Type 1 diabetes in a Nigerian family - occurrence in three out of four siblings:A case report
Michael Adeyemi Olamoyegun,Oluwabukola Ayodele Ala
Michael Adeyemi Olamoyegun,Department of Internal Medicine,Endocrinology,Diabetes &Metabolism Unit,College of Health Sciences,Ladoke Akintola University of Technology(LAUTECH)/LAUTECH Teaching Hospital,Ogbomoso 240222,Oyo State,Nigeria
Oluwabukola Ayodele Ala,Department of Internal Medicine,Endocrinology,Diabetes &Metabolism Unit,BOWEN University Teaching Hospital,and College of Health Sciences,BOWEN University,Iwo 232101,Osun State,Nigeria
Abstract
Key words: Type 1 diabetes; Siblings; Case report; Nigerian; Family
INTRODUCTION
Type 1 diabetes (T1D) is a life-long medical condition that primarily affects young people.It is characterized by immune destruction of insulin-producing beta-cells in the pancreas resulting from the action of environmental factors in genetically predisposed individuals[1].It usually begins in childhood or young adulthood but can develop at any age.The presence of any of the following antibodies increases the risk of T1D:Glutamic acid decarboxylase-65,islet cell,insulin autoantibody and insulinoma-associated protein-2[2].In general,70% of people with new-onset T1D have a positive antibody if only one antibody is measured,whereas 90% will have at least one antibody when all forms are measured[2].Most occurrences of T1D cases in any population are sporadic; that is,first-degree relatives do not have diabetes at the time patient with diabetes is diagnosed.Nevertheless,siblings of childhood-onset T1D patients are at increased risk of developing the same disease compared with the general population[3,4].
Genetic susceptibility is important in the development of T1D.In Caucasian populations,the lifetime risk in siblings of type 1 diabetic probands has been reported to be much higher than that in the general population (6%vs0.4%),indicating that T1D clusters in families[5].This represent a 15-fold risk tendency in siblings compared to the risk in the general population[5].This classic role of genetics in diabetes risk is demonstrated by comparing concordance rates in monozygoticversusdizygotic twins.In Finland,with the highest incidence of T1D,concordance rates for T1D were found to be 27% and 3.8% among monozygotic and dizygotic twins,respectively[6].Familial clustering (which refers to the occurrence of a disorder at a higher frequency in firstdegree relatives of an affected person compared to the general population)[7]of T1D is a rare occurrence.Even more rare is for three or more siblings to develop T1D.
It is estimated that HLA (a cluster of genes located within the major histocompatibility complex) on chromosome 6p21 accounts for 40%-50% of familial clustering and the strongest genetic association with T1D[8],in addition to other different genetic loci that contribute susceptibility to the development of T1D[9].Although the risk of developing T1D is increased in relatives of individuals with the disease,the risk is relatively low.This risk depends on which HLA haplotypes are shared[8].From multiple family pedigrees and HLA typing data,it is estimated that if a sibling shares both HLA-D haplotypes with an index patient,the risk for that individual is 12% to 20%.For a sibling sharing only one haplotype,the risk for T1D is 5% to 7%.For a sibling with no haplotype in common,the risk is only 1% to 2%[10].According to Redondoet al[11],approximately 85% of new cases of T1D occur in persons without an affected first-degree relative.Approximately 13% of children and adolescents who develop T1D have a parent or sibling with diabetes.Dahiquist and Gothefors[12]reported that among children with newly diagnosed diabetes,2%-3% had a mother with T1D,5%-6% had a father with T1D and 4%-5% had a brother or a sister with T1D.
The study of familial clustering is an important concept in genetic epidemiology.The lifetime risk in siblings of type 1 diabetic probands in Nigerians is unknown (it has never been reported).Hence,the purpose of this paper is to report a case of a Nigerian family in which T1D occurred in three siblings among four children with neither of the parents having diabetes.This report will encourage clinicians to assess the possibilities of diabetes in siblings of children with T1D.
CASE PRESENTATION
Chief complaints
The three siblings presented with polyuria,polydipsia and weight loss of about 2 wk duration.
Present illness
Case 1:First child,male,was diagnosed of acute-onset T1D at 15-years-old.He had presented with osmotic symptoms (polyuria and polyuria) and associated weight loss about 2 weeks before presentation.At presentation,he was drowsy and dehydrated.
购物车里的宝贝,是韩莎挑了很多天才选出来的,眼睛都快累盲了,而杜飞就因为凑不够满减的优惠,竟然不让她买了!
Case 2:Second child,female,was diagnosed of acute-onset T1D at 11-years-old.She had presented with polyuria,polydipsia and weight loss.
Case 3:Fourth child,male,was delivered at estimated gestation age of 36 wk and birth weight was 4.65 kg.He presented with features of acute-onset osmotic symptoms at 9-years-old (Figure 1).
History of past illness
None of the siblings were previously diagnosed with diabetes.
Personal and family history
Both parents of the probands have no prior history of diabetes.Their blood glucose and glycated hemoglobin (HbA1C) levels were within normal ranges.The third child(male) had no history suggestive of diabetes,and his blood glucose and HbA1C were within normal ranges.None of the siblings or parents were smokers or used alcohol.The father was overweight,and the mother was diagnosed with obesity.
Physical examination upon admission
Case 1:At presentation,he was drowsy and dehydrated.His plasma glucose and HbA1C levels were 403 mg/dL (22.4 mmol/L) and 10.6%,respectively.His urinalysis showed glucosuria (4+) and ketonuria (3+).His serum C-peptide level was markedly low,which showed that his insulin secretory capacity was reduced.
Case 2:Her blood glucose at diagnosis was 448 mg/dL (24.9 mmol/L),and HbA1C was 11.0%.Urinalysis showed ketonuria (3+) and glucose (4+) but no proteinuria.
Case 3:His blood glucose at diagnosis was 448 mg/dL (24.9 mmol/L) and HbA1C was 11.0%.Urinalysis showed ketonuria (3+) and glucose (4+) but no proteinuria.
Anti-glutamic acid decarboxylase,anti-insulinoma-associated protein-2 and antithyroid peroxidase antibodies were determined by radioimmunoassay.However,the genotype of the HLA could not be done due to lack of facility (Table 1).
FINAL DIAGNOSIS
All were diagnosed of acute-onset diabetic ketoacidosis and T1D.
TREATMENT
All were treated with intravenous fluid and multiple doses of insulin at admission.
OUTCOME AND FOLLOW-UP
All are currently being treated with multiple injections of insulin with total daily insulin dosage ranges of 90-122 U/d.They all have fair glycemic control with occasional hypoglycemia in the youngest sibling with diabetes.
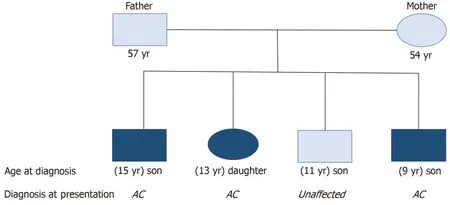
Figure1 Pedigree of the family with type 1 diabetes.
DISCUSSION
The occurrence of T1D among three or more siblings is extremely rare.Although large families with T1D arising from a common ancestor have been reported among Arabs[13]and in the Netherlands[14].However,none have been reported among Nigerians except a patient with T1D whose three siblings also had prediabetes[15].An analysis of 767 multiplex Caucasian families showed that fifty-one families had three affected siblings,one family had four affected siblings and two families had five affected siblings[16].There has also been a reported case of T1D in three sisters in a Japanese family,whose parents also had T1D[17].To our knowledge,no case report has described T1D in three or more siblings in Nigerian patients.
In this case report,three out of four siblings (two males and one female) developed T1D,although neither of the parents had diabetes.Fathers have been known to transmit T1D to their offspring more than mothers[17,18].At diagnosis,4%-7% of children have a father with T1D whereas 1.5%-3% have an affected mother.This tendency of transmitting the disease is amplified if both parents have the disease.This familial T1D has been shown to be associated with increased genetic susceptibility attributed to a higher prevalence of HLA genes among family members[8,19].Hence,the T1D risk for siblings depends on genetic background primarily in the HLA region on chromosome 6 in particular[8],and it depends on siblings sharing the HLA haplotype with the proband[18].While HLA-B8 is strongly associated with T1D in Caucasians,the contrary was the case among Nigerians[20].Another study[21]reported a low prevalence of HLA-DR4 among Nigerians with T1D.The incidence and prevalence of T1D is not known in Nigeria although the prevalence was said to be much lower than and occurred at later ages compared to Caucasians[22].This rare occurrence makes it difficult to identify families with multiple siblings with T1D.
Regarding the age of diagnoses of our patients,there was a progressive decline in the age of diagnosis and reduced levels of glycemia at diagnosis as assessed by both plasma glucose and HbA1C with subsequent siblings with diabetes.The decreasing age of diagnosis of other siblings compared to the first affected sibling is in keeping with previous reports demonstrating a younger age at diagnosis among affected siblings[23-25].The progressive reduction in the age of diagnosis might be due to modification of the genetic susceptibility by environmental factors such as diets,abnormal weight gain or sedentary lifestyles.Previous studies showed that HLA genes related to high disease susceptibility (HLA-DR and HLA-DG genotypes) were associated with earlier onset of diabetes[26,27].Also,Harjutsaloet al[16]suggested that genetic effects in such families may be particularly strong.They proposed that a young age at onset in the first child diagnosed with T1D indicated an overall increased lifetime risk for T1D in siblings and that the process leading to diabetes seems more rapid in such siblings.Long-term follow-up studies corroborated this statement[28,29].Another explanation that has been proposed is that genetic or environmental factors that precipitate an earlier onset of T1D in the proband are shared with the other siblings and may also increase their risk for T1D.
The mode of presentation at diagnosis in all these three siblings was quite similar.All of them presented with polyuria,polydipsia and weight loss over a similar mean period of time with consequent diagnosis of diabetic ketoacidosis.Although,there was a slight increase in blood sugar of the second sibling compared to the first,there was a reduction in the plasma glucose at presentation in the third sibling who had the lowest blood sugar among the three affected siblings.The first affected siblingpresented with the worst clinical symptoms at presentation as he was drowsy.This observation was probably due to greater family awareness of diabetic symptoms,hence earlier presentation to the hospital of the younger siblings.
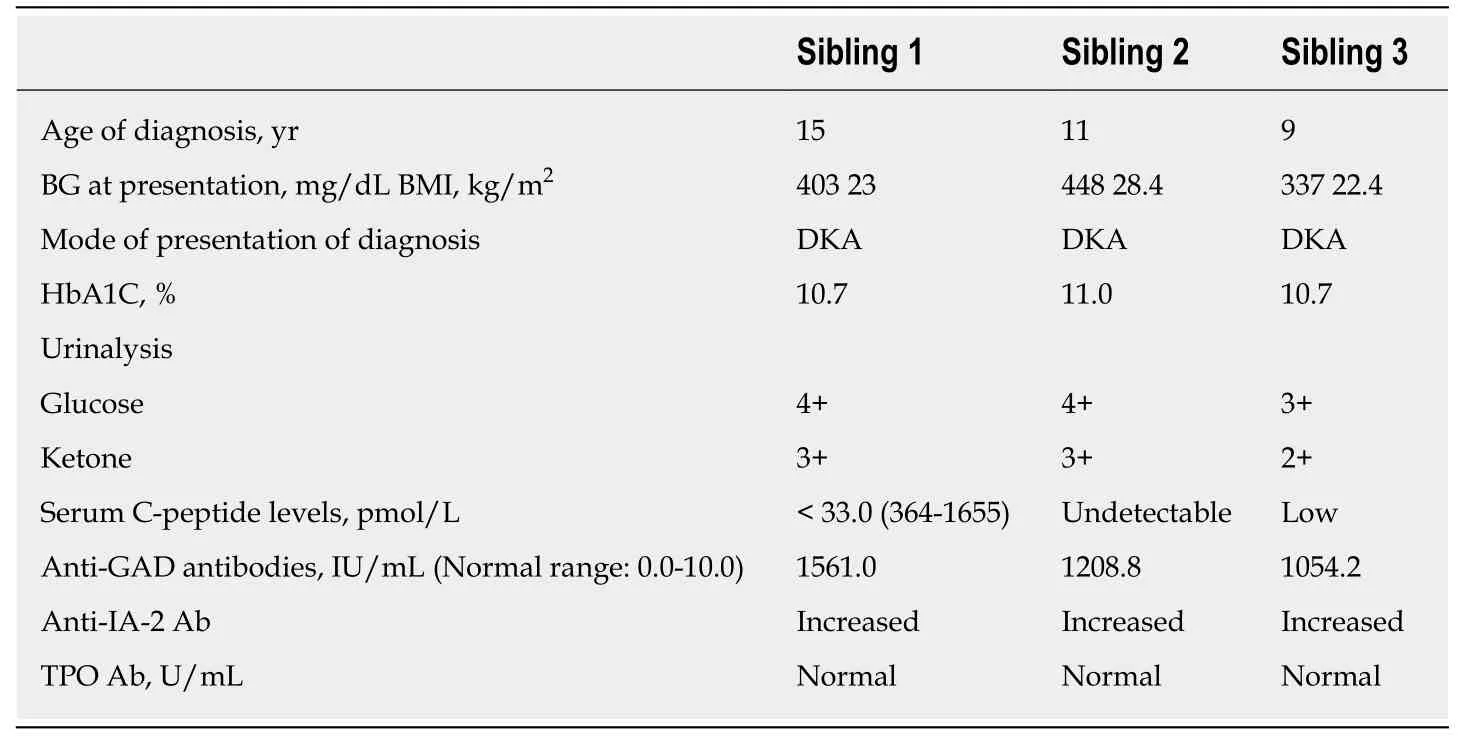
Table1 Laboratory parameters of the siblings at diagnosis
Although this report showed the possibility of familial clustering of T1D among siblings,our inability to do genetic analysis for proper characterization of the exact loci genes affected was a limitation of this study.Although,one sibling of the four children was not affected by T1D,we could not assess him for the presence of autoantibodies,which may also predispose him to development of diabetes in the future.
CONCLUSION
This is the first report of familial clustering of T1D in three out of four children in a Nigerian family.This shows that the occurrence of T1D among siblings is possible even in areas where the incidence and prevalence of T1D is rare (as in Nigeria).This report is also unique because neither of the parents had either type 1 or type 2 diabetes.The finding of decreasing age at diagnosis and severity of symptoms at presentation with each subsequent sibling suggested a possible influence of environmental effects on genetic susceptibility and awareness of diabetes symptoms from prior diagnosis.
 World Journal of Diabetes2019年10期
World Journal of Diabetes2019年10期
- World Journal of Diabetes的其它文章
- Diabetic cardiomyopathy:Pathophysiology,theories and evidence to date
