中出血及副损伤是确保手术疗效的关键。本研究中研究组在术中出血量、手术时间,取尿管时间均少于对照组,具有统计学意义(P<0.05)。提示腹腔镜下子宫切口妊娠物清除术中安置杯状举宫器后膀胱容易自宫颈及阴道前穹隆分离,更容易找到膀胱宫颈间隙,下推膀胱更容易,减少术中出血量、缩短手术时间、缩短安置尿管时间。与研究报道一致[19]。
選择腹腔镜下子宫切口病灶清除不仅清除妊娠组织,还能切除疤痕组织,修补子宫切口缺陷,从而增加治疗的有效性,降低再次切口妊娠风险,同时降低再次子宫切口憩室发生率。举宫杯的使用在腹腔镜下子宫切口妊娠物清除术中明显降低手术难度,减少手术并发症。因此,在腹腔镜下子宫疤痕妊娠病灶清除术中安置举宫杯操作方便,具有较高的安全性和有效性,值得临床借鉴应用。
参考文献:
[1]李露,张轶清.子宫疤痕处妊娠研究进展[J].承德医学院学报,2016,33(3):246-249.
[2]Horne AW,Skubisz MM,Johns TG,et al.Combination gefitinib and methotrexate treatment for non-tubal ectopic pregnancies:a case series[J].Hum Reprod,2014,29(7):1375-1379.
[3]傅柳陶,金东,卫兵,等.阴道超声联合MRI对剖宫产后子宫切口瘢痕处妊娠的诊断价值[J].安徽医学,2018,39(8):907-909.
[4]韦昕芳,赵华山,姜陵,等.剖宫产切口妊娠患者MRI影像特点及临床结局分析[J].中国CT和MRI杂志,2018,16(5):110-113.
[5]瞿薇花,唐震.子宫切口瘢痕妊娠的MRI诊断[J].医学影像学杂志,2016(1):175-177.
[6]吴莎,于小娜,王秋玉.不同分型CSP的手术结果分析[J].中国计划生育学杂志,2018,26(12):1254-1256.
[7]Godin PA,Bassil S,Donnez J.An ectopic pregnancy developing in a previous caearean section scar[J].Fertil Steril,1997,67(2):398-400.
[8]章鹏鹏,孔丽娜.子宫疤痕处妊娠诊断和治疗的最新进展[J].湖北科技学院学报(医学版),2015,29(3):272-275.
[9]陈雪,李艳飞,黄岳.宫腔镜手术治疗早期内生型剖宫产术后子宫疤痕妊娠的疗效观察[J].山西医药杂志,2016,45(8):871-875.
[10]王玮.腹腔镜手术和开腹手术对异位妊娠治疗效果的对比分析[J].陕西医学杂志, 2016,45(4):423-424.
[11]吴一彤.子宫动脉栓塞MTX介入及清宫术联合用于疤痕妊娠的疗效及可行性[J].临床和实验医学杂志,2015,14(19):1638-1641.
[12]周传亚,史爱丽,张小玲,等.经阴道切除CSP26例[J].中华灾害救援医学,2016,4(2):113-114.
[13]Le A,Shan L,Xiao T,et al.Transvaginal surgicaltreatment of cesarean scar ectopic pregnancy[J].Arch Gynecol Obstet,2013,287(4):791-796.
[14]Fystra DL,Pound Z,Chang T,et al.Ectopic Pregnancy within a cesareean delivery scar:A case report[J].Am J Obsstct Gynecol,2002,187(2):3022-3041.
[15]Fong J,Gurewitsch ED,Kang HJ,et al.An analysis of transfusion prectics and the role of intraoperative red blood cell salvage during cesarean delivery[J].Anesth Analg,2007,1049(3):666.
[16]庄粤冰.经阴道病灶切除术治疗32例子宫瘢痕妊娠的临床分析[J].现代妇产科进展,2016,25(4):296-297.
[17]尹香花,顾建娟,成艳.杯状举宫器联合超声刀在腹腔镜全子宫切除术中的应用价值[J].中国微创外科杂志,2010,10(12):1086-1087.
[18]蒋燕,赵卫东,周虎.腹腔镜联合杯状举宫器下全子宫切除术的学习曲线[J].安徽医学,2014,35(8):1023-1026.
[19]庄元,罗燕,李福敏.腹腔镜与阴式手术治疗外生型CSP的对比研究[J].中国妇幼保健,2018,33(14):3314-3317.
收稿日期:2019-5-5;修回日期:2019-7-2
编辑/肖婷婷

