Exercise as a prescription for patients with various diseases
Xin Lun,Xingyng Tin,Hixin Zhng,Rui Hung,N Li,Peijie Chen,*,Ru Wng,*
a School of Kinesiology,Shanghai University of Sport,Shanghai 200438,China
b Department of Sport,Huainan Normal University,Huainan 232038,China
Abstract A growing understanding of the benefits of exercise over the past few decades has prompted researchers to take an interest in the possibilities of exercise therapy.Because each sport has its own set of characteristics and physiological complications that tend to occur during exercise training,the effects and underlying mechanisms of exercise remain unclear.Thus,the first step in probing the effects of exercise on different diseases is the selection of an optimal exercise protocol.This review summarizes the latest exercise prescription treatments for 26 different diseases:musculoskeletal system diseases (low back pain, tendon injury, osteoporosis, osteoarthritis, and hip fracture), metabolic system diseases (obesity,type 2 diabetes,type 1 diabetes,and nonalcoholic fatty liver disease),cardio-cerebral vascular system diseases(coronary artery disease,stroke,and chronic heart failure),nervous system diseases(Parkinson's disease,Huntington's disease,Alzheimer's disease,depression,and anxiety disorders),respiratory system diseases(chronic obstructive pulmonary disease,interstitial lung disease,and after lung transplantation),urinary system diseases (chronic kidney disease and after kidney transplantation), and cancers (breast cancer, colon cancer, prostate cancer, and lung cancer).Each exercise prescription is displayed in a corresponding table.The recommended type,intensity,and frequency of exercise prescriptions are summarized,and the effects of exercise therapy on the prevention and rehabilitation of different diseases are discussed.2095-2546/© 2019 Published by Elsevier B.V.on behalf of Shanghai University of Sport.This is an open access article under the CC BY-NC-ND license.(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Keywords: Diseases;Exercise prescription;Patients
1. Introduction
Various diseases occurring in the human body are not only detrimental to people's health, but can also reduce quality of life. The lack of physical activity (PA) in modern life is a main reason for the decline of national physical fitness. It affects the growth and development of children and adolescents, as well as the physical wellness and work efficiency of adults.At the same time,a lack of exercise leads to an increase in the incidence of chronic diseases, which increases medical costs and the economic burden on the state and individuals.Guiding people to take part in exercise properly to enhance physical fitness is more urgent and more important than ever.
Lifestyle interventions should be the primary strategy for the prevention and treatment of metabolic diseases owing to their safety and effectiveness.Reasonable diet and weight control have received widespread attention, but the role of an exercise intervention is often overlooked by doctors and patients.1Research shows that a reasonable exercise intervention can increase energy consumption, strengthen muscle,reduce blood pressure and blood lipids,increase bone density,and regulate psychological processes.2-4Therefore, the importance of establishing an individual's level of PA,like the dosage of a drug, prompts investigators to study this problem in different diseases and in different clinical areas related to undesirable living habits. To achieve the desired goal, a specific exercise prescription is important.5
Exercise prescription is generally a specific plan of PA designed for a specific purpose, and it is usually developed by rehabilitation specialists based on the patient's condition.It mainly includes the type, frequency, intensity, and duration of exercise. For resistance exercise (RE) prescription, the total amount of training, interval time, and so on also need to be determined.6Exercise intensity is critical for patients, and is usually determined by subjects' heart rate reserve, maximum heart rate (HRmax), maximum oxygen uptake (VO2max),or rating of perceived exertion scales. The overall condition of each patient and the characteristics of the disease should also be considered. Generally, in the early and middle stages of the disease, moderate-intensity or even high-intensity intervals can be adopted. If the disease is in its late stages or if it is shortly after surgery, low-intensity training should be carried out, and the load intensity should be increased gradually. Owing to the special and unique needs of individual patients, the exercise prescription should be personalized and its goal should be evaluated during implementation to achieve the desired effect.
The purpose of this review was to provide effective exercise prescriptions for different diseases as identified in randomized controlled trials(RCTs).After providing background on 26 different diseases in 7 categories, we collated and analyzed the different types of exercise prescriptions and their effects for each disease. We conclude by identifying the best exercise therapy program and its dosage based on evidence,experience, and common sense. The review provides a scientific and methodological basis for choosing an exercise prescription based on to the type of disease being treated and the health needs of the patient, which can aid in preventing and treating diseases and thus promote rehabilitation and improvement in the quality of patients'lives.
2. Methods
2.1. Data collection
The process used for screening articles is summarized in Fig. 1. A comprehensive literature search was carried out for all forms of exercise in the PubMed of NCBI databases using the following search terms: (exercise [Title] OR training[Title]) AND (human [Title]). To limit the range of search results, we set 2 filters: publication dates within the past 10 years and sorting by best match. We initially found 736 articles corresponding with these limitations. Next, we excluded review articles and gave priority to articles reporting on RCTs with exercise intervention as the main research method, with consideration given to the frequency of the occurrence of the disease and the relative need for exercise therapy.In addition,we focused on the effect of a single exercise intervention and excluded treatments related to diet,drugs, and other measures. Using these filters, we identified 188 articles and used them for data analysis.
2.2. Data analysis
According to the various targets of exercise intervention,we classified the selected articles into 7 categories: musculoskeletal system diseases, metabolic system diseases, cardiocerebral vascular system diseases, nervous system diseases,respiratory system diseases, urinary system diseases,and cancers. The selected articles were further subdivided into different disease types associated with each category. The details regarding the exercise protocols that were documented in the articles are listed in the following sections according to the exercise protocol's duration,frequency,and intensity level.
After classifying and analyzing the articles, we identified some commonly used protocols for exercise rehabilitation prescribed for different human diseases.These protocols included aerobic exercise(AE),RE,combined AE with resistance training (CT), home-based exercise (HE), multimodal exercise(ME), and other exercises. The general standards and procedures used for these types of training are described.
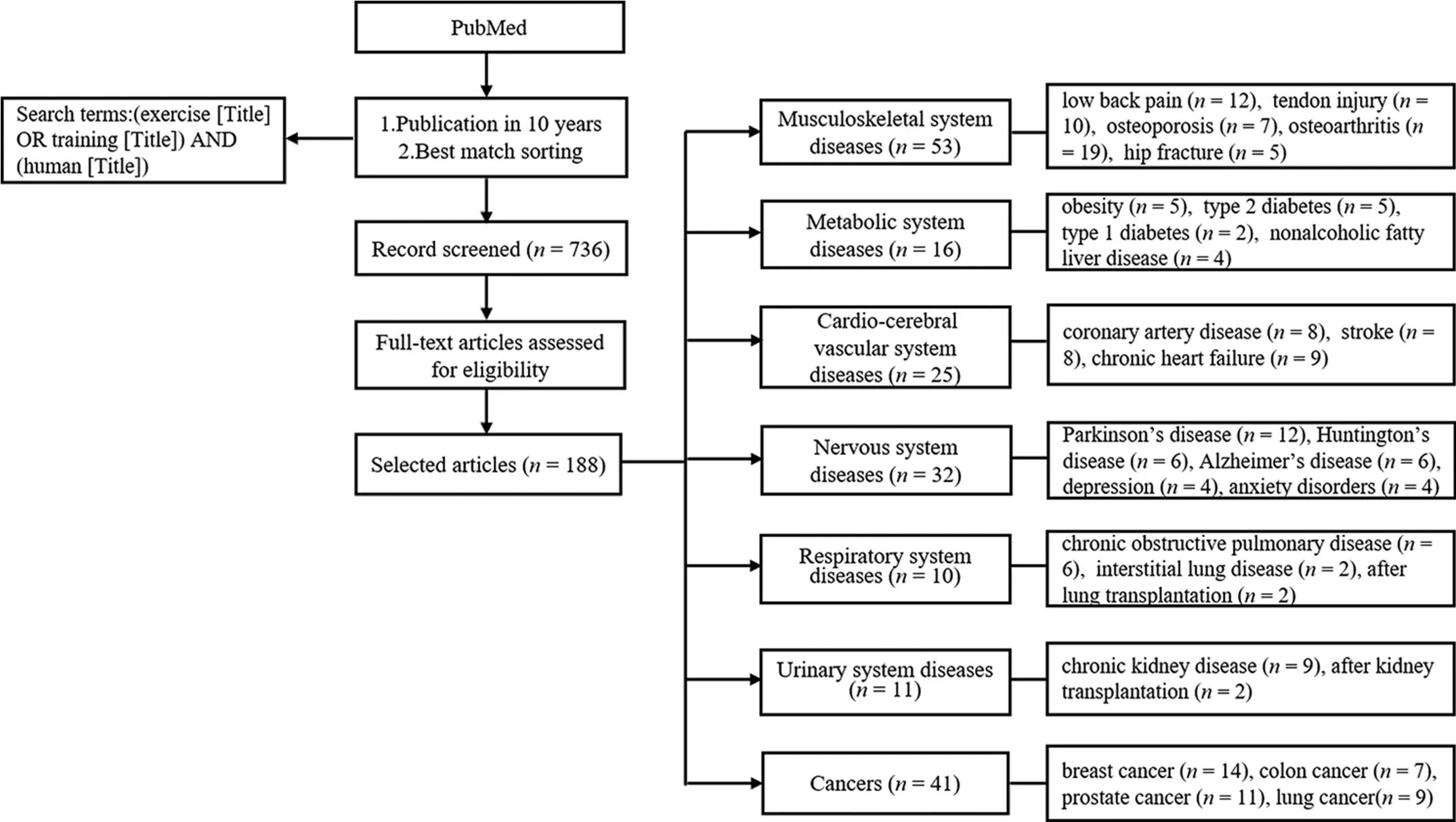
Fig.1. The flowchart for article searches.The articles included in this review were published before July 2018.
2.3. Classification of exercise types
2.3.1. AE
AE (i.e., regular exercise characterized by high repetition and low resistance demands during skeletal muscular contraction)7is a well-established approach to improving aerobic capacity and health.AE plays a homeostatic role in regulating the rate of energy production,blood flow,and substrate utilization in response to locomotion.8
Typical forms of AE include walking and running on a treadmill, yoga, Tai Chi, Pilates, and cycling. When used for early postoperative rehabilitation or severe disease, each AE regimen can be categorized as being of low,moderate,or high intensity. Endurance training can also be classified as highintensity AE. Patients who have acceptable cardiorespiratory function are commonly treated, especially at the restorative stage, by cycle, treadmill, or stationary bicycle ergometer using high-intensity interval training (HIIT). In comparison with other types of exercise,HIIT can be considered as a more effective and time-efficient intervention to improve blood pressure and aerobic capacity in obese youths.9
We defined 6 weeks as a tipping point between short-term and long-term exercise; short-term exercise lasts for fewer than 6 weeks while long-term exercise lasts for 6 weeks or more.In the studies we reviewed,the frequency of training ranged from 2 to 6 times per week. Intensity was usually expressed as a percentage of heart rate reserve,a percentage of HRmax,VO2max,or the rating of perceived exertion scales.We followed the intensity classification specified in the original tables from the References articles and, if there was no mention of intensity there, we referred to the classification standard identified in Table 1.10
2.3.2. RE
RE originated in Europe in the 19th century and was quickly adopted in the United States.11At first, it was believed that RE was detrimental to health and athletic performance. However,with an increased understanding of exercise, RE came to be viewed as helpful to athletes in improving their performance.12RE is now part of the recommended activities for helping adults maintain their overall health and has been shown to decrease mortality, cardiovascular disease, cholesterol levels, depression,and fatigue,and to improve bone density and insulin sensitivity.13
RE includes strength training and self-managed loaded exercise.Resistance can be achieved by using resistance bands,body weight, or weights such as dumbbells, barbells, machines, and kettle bells. When weights are used, the amount of lift is often defined with respect to a repetition maximum.In this review,RE refers mostly to progressive resistance training(PRT)with weight machines or when different machine-based protocols are used to train major upper and lower muscle groups.
RE protocols involve many factors,including the frequency and intensity of training. Frequency refers to the number of times a muscle group is exercised each week. A repetition refers to 1 full movement of an exercise, and the number of times that movement is done without stopping is the number of repetitions per set. A set refers to the number of times an individual repeats an exercise with a given number of repetitions.14Intensity is affected by a combination of (1) the amount of resistance used, (2) the number of repetitions, and(3) the number of sets of repetitions performed per muscle group.The intensity of RE varies based on the patient's condition. We followed the intensity classification specified in the original tables from the Referencesarticles and,if there was no mention of intensity,we referred to the classification standard identified in Table 1.The training duration for RE is the same as for AE:short term(<6 weeks)and long term(≥6 weeks).
2.3.3. CT
CT greatly benefits body function.Current theoretical studies show that combining AE with resistance training not only enhances cardiorespiratory function,15but also increases muscle strength.16Owing to CT including RE, full consideration should be given to the patient's endurance capabilities before CT is prescribed. Depending on the condition of the patient,the most common regimens for CT are walking and riding a bicycle. When the duration of CT is shorter than 6 weeks, we classify it as short-term CT; otherwise it is classified as longterm CT.Intensity of CT is classified in the same way as intensity of AE.
2.3.4. HE
HE (an exercise program that can be undertaken individually in the patient's own home) has been introduced in an attempt to enhance long-term adherence to recommended levels of PA.17As a type of exercise that is simple and easy, HE is integrated into the daily lives of patients.HE can lead to significant improvements in PA levels, balance, mobility, andmuscle strength. Some HE only involves an AE intervention.However, HE patients often first undertake a simple AE regimen,and then do some strength training and other RE.Sometimes HE patients are prescribed specific training, such as high-intensity leg-strengthening exercises or functionally oriented exercises. The duration of HE is classified in the same way that duration of AE is classified.Intensity of HE is classified in the same way as intensity of AE.

Table 1 Classification of exercise intensity.
2.3.5. ME
ME is a combination of various training methods.Almost all ME trials include AE,RE,strength training,stretching training,balance exercise,and other forms of exercise.ME interventions usually start with AE and use stationary bicycle/cycle ergometers and walking.This is followed by strengthening exercises for the upper limbs and ends with a set of cool-down stretching exercises.Training intensity for ME varies considerably among studies,ranging from 50%to 90%of the HRmax.18ME is effective in improving muscle strength in the lower extremities,dynamic standing balance,gait speed,and chair stand test scoring.In addition,ME is effective in reducing falls.It is most often prescribed for postoperative treatment and rehabilitation of patients with nervous system diseases. It can also improve cancer-related fatigue symptoms.19The duration of ME is classified in the same way that duration is classified for AE.The intensity of ME is classified in the same way as the intensity of AE.
2.3.6. Other exercises
There are other special exercise prescriptions, such as balance exercise, aquatic or water-based exercise (distinguished from swimming),whole body vibration(WBV)exercise,concentric and eccentric exercise, and stretching training. The supplementary tables in various sections of this review identify some of the diseases for which these forms of exercise were used in some of the studies we reviewed.
3. Results
3.1. Musculoskeletal system diseases
The musculoskeletal system includes bones, skeletal muscles,tendons, ligaments, cartilage, joints, and other connective tissues,along with vascular and nervous tissues.20Bones and skeletal muscles are the 2 largest tissues within this system and play fundamental roles in human physiology,enabling locomotion and movement,promoting blood flow to organs,and providing protection for vital organs.20,21Sports is a way for people to engage in PA;however, injuries can be a negative consequence of engaging in sports.22Sports injuries occur during athletic activities or as a result of exercising. Common sports injuries include acute and chronic injuries of muscles, tendons, and ligaments, as well as traumatic fractures and other injuries. The prevention and rehabilitation of sports injuries are addressed through the use of different kinds of training and exercise,or a combination of the 2 modalities.23
3.1.1. Low back pain(LBP)
LBP is one of the main causes of disability and is a major public health issue in many developed countries.24Chronic nonspecific LBP is usually defined as pain,muscle tension,or stiffness that is localized below the costal margin and above the inferior gluteal folds.25The vast majority of patients(up to 90%) described having nonspecific LBP, which is defined as symptoms without a clear specific cause.25
Supplementary Table 1 shows that the forms of exercise most commonly used to treat LBP in the studies we reviewed were AE and WBV exercise. At present, exercise therapy is one of the key treatments for the rehabilitation of chronic nonspecific LBP. The modes of AE most commonly used were Tai Chi,yoga,and Pilates.Long-term,low-intensity AE was a safe and effective intervention for patients with nonspecific LBP.AE not only alleviated pain,26anxiety,and depression,27but also improved body function more effectively. For example,AE improved patients' flexibility,balance,28,29and spinal mobility in cases associated with LBP.30The most frequently used mode of AE was Pilates, which provided position methods that focus on pelvic stability at the waist, including exercises for core muscles and respiratory control, and helped to activate certain muscles. This type of exercise intervention was important to the improvement of pain, disability, and physical and psychological perception of heath and improved stability parameters.31,32Furthermore, high-intensity AE was also found to reduce pain, the disability rate, and psychological stress in patients with LBP.33Short-term daily AE programs that could be used to emphasize postconsciousness and spine self-care were recommended to keep the spine healthy and prevent back pain.34Long-term WBV exercise was marketed as an intervention for patients with chronic LBP and improved spine strength and endurance, trunk proprioception,and transversus abdominis activation capacity.35Likewise,long-term WBV exercise was an effective, safe, and suitable intervention for seated working employees with chronic LBP.36Low-frequency vibrating board therapy was also used to improve postural stability, physical function, health-related quality of life(HRQoL),disability, and foot vibration perception threshold for patients with nonspecific LBP.37
Long-term,low-intensity AE is a common form of exercise for patients with LBP.It is used to decrease pain and enhance quality of life. Pilates, one of the low-intensity AE forms, is the most commonly used among patients with LBP. WBV exercise is also currently being promoted as a treatment for patients with LBP.
3.1.2. Tendon injury
Common tendon injuries include rotator cuff tendinopathy,tennis elbow, and Achilles tendinopathy (AT). Rotator cuff tendinopathy is the most commonly diagnosed musculoskeletal shoulder condition and is associated with pain, weakness,and loss of function in the shoulder. Tendon swelling may result from acute overload.38Tendon damage in the shoulder significantly affects function and activities of daily life,including eating, dressing, and working. Tennis elbow, or lateral elbow tendinopathy, is a disorder that affects about 1%-3%of the population.39,40A typical symptom is pain at the lateral epicondyle of the humerus,which is aggravated by loading of the common extensor tendinous origin of the forearm extensor muscles.41AT occurs both in athletic and sedentary people.The incidence among top-level runners has been estimated to be between 7% and 9%.42About 30% of patients who have AT have a sedentary lifestyle.43
Supplementary Table 2 shows that the exercise interventions used for these conditions included concentric and eccentric training, self-management load training, open chain exercise,and closed chain exercise.Long-term isolated eccentric training was beneficial for shoulder function and helped to alleviate pain in patients.44When isolated eccentric training was done with a long-term weekly load increase, results showed significant relief of pain in patients with tennis elbow.Muscle contraction was faster and muscles had better elongation.41,45Eccentric exercise has become the treatment of choice for AT,46because it decreases pain and eliminates the need for surgical intervention.It was effective in about 60%of patients.47In 1 study, Astym therapy, an emerging rehabilitation treatment, was an effective treatment option for patients with lateral elbow tendinopathy, as an initial treatment, and after an eccentric exercise program had failed.48Alfredson's isolated eccentric and Silbernagel's combined concentric-eccentric exercise programs both showed beneficial results for patients with chronic midportion AT.49The mechanism of eccentric training might include changes associated with symptomatic tendinopathy that alter fluid movement within the tendon matrix to disrupt remodeling and homeostatic processes.50Therefore,long-term eccentric training was usually used for tendon injuries in the studies we reviewed.In addition, a self-management program based around a single exercise seemed to be comparable with usual physiotherapy treatment.51When it was performed with loaded exercise, it also decreased pain as measured by the Shoulder Pain and Disability Index.52Open chain, closed chain, and range-ofmovement exercises all seemed to be effective in bringing about short-term changes in pain and disability in patients with rotator cuff tendinopathy.53
Long-term eccentric exercise has proven to be effective in the management of tendon injuries. It is a fundamental therapeutic resource for the treatment of AT and lateral elbow tendinopathy and may represent a promising and feasible tool for treating tendinopathies.
3.1.3. Osteoporosis(OP)
OP is characterized by low bone mass and bone microarchitecture deterioration,leading to bone fragility and an increased risk of fracture. In recent years, OP has become a metabolic bone disease that affects millions of people around the world.54Menopause and aging are associated with low PA,55and a sedentary lifestyle is particularly prevalent in postmenopausal women living in urban areas.56There is evidence that exercise can prevent some of the complications associated with menopause,such as bone loss,loss of physical fitness,and increased risk of OP.57Physical exercise effectively decreases risk factors for falling58and improves balance.59,60
Supplementary Table 3 shows that commonly used forms of exercise for OP treatment include AE, RE, CT, and balance training. The AE and RE programs stimulated bone synthesis and decreased bone resorption in postmenopausal women with OP,but that exercise while wearing a weighted vest was better for improving balance.61Long-term Tai Chi exercise decreased the loss of bone mineral density and reduced the risk of fractures in the study population.62Short-term submaximal AE provided significant improvements in static and dynamic balances in postmenopausal osteoporotic women.63Long-term,low-intensity balance and strength training significantly improved the strength and balance capability of women with OP.16Long-term resistance training and balance training had a direct impact on the habitual walking speed of elderly women with a history of OP.64Supervised long-term, highintensity CT increased bone mineral density and effectively prevented fractures in senior citizen populations.65,66
In summary, short-term, moderate-intensity AE and longterm, high-intensity RE can prevent OP and improve balance capacity,aiding in the avoidance of falls and fractures.
3.1.4. Osteoarthritis(OA)
OA is a chronic degenerative musculoskeletal disease that affects many older people around the world.67In the United States, 33.6% of individuals (12.4 million) age 65 years and older are affected by OA, and this number is projected to increase to 67 million by 2030.68The main symptoms of OA are joint pain, stiffness, physical limitations, and decreased functional ability in middle-aged and elderly patients.69The most common joints affected are the knee and hip joints. The strong relationship between obesity and incident knee and hip OA may in part be explained by the increased load on weightbearing joints experienced by overweight and obese patients.Because OA is a chronic condition that has no effective cure,the clinical management of OA is an enormous challenge.Recent practice guidelines recognize that exercise is a key element of any treatment program for OA.70
Supplementary Table 4 shows the forms of exercise most frequently used for treating OA in the studies we reviewed were aquatic exercise, AE, RE, CT, WBV exercise, and ME.In aquatic exercise protocols, long-term, moderate-intensity treatments significantly decreased body fat proportion,71,72and patients showed significant improvements in pain level,disability,and quality of life.71,73Aquatic exercise was also an option for obese patients because it minimized joint load.74Combined with education, it was effective in improving fall risk factors in older adults.75In addition, an 8-week, dancebased aquatic exercise intervention improved function and cardiorespiratory capacity, and decreased postexercise heart rate and fatigue.76In AE protocols, long-term, low-intensity yoga improved symptoms and function,77,78long-term Tai Ji Quan training improved sleep quality and quality of life,79and swimming and cycling training improved function and decreased pain.69Compared with land-based cycling exercise,long-term regular swimming exercise has similar or even better effects on vascular function and inflammatory markers in patients with OA who tend to have a higher risk of cardiovascular disease.80In RE protocols, long-term strength exercise with gradually increasing intensity improved the motion sense of knee flexion81and lower extremity function in patients with knee OA.82For patients with hip OA, muscle power, walking speed, and cadence significantly increased only in the longterm,high-velocity group.83A WBV exercise program had beneficial effects on the physical performance and neuromuscular control of individuals with knee OA.84Furthermore, long-term WBV exercise in combination with RE was superior to RE in relation to muscle strength and proprioception.85,86ME programs included high-speed resistance training87and balance training,as well as long-term strengthening,functional,and stretching exercises88with gradually increasing intensity.
In short, long-term, low- to moderate-intensity exercise focusing on aquatic exercise improves physical function,comorbidities, and quality of life in patients with OA. WBV exercise is also a treatment protocol for OA.
3.1.5. Hip fractures
Over a lifetime,about one-half of women and one-quarter of men will suffer a fragility bone fracture, mostly owing to falling.89,90Among the most serious and common fractures are hip fractures, which have significant risks of mortality and disability.90Increasing evidence shows that exercise rehabilitation interventions have a positive effect on various functional abilities beyond the subacute stage and even later in the nursing stage.Structured exercise improves mobility after a hip fracture.91
Supplementary Table 5 shows that the forms of exercise used for treating hip fractures were AE, HE, and ME. In HE protocols involving PRT, challenging balance training, and neuromuscular functional training of the lower limbs in part overcame some barriers for rehabilitation.7The HE protocol was sufficient to achieve modest improvement in physical function,92which might improve measures of balance, strength, and bone density and result in moderate to large improvements in physical performance and quality of life.92In addition, specific workstation exercise significantly improved balance and strength, which might decrease the risk of falls and fractures in osteopenia women already at risk.93Among patients who completed standard rehabilitation after a hip fracture, physical function improved modestly 6 months after randomization using a home-based function-oriented exercise program.94ME programs, including traditional PRT, weight-bearing impact training, and balance training, were recommended to decrease the risk factors of falls and fractures.95
In short, long-term, low- to moderate-intensity exercise focusing on balance training helps in the recovery of hip joint function and improves quality of life.
3.2. Metabolic system diseases
Metabolic disorders have become very concerning because they have negative impacts on people's health and life quality.Lifestyle interventions should be the primary strategy for the prevention and treatment of metabolic diseases. Reasonable diet and weight control have been highly recommended as treatments, but doctors and patients have overlooked the role that exercise interventions can play.96Such treatments can help to decrease the risk of developing metabolic diseases and can aid in promoting recovery.
3.2.1. Obesity
Obesity is a condition in which excess body fat accumulates. Simple obesity is related to genetics and lifestyle; secondary obesity is associated with multiple endocrine and metabolic diseases. There are a variety of treatments, including exercise therapy,that can be used to intervene in obesity.97
As Supplementary Table 6 shows,exercise prescriptions for obesity included AE and RE combined with HIIT. In AE protocols,the main exercise form was long term and of moderate to high intensity.Specific forms of exercise included treadmill and stationary bicycle aerobic training, which improved body composition and VO2maxin obese adults,98upregulated muscle apelin expression in obese subjects,99and increased levels serum and platform-based brain derived neurotrophic factor in overweight and obese subjects.100Additionally, aerobic interval training (AIT) was shown to relieve reactive oxygen species from excessive nicotinamide adenine dinucleotide phosphate oxidase sources, and it improved microvascular endothelial dysfunction in obese patients.9RE combined with HIIT was used as an intervention among sedentary, overweight, middle-aged individuals, and it was shown that subjects using this method lost weight by improving the function of acute satellite cells. RE combined with HIIT was better than resistance training alone.101
In short,the exercise methods described usually show positive effects, and the most common exercise form for treating or preventing obesity is AE.
3.2.2. Type 2 diabetes(T2D)
T2D, with its high morbidity and mortality, is developing rapidly worldwide and is becoming a significant health problem.Environmental and lifestyle changes, in addition to the ageing of populations, are generally believed to account for the rapid global increase in T2D prevalence and incidence in recent decades.102Epidemiological investigations demonstrate that there are currently 371 million people with diabetes in the world,and the number is expected to rise to 552 million by 2030.103,104Diet therapy,drug therapy,psychotherapy,and self-care monitoring are commonly used intervention methods.Exercise therapy is also a key treatment for patients with T2D and is considered a cornerstone of treatment for T2D, alongside diet and drug treatments.105
As Supplementary Table 7 shows, exercise forms for T2D were CT, RE, and HIIT. AE protocols included treadmill and stationary bicycle.Long-term CT at a moderate intensity alleviated cellular stress in obese adults,106with no effect on plasma carnosinase content or activity in T2D. This was because the beneficial effects of exercise training on the incidence of diabetic complications were probably not related to a lowering effect on plasma carnosinase content or activity.107RE was usually performed at moderate and high intensity for a long term.This strategy significantly decrease glucose,insulin,and homeostatic model assessment-insulin resistance levels in elderly T2D patients,108and altered acute exercise reaction of monocarboxylate transporter 1 in erythrocytes in patients with non-insulin-dependent T2D.109One session of low-volume HIIT was carried out on a cycle ergometer as an intervention for participants with T2D,and this method had immunomodulatory effects and provided potential anti-inflammatory benefits.110
The most common forms of exercise for treating T2D are AE and RE. Long-term exercise at moderate intensity also shows positive effects in treating T2D patients.
3.2.3. Type 1 diabetes(T1D)
T1D, is the archetypal example of a T-cell-mediated autoimmune disease characterized by selective destruction of pancreatic β cells.111The pathogenic equation of T1D shows a complex relationship between genetic and environmental factors, most of which have not yet been determined.111Insulin therapy, psychotherapy, and exercise therapy are intervention methods for treating T1D.
As shown in Supplementary Table 8, HIIT and speed endurance training were the exercise methods used to treat T1D.Cycle sprint training was used as a common speed endurance training method. In the HIIT protocol, cycle sprints with acute interval training carried out on cycle ergometers with high intensity showed a positive effect in that the intervention rapidly decreased patients' perception of subsequent hypoglycemia and reduced their cognitive dysfunction caused by hypoglycemia.112However,speed endurance training also showed a negative effect in that it reduced Ca2+-ATPase in skeletal muscles.113
To sum up, long-term speed endurance training at high intensity can improve T1D.
3.2.4. Nonalcoholic fatty liver disease(NAFLD)
NAFLD,the most common chronic liver disease in the world,is predicted to become the most frequent indication for liver transplantation by 2030.114The disease includes a wide range of liver manifestations, including simple steatosis (also known as nonalcoholic fatty liver), nonalcoholic steatohepatitis, and liver cirrhosis,which may eventually develop into hepatocellular carcinoma. The American Association for the Study of Liver Diseases proposes that exercise can decrease hepatic steatosis in patients with NAFLD.115
As Supplementary Table 9 shows,exercise prescriptions for NAFLD included AE and CT. AE was the main intervention used for NAFLD and was usually performed at moderate to high intensity for both long-term and short-term treatments.Using moderate- and high-intensity AE also decreased the patients'risk of developing NAFLD116and yielded small beneficial effects on intrahepatic triglyceride content.117A 1-year program of AE intervention significantly decreased intrahepatic triglyceride levels and decreased abdominal obesity and blood pressure in obese patients with NAFLD in the moderate exercise group.118In addition, CT decreased intrahepatic triglyceride in patients with NAFLD.119
To summarize,AE and CT usually showed positive effects,and the most common exercise form used for NAFLD was long-term AE at moderate intensity.
3.3. Cardio-cerebral vascular system diseases
In recent years,the incidence of cardiovascular and cerebrovascular diseases has increased rapidly.Although cardiovascular and cerebrovascular diseases mainly occur in the elderly, they can also occur in young people.Proper exercise can improve the efficiency of heart and lung operation, speed up blood circulation,increase the oxygen supply to the whole body,and improve the elasticity of blood vessels. In addition, exercise can lower blood lipids and prevent arteriosclerosis and thrombosis.120The effects of exercise help to relieve stress on the heart and effectively prevent cardiovascular diseases.
3.3.1. Coronary artery disease(CAD)
CAD, also known as ischemic heart disease, refers to a group of diseases including stable angina, unstable angina,myocardial infarction, and sudden cardiac death.121CAD is the most common type of cardiovascular disease.122Recent research has shown that exercise is an effective way to enhance cardiopulmonary function and improve the overall quality of life for these patients.123
As shown in Supplementary Table 10,exercise interventions for CAD included AE and HE. The most common forms of exercise included walking,cycling,jogging,and Tai Chi.Longterm, moderate-intensity walking exercise decreased the severity of sleep apnea in CAD patients.124HIIT reduced the morbidity and mortality of CAD and prevent atherosclerosis.125It had beneficial effects on heart function and quality of life in patients and did not increase the risk of cardiovascular diseases.15,126Compared with aerobic continuous training, AIT was more effective for the rehabilitation of patients with CAD in earlier smaller trials,but in another study,the investigators found that similar improvements in exercise capacity and peripheral endothelial function after AIT and aerobic continuous training in a large population of CAD patients.127,128Long-term HE was superior to traditional hospital-based cardiac rehabilitation among the hospital group in terms of VO2maxand PA, which was more beneficial for postoperative recovery.129Networkbased family cardiac rehabilitation procedures were feasible and effective in improving the PA of patients with CAD.130
In short, exercise interventions usually improve CADrelated risk factors,such as body composition and blood pressure. Compared with moderate continuous training, long-term AE or HE is more effective in improving the physical condition of patients with CAD.
3.3.2. Stroke
Stroke, also known as cerebral vascular accident, is an acute cerebrovascular event, including ischemic and hemorrhagic stroke. The treatment of the acute phase is mainly thrombolysis.After the acute phase,stroke has a very high disability rate.Early exercise intervention after the acute phase is extremely important for the recovery and improvement of exercise capacity.131
As Supplementary Table 11 shows, the types of exercise intervention for stroke were AE, RE, CT, and RE combined with balance training.The forms of exercise included walking,cycling,jogging,power sports,Tai Chi,moving objects in the home, and picking up objects. In AE protocols, moderateintensity aerobic cycle dynamometer training improved the aerobic capacity and walking ability of stroke patients with hemiplegia132and had a positive effect on the cognitive ability and exercise control ability of patients with hemiplegia.133,134Vigorous AE was also a method used to effectively improve the aerobic capacity of stroke patients with hemiplegia.135In RE protocols, after long-term PRT combined with balance training, the patient's balance ability was improved in 3 months and the stroke patients' walking ability improved in 3-6 months.136Low-intensity RE with balance training was beneficial for improvement in plasma lipids, glucose, and exercise capacity.137Short-term respiratory muscle training combined with routine physical training improved lung function and exercise capacity.138Long-term CT improved cognitive ability and reduced mild cognitive impairment in patients with stroke hemiplegia.139
In brief, exercise interventions usually improve cardiopulmonary function,walking ability,balance function,and cognitive ability in stroke patients. Long-term, low- to moderateintensity AE improves cardiopulmonary function and aerobic capacity and is the most common training method used among stroke patients.
3.3.3. Chronic heart failure(CHF)
CHF refers to the inability of the blood to return to the heart owing to the low relaxation and contraction function of the heart, resulting in venous system deposition and insufficient arterial perfusion,thereby causing cardiac dysfunction.140The traditional view is that patients with poor heart function should avoid exercise and reduce the stimulation of the heart; however,with continuous developments in sports therapy research,it is now believed that patients with CHF should exercise moderately.
Supplementary Table 12 shows that the types of exercise methods used for CHF included AE,RE,and HIIT.In AE protocols, long-term walking with breathing exercise improved blood oxygen saturation and internal perception, and adjusted mood and quality of life.141Long-term, moderate-intensity stretching combined with cycling improved and enhanced muscle metabolic reflex control.142HIIT protocols improved the patients' quality of life by changing their levels of health.143HIIT combined with continuous moderate-intensity aerobic training improved the index of submaximal exercise capacity.144HIIT was easy to implement and was a welltolerated exercise intervention in cardiac rehabilitation, but it was not more effective compared to continuous AE.145Longterm HIIT combined with strength training, which is conductive to aortic dilatation ability and increased systolic blood pressure, was more beneficial for vascular response.146,147In RE protocols, short-term, low-intensity resistance activities and abdominal exercise improved cardiac function indicators and lung function and had significantly positive benefits for the rehabilitation of elderly and middle-age patients with CHF after acute decompensation.148Long-term AE and RE were more beneficial for the rehabilitation of patients.149
In short, exercise interventions usually improve heart and lung function in patients with heart failure.Compared with continuous AE training or no exercise, HIIT improved the cardiac contraction function and quality of life. Long-term, HIIT is often used to treat patients with CHF.
3.4. Nervous system diseases
Nervous system disorders mainly include central nervous illnesses and diseases, as well as peripheral nervous system diseases, which are often associated with motor control and cognitive dysfunction.Most of these diseases are chronic,with a high disability rate that disrupts the normal life of patients.Exercise is the most common physiological stimulus in humans,because it has the capacity to regulate and reshape tissue function.The patient's motor control abilities can be improved with exercise, and some studies have determined that exercise can also enhance the patient's cognitive function.150
3.4.1. Parkinson's disease(PD)
PD is a common neurodegenerative disorder that brings with it the prominent loss of the dopaminergic neurons in the substantia nigra pars compacta,which is mainly manifested by motor dysfunction, such as rest tremor and muscular rigidity.151Although medication is currently preferred as a treatment, exercise has drawn more and more attention as a potentially important treatment.
The exercise protocols for patients with PD are summarized in Supplementary Table 13. AE, RE, and ME had some positive effects on patients with PD. AE protocols included walking and the use of bicycles and treadmills. These forms of exercise were usually performed under moderate to high intensity for a long term. AE usually showed positive effects on patients' walking capacity, exercise function,152,153velocity,and step length.154AE also improved the executive ability of patients with cognitive impairment.155Additionally, AE was used for early rehabilitation.156RE involved treadmill training with load or used other machines under moderate to high intensity for short-term and long-term interventions.In regard to cardiovascular function, RE was shown to be safe and improved the patients' physical performance.157-159ME protocols comprised tango, treadmill, cycle ergometer, Tai Chi,Pilates, and boxing. These protocols were performed both as short-term and long-term interventions. They were easy to implement160and yielded some benefits related to motor function,executive function,and balance.160-162A research study reported that aquatic exercise was feasible for individuals in the early stages of PD.163
Long-term AE is frequently prescribed as a treatment for patients with PD and may alleviate PD symptoms.
3.4.2. Huntington's disease(HD)
HD is an inherited disease resulting in neuron apoptosis,which is characterized by jerky and uncoordinated movements of limbs. Unfortunately, there is no effective treatment.164AE, a combination of AE and RE, and ME can partially alleviate the symptoms of HD, although all these types of exercise are challenging for HD patients, who typically have difficulties in engaging in regular PA.165
As shown in Supplementary Table 14,AE was usually performed long term using moderate-intensity interval training or HIIT. A dosage of 3 times each week for 25-30 min per session yielded improvement in cardiovascular function166and skeletal muscle mitochondrial function167and maintained a stabilization of motor function.166,167In another study, AE was combined with RE long term at moderate intensity,which benefited cognitive ability and walking.168In the third study,long-term ME was provided,which included AE,RE,stretching exercise,and task-specific training.Some of these exercise methods proved beneficial for HD patients.169Surprisingly,the task-specific training did not elicit any effect on HD. The results may have been affected by the insufficiency of the exercise program.170
In short, long-term ME is often prescribed as a novel exercise treatment for HD.
3.4.3. Alzheimer's disease(AD)
AD is a progressive neurodegenerative disease that starts slowly.171AD patients usually show memory impairment,aphasia, impaired visuospatial skills, executive dysfunction,and personality and behavioral changes, all of which become worse over time and eventually lead to death. Currently, the main treatment of AD is drug therapy, which has not shown satisfactory efficacy because the underlying mechanism of AD is still unclear. However, if patients with AD exercise regularly and systematically, the cognitive, functional, and behavioral symptoms of AD can be reduced.172
As shown in Supplementary Table 15, exercise interventions for AD included AE, ME, and HE. The forms of AE included the use of bicycles and treadmills. As expected, AE improved the patients'daily activity ability and cognition,173a change that was independent of the change in Aβ species and total tau protein in cerebrospinal fluid. Long-term balance exercise was also prescribed,and improved the patients'exercise capacity.174Long-term ME significantly improved upper and lower body muscle strength and flexibility, agility and dynamic balance, as well as the endurance fitness, gait,and balance abilities of patients with AD.175Long-term, customized HE decreased the risk of falling in the late stage of the disease176and improved the executive function of community-dwelling older people with memory disorders.177It also had beneficial effects on the physical functioning of patients with AD without increasing the total costs of health and social services or causing any significant adverse effects.178
A wide variety of HE is widely used among patients with AD to increase their ability to carry out daily activities and improve their cognitive function.
3.4.4. Depression
Depression is a complex, debilitating disease that affects more than 120 million people worldwide.179Compared with healthy people, people with depression have a much higher risk of developing complex chronic diseases,such as diabetes,cardiovascular disease, and hypertension, which can significantly decrease their quality of life.180Clinical studies have shown that traditional depression treatments do not yield satisfactory outcomes.Emerging evidence shows that exercise may be a promising treatment for depression.181
Supplementary Table 16 shows that long-term AE treatments for depression included the use of cycling, treadmills,and other exercise machines at moderate to high intensity.These exercise methods were effective treatments for positive valence symptoms in major depression.182The combination of AE and sertraline improved the management of late life major depression183and cognitive abilities,184decreased the disability rate,184and improved quality of life.185
In conclusion,long-term,moderate-intensity AE can effectively relieve depressive symptoms and is widely used in the treatment of depression.
3.4.5. Anxiety disorders
The number of patients diagnozed with anxiety disorders is increasing rapidly worldwide.186Patients with anxiety disorders often not only suffer from severe anxiety disorder, but also have poor metabolic function.187Epidemiologic investigations have shown that anxiety is one of the world's most common mental illnesses.188Psychotherapy and medication are usually used for the patients with anxiety disorder.
As Supplementary Table 17 illustrates, the types of exercise interventions used for anxiety were AE,HE,and RE.The forms of AE included cycling, walking, and Tai Chi at moderate to high intensity in long-term doses. Moderate-intensity AE might be a temporary alternative to psychotherapy to decrease anxietyrelated psychopathology.189Long-term HE exercise program had a positive effect on the metabolic index and anxiety level of anxiety patients in Taiwan, China.190For the patients with an anxiety disorder, RE was performed at low to high intensity acutely or for a short term with a frequency of 2 times per week.So,RE was a low-risk and feasible method to reduce anxiety symptoms in patients with general anxiety disorder.191,192
In short,moderate-intensity AE and RE can be used to help patients with anxiety disorders.
3.5. Respiratory system diseases
Respiratory system diseases are common diseases that seriously endanger human health.193Some stretching and chest expansion exercises can enlarge the thorax and increase the strength of the respiratory muscles. It is beneficial to increase lung capacity,lung ventilation,and oxygen utilization capacity to improve the working function of the lungs.194,195
3.5.1. Chronic obstructive pulmonary disease(COPD)
COPD is a devastating lung disease characterized by incomplete reversible airflow limitation. The main symptoms are chronic cough, cough with sputum, dyspnea, wheezing,and chest tightness. COPD intervention methods mainly include drug therapy,oxygen therapy,and exercise therapy.196
As shown in Supplementary Table 18,exercise prescriptions consisted of individualized AE, RE, and water-based exercise.The forms of exercise included strength training with a pedal exerciser, Tai Chi, and ground-based walking. Patients with COPD individually received long-term, low-intensity physical outpatient training to improve their athletic ability and quality of life.197Endurance and strength training were performed at high intensity for a long term, which significantly improved endurance.198Long-term water-based exercise at low intensity constituted a relatively new concept in the management of patients with COPD,and the aquatic environment was well accepted by COPD patients with physical comorbidities.199Strength training with a pedal exerciser was performed at low intensity for a short term,which improved the muscle strength,balance,and exercise ability of frail elderly patients.200In addition, long-term Tai Chi exercise enhanced lung function, exercise capacity,and diaphragm strength.201The results of another study showed that training in ground-based walking was an effective method for improving the quality of life and endurance of patients.202
In brief,patients with COPD can use long-term AE or RE at a low to moderate intensity,combined with training in breathing, to promote disease recovery. Also, water-based exercise is a novel way to treat COPD.
3.5.2. Interstitial lung disease(ILD)
ILD is a group of diseases in which pulmonary interstitial lesions are the main lesions. The chief clinical manifestations are cough and postoperative dyspnea, which often aggravates the condition and eventually leads to respiratory failure. Glucocorticoids combined with immunosuppressive therapy,antifibrotic drug therapy,lung transplantation,Chinese herbs,oxygen inhalation, and exercise therapy are intervention methods used to treat ILD.203
As Supplementary Table 19 shows,the exercise method used for ILD was supervised CT. The supervised exercise protocol consisted of long-term, high-intensity AE and resistance training for upper and lower limbs. This method of exercising was effective in patients across the range of ILDs, with clinically meaningful benefits in asbestosis.204Another study provided certainty regarding the role of in ILD.The results from another study showed that supervised exercise training could be used to inform and optimize the clinical management of people with ILD.205
In short,long-term high-intensity CT can be used to relieve symptoms of ILD patients.
3.5.3. After lung transplantation(LTx)
LTx is a treatment option for patients with end-stage lung disease. Over the past 15 years, with the gradual maturity of lung transplant techniques, donor preservation,and perioperative management,the 1-year survival rate of LTx has increased from 70% to 85%.206However, there are typically complications after LTx that endanger the patient's health and affect the patient's recovery. Proper exercise can prevent the occurrence of complications and improve the speed of postoperative recovery.
As shown in Supplementary Table 20, exercise methods included WBV exercise and CT. As a feasible and safe exercise modality,short-term WBV exercise was also shown to be a good method for helping patients recover from LTx.207The forms of CT included cycling, walking, and stair climbing, as well as using leg press equipment. The results of this study showed that supervised endurance strength training immediately after discharge improved functional recovery after LTx in postoperative patients and also improved the body function of patients within 1 year.208
In a word, long-term moderate-intensity CT after LTx improves patients in daily activity,and short-term WBV exercises also have good effects.
3.6. Urinary system diseases
Patients with kidney diseases are characterized by poor physical strength,malnutrition,and a lack of energy.Research shows that exercise can improve the body's function,promote multiple systems,and improve the life quality of patients with kidney disease. Owing to the lack of a comprehensive understanding of the disease,which eventually leads to dysfunction of other systems,most patients with kidney disease need more exercise.209,210
3.6.1. Chronic kidney disease(CKD)
CKD is a structural or functional abnormality of the kidney. CKD is a compound disease that affects multiple organs and systems in human body.211Additionally, the lack of exercise and low body function in patients with CKD is an important cause of deterioration.209
Supplementary Table 21 shows that the types of exercise intervention used for CKD were mainly AE,RE,CT,and HE.In AE protocols,short-term,moderate-intensity AIT was used to intervene in patient with CKD Stage 3. The results seemed to show reduced levels of endothelin-1.212The vasoconstriction function of endothelin-1 is an important factor in cardiovascular disease. In RE protocols, long-term progressive RE was a tolerable intervention for overweight patients with chronic nephropathy. Progressive RE increased muscle the anatomic cross-sectional area, muscle volume, knee extensor strength, and exercise capacity.213For patients with CKD without deterioration of renal function, modest CT improved the physical performance and avoided muscle wasting.214In HE protocols, home-based CT was feasible and improved muscle strength and exercise capacity of patients with CKD.215-217Additionally, moderate-intensity home-based aerobic training improved the patients'VO2maxand quality of life,although it did not change endothelial function or arterial stiffness.218Similar studies suggested that AE was effective in decreasing visceral fat in patients and improving cardiopulmonary function.219,220
Long-term, moderate-intensity HE has a promising effect on CKD, as reflected by improvements in muscle strength,enhanced metabolic capability, regulation of mood, and decrease in other complications.
3.6.2. After kidney transplantation
Kidney transplantation is the most effective way to treat patients with end-stage renal disease and chronic renal failure.221However, patients sometimes experience organ rejection after surgery, so they need to take immunosuppressive agents to maintain a normal physiological status.These agents sometimes have an ill effect on the patient's physical condition.Recent research shows that regular exercise has a positive effect on kidney transplant patients.222
Supplementary Table 22 shows that the types of exercise intervention for kidney transplantation included AE, RE, and individualized progressive exercise programs. Aerobic and resistance training studies have shown that this type of training is feasible and is an effective treatment that regulates pulsewave velocity.223The combination of walking on a treadmill and low-intensity dynamic stretching was beneficial to the physical and psychological rehabilitation of the patients.In addition,this individual intervention method could be appropriately extended to other patients after renal transplantation.224
The exercise regimens described often had a positive effect on patients who have undergone kidney transplantation by improving their movements and limiting the complications they experienced.
3.7. Cancers
Cancer is a major cause of death in the United States and many other parts of the world. In the United States, cancer causes one-quarter of all deaths.225Increasing numbers of new cancer cases and increasing cancer survival rates have led to a large and rapidly growing population with unique health care needs. PA has emerged as an effective strategy for improving the quality of life,both in physical and emotional terms,among cancer survivors and among those diagnosed with several forms of cancer,including breast,colon,prostate,and lung cancers.
3.7.1. Breast cancer(BC)
BC is the most commonly diagnosed cancer and is the leading cause of death in female patients with cancer around the world. Because anti-cancer treatments and diagnostic technologies have progressed, patients with BC now live longer.226It is well known that patients with BC suffer from many cancer-and treatment-related side effects, all of which worsen their overall quality of life.227,228Exercise is considered to be an effective supportive treatment for patients with BC.229
Supplementary Table 23 shows that the main methods of exercise for patients with BC were AE,RE,and CT.The forms of AE included the use of cycle ergometers, treadmills, elliptical machines,and rowing ergometers.Long-term,high-dose exercise led to loss of fat, improved cardiopulmonary function, and reduced the risk of BC.230-232Short-term,low-intensity AE combined with muscle strength enhancement helped to improve shoulder joint mobility and alleviated BC-associated lymphedema and pain.233Long-term,moderate-intensity AE had significant benefits, but only for women with early stage BC.234In 1 study, long-term, PRT of moderate intensity using 8 different machines was especially an important part of supportive care.229,235-237Moderate-intensity AE combined with RE benefited early adjuvant BC treatment;after 18 weeks of an exercise program,there was a positive effect on physical fatigue,cardiopulmonary function,and muscle strength among participating patients.238High-intensity AE combined with RE significantly improved patients'self-confidence,physical fitness,body composition,and chemotherapy completion rate.At the same time,this form of exercise helped to improve sleep quality in patients with BC undergoing chemotherapy.239-242
In short,for patients with early BC,long-term,low-to moderate-intensity AE and RE are more conducive to patients'rehabilitation.
3.7.2. Colon cancer
There are 103,000 people diagnosed annually with colon cancer in the United States.238Among these diagnosed cases, 39%will have localized colon cancer (confined to the primary site,Stages I-II),36%will have regional colon cancer(the cancer has spread to the regional lymph nodes;Stage III),and 20%will have metastatic disease(the cancer has spread to distant organs,Stage IV).243,244The 5-year survival rates for localized and regional colon cancer are 90% and 70%, respectively.243Observational studies indicate that higher volumes of PA are associated with improved disease outcomes among colon cancer survivors.245
Supplementary Table 24 indicates that the main forms of exercise used for patients with colon cancer were AE and CT.Long-term, moderate-intensity AE reduced the visceral adipose tissue content, increased health-related fitness, and reduced the recurrence risk of colon cancer among patients with Stages I, II, and III disease.246,247Long-term, moderateintensity, high-dose AE improved the favorable prognosis of biomarkers and the multiple HRQoL outcomes of patients with colon cancer.248,249Long-term CT had a beneficial effect on reducing patient fatigue.250Low- to moderate-intensity exercise shortened the length of postoperative hospital stays and improved bowel movement after colectomy.251
In conclusion, for patients with colon cancer, long-term,moderate-intensity, high-dose AE is often used as an adjunct to the treatment of the disease.
3.7.3. Prostate cancer
Prostate cancer is the most prevalent cancer among men in the United States and is the second leading cause of cancer death in men.252Men over 65 years of age account for 64%of new prostate cancer cases in the United States, and men over 75 years of age account for 23%of patients with prostate cancer.253Current treatments include radical prostatectomy,radiotherapy, and androgen deprivation therapy (ADT).Patients need active physical rehabilitation after surgery, and one of the ways they can receive it is through exercise.
Supplementary Table 25 reveals that the main forms of exercise used for prostate cancer patients were AE, RE, and CT. AE increased the PA level of patients and had a positive effect on recovery from disease.254Walking 10,000 paces a day was effective in improving cardiovascular health.255Long-term RE and impact exercise for patients who were treated with ADT decreased their total body fat.256,257The application of ADT in combination with AE and endurance exercise had significant effects on cardiopulmonary capacity,258resting fat oxidation and glucose,259body composition,260and improvement of fatigue.261Short-term exercise helped to maintain the sexual activity of patients with ADT.262,263In addition,long-term,high-intensity exercise significantly improved the peak oxygen uptake and provided more sustainable cardiopulmonary efficacy than low-intensity exercise.264
In summary,for prostate cancer patients,long-term,moderate- and high-intensity CT is often used to assist in the treatment of diseases.
3.7.4. Lung cancer(LC)
LC is the leading cause of cancer-related deaths in men and women in the United States, with an estimated 158,040 deaths from LC in 2015.265The LC mortality rate exceeds that of colon,breast,and prostate cancers combined.Exercise has been shown to improve blood immune function in LC survivors.266
As Supplementary Table 26 shows, the main forms of exercise used for LC patients were HE, AE, CT, and HIIT. Longterm home-based,moderate-intensity walking was a feasible and effective intervention for managing anxiety and depression among patients with LC.267Long-term Tai Chi helped to improve the proliferation and cell-dissolving activity of peripheral blood mononuclear cells in patients,268it decrease body fatigue and physical fatigue, and it increased the vitality of patients.269After receiving supervised CT, the patients' pain was decreased,but no improvement in HRQoL.270However,in another study, long-term, moderate-intensity AE or RE had a good effect on HRQoL, physical and psychological symptoms,and tumor treatment effects.271Home-based,moderate-intensity RE delayed the deterioration of body function and improved muscle strength among patients with advanced LC.272Patients receiving short-term, high-intensity endurance training and strength training conducted within 5-7 weeks after their operation had good tolerance to the protocol.273Other studies have shown that preoperative HIIT can significantly improve AE,but cannot reduce early complications after LC resection.274,275
In brief, for the exercise prescriptions for LC, long-term,moderate- and high-intensity AE or RE is commonly used as adjuvant therapies.
4. Discussion
We have described several types of exercise interventions and their uses in the treatment of various diseases (Table 2).Exercise has a positive effect on many diseases, especially chronic noncommunicable diseases, which is consistent with the results of Pasanen et al's study.276The clinical significance of exercise intervention is worthy of affirmation. Compared with the huge cost of drugs, exercise intervention is an economic and safe way to prevent and treat diseases,and has few side effects, which reduces the economic burden on families and society. However, not all diseases can be improved by exercise therapy, which sometimes can only be used as an adjuvant treatment for major illness. At present, the types of exercise interventions used as treatments are mainly AE, RE,and CT. Different types of training methods have their own characteristics.For instance,AE primarily enhances cardiopulmonary function, and RE primarily enhances muscle strength and increases basal metabolic rate.
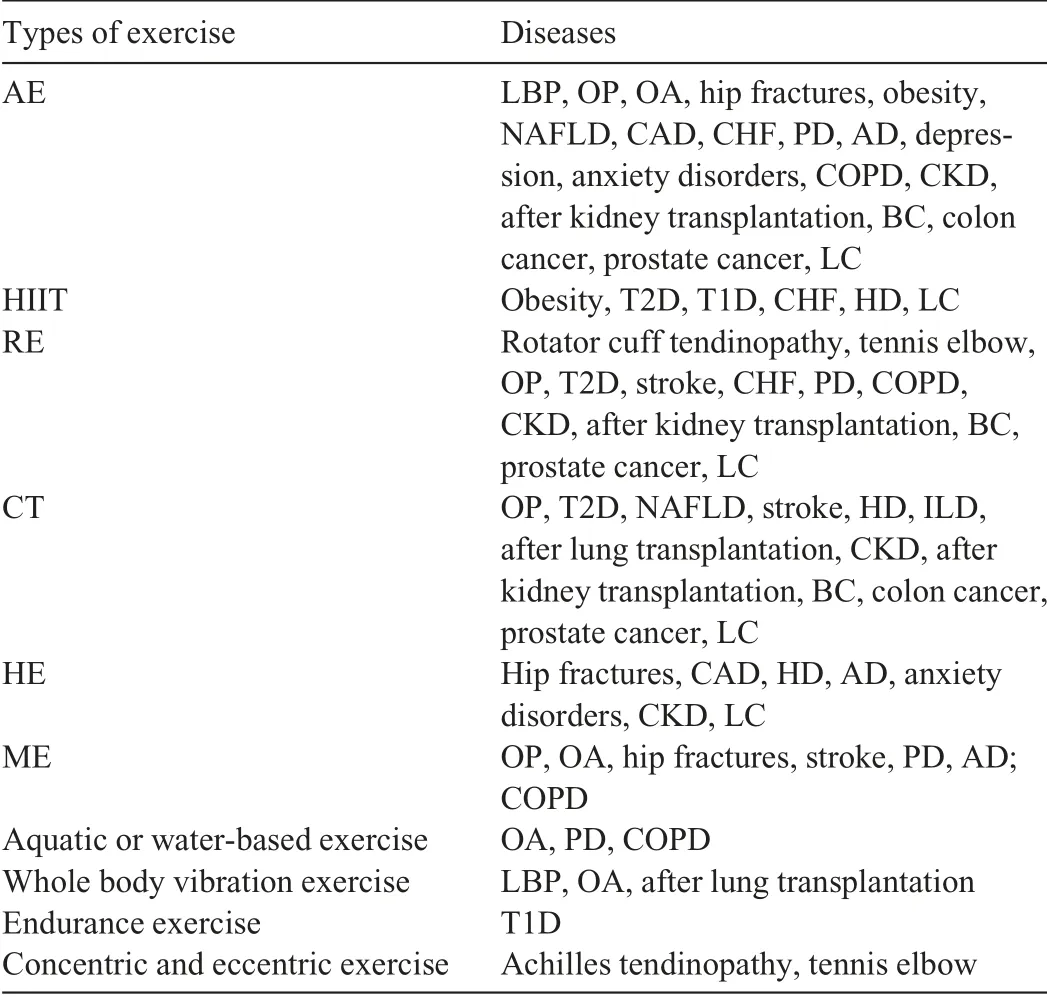
Table 2 Types of exercise for various diseases.
However,avoiding injury is more important than engaging in exercise. Measures for preventing patient from injuries should be taken. When designing an exercise program, we should conduct a comprehensive evaluation of the patient,exclude all possible contraindications,and select the appropriate type and intensity of exercise. During the training, we should keep an eye on the patient's adaptation to the intensity of the exercise and follow the principle of gradual training by starting with a low intensity and gradually increasing the load.The joint efforts of researchers in related fields can help to design the optimal exercise treatment for each individual,yielding a personalized exercise protocol that will help alleviate the symptoms of the illness and improve the patient's quality of life.
There are some limitations to the selection process we used for this review.In screening the articles,we focused on identifying studies that reported on RCTs and ignored comprehensive and systematic reviews or meta-analyses. The reviews and meta-analyses we omitted may have provided additional disease-specific findings. Thus, the search strategy we used may not have identified all relevant studies.
5. Conclusion
Exercise therapy is a safe method for improving patients'physical performance and alleviating the symptoms of diseases.In this article,we identified the exercise intervention methods used for 26 common diseases and described the main characteristics of each exercise prescription. We then compared the effects of the various exercise intervention methods on the patients' conditions and selected the recommended forms of exercise to prescribe. For future studies, people should focus on the role of exercise therapy in the prevention of diseases and provide guidance for family doctors and health management consultants that will help them to develop personalized and targeted exercise prescriptions for disease prevention.
Acknowledgments
The authors thank all the study participants.This study was supported by Natural Science Foundation of China (No.31671242)and the National Key R&D Program of China(No.2018YFC1314701).
Authors'contributions
Both XL and XT participated in drafting,writing,and revising the manuscript;HZ,RH,and NL made edits and comments to the manuscript; RW and PC helped conceive of the design,provided funding for the study, and helped to draft the manuscript.All authors have read and approved the final version of the manuscript, and agree with the order and presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Supplementary materials
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jshs.2019.04.002.
Manuscript translated in Chinese
The Chinese version for this article can be found in the online version at doi:10.1016/j.jshs.2019.04.002.
 Journal of Sport and Health Science2019年5期
Journal of Sport and Health Science2019年5期
- Journal of Sport and Health Science的其它文章
- Biomechanics of ankle giving way:A case report of accidental ankle giving way during the drop landing test
- Dynamic knee valgus kinematics and their relationship to pain in women with patellofemoral pain compared to women with chronic hip joint pain
- Influences of load carriage and physical activity history on tibia bone strain
- Effects of intermittent sprint and plyometric training on endurance running performance
- The relationship between transport-to-school habits and physical activity in a sample of New Zealand adolescents
- Cardiorespiratory fitness and cancer in women:A prospective pilot study
