Breast metastasis from primary lung adenocarcinoma in a young woman: A case report and literature review
Diego Enrico, Silvia Saucedo, Inés Bravo
Diego Enrico, Department of Clinical Oncology, Eva Perón General Hospital, 3200 Balbín Avenue, San Martín 1650, Buenos Aires, Argentina
Silvia Saucedo, Inés Bravo, Department of Pathology, Eva Perón General Hospital, 3200 Balbín Avenue, San Martín 1650, Buenos Aires, Argentina
Abstract
Key words: Lung cancer; Breast metastasis; Immunohistochemistry; Lymphatic spreading;Case report
INTRODUCTION
Primary breast cancer is the most common malignancy in adult females. However,metastatic involvement of the breast is a rare phenomenon, with a reported frequency of approximately 0.2%-1.3%[1]. A variety of neoplasms have been reported to metastasize to the breast, including malignant melanoma, lymphoma, lung, ovary,prostate, kidney, stomach, ileum, thyroid, and cervical cancer[2]. Despite its rarity,metastatic breast disease from lung adenocarcinoma poses a significant diagnostic dilemma.
Lung cancer is the leading cause of cancer death, with one of the highest incidences.However, to date, there have been a few published cases of lung adenocarcinoma metastasizing to the breast. We report the case of a patient with breast metastasis from primary lung adenocarcinoma. To the best of our knowledge, this is the second report of this entity in a woman under 30 years of age.
CASE PRESENTATION
Chief complaints and history of illness
A 29-year-old nonsmoking nurse presented with a 3-wk history of dry cough to the Eva Perón General Hospital, San Martín (Buenos Aires), Argentina.
Imaging examinations and physical examination
Routine chest X-ray followed by computed tomography (CT) revealed atelectasis in the right middle lobe of the lung, ipsilateral pleural effusion, and enlarged lymph nodes in the mediastinum and right hilum (Figure1). On physical examination, a small mass was noted in the upper outer field quadrant of her right breast. Axillary and cervical chain lymph nodes were not palpable. Mammography did not reveal any suspicious images. However, ultrasonography (US) satisfactorily showed a hypoechoic solid nodule (11.6 mm x 6.6 mm x 8.9 mm) in the right breast, which was biopsied with a trucut needle (Figure2).
The patient underwent bronchoscopy, which revealed submucosal infiltration causing a about 50% obstruction of the right middle lobe bronchus. During the bronchial procedure, washing, brushing and biopsies were obtained. Furthermore,needle thoracentesis was performed.
Based on all this information, the main differential diagnoses considered were a primary breast tumor with lung and pleural metastasis or two synchronous primary tumors.
Cytological findings
All the cytological specimens (pleural effusion, bronchial washing, and bronchial brushing) were stained using the Papanicolaou technique, and the diagnosis of adenocarcinoma was suggested.
Histopathological and immunohistochemical findings
Hematoxylin-eosin (HE) staining and immunohistochemistry (IHC) were performed on formalin-fixed paraffin embedded tissues from bronchoscopy biopsy and coreneedle breast biopsy. On both biopsies (bronchial mucosa and breast), HE-stained paraffin sections revealed infiltration by adenocarcinoma (Figure3). Additionally, no evidence of in situ carcinoma was observed on the breast specimen. IHC (performed on a BenchMark XT autostainer, Ventana Medical Systems Inc, Tucson, AZ) of lung and breast specimens revealed strong immunoreactivity for anti-pancytokeratin AE1AE3, cytokeratin 7 (CK7), thyroid transcription factor-1 (TTF-1), and napsin A.The neoplastic cells lacked expression of cytokeratin 20 (CK20), P63, estrogen receptor(ER), progesterone receptor (PR), HER2/neu, and GATA3 (Figure3).
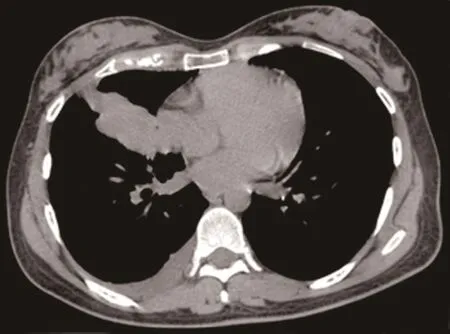
Figure1 Chest computed tomography scan. Atelectasis in the right middle lobe of the lung, ipsilateral pleural effusion, and enlarged lymph nodes in the mediastinum and right hilum.
Molecular findings
Epidermal growth factor receptor mutations in exons 19 to 21 were negative (PCR-based pyrosequencing assay), as was EML4-ALK rearrangement by fluorescencein situhybridization (FISH).
FINAL DIAGNOSIS
The histology and immunohistochemical staining pattern were strongly consistent with metastasis to the breast from primary lung adenocarcinoma.
TREATMENT
In February 2016, the patient was started on treatment with cisplatin and pemetrexed.After an initial response, she experienced lung progression, and docetaxel was used as a second-line therapy to achieve stable disease.
OUTCOME AND FOLLOW-UP
Due to the deterioration of her clinical conditions, a third-line therapy was not feasible, and she continued with palliative supportive care. Her overall survival was 20 mo.
DISCUSSION
Literature review
Since 2000, 63 cases of breast metastasis from a lung adenocarcinoma have been reported in the literature, including our patient (Table1)[1,3-44]. The median age was 56 years (SD 13.4), and as expected, the majority were female (82.5%), while only 8(12.7%) patients with breast metastasis were men.
Of the 43 patients with data about the side of disease, 35 (81.4%) had evidence of disease in both lung and breast on the same side, while 6 (14%) had contralateral and 3 (7%) had bilateral breast involvement. A statistical correlation was observed between the side of the primary lung cancer and the side of the breast metastasis (P<0.001).
The distribution of immunohistochemical markers in the literature is shown in Figure4. The most frequent markers analyzed were TTF-1, CK7, CK20, napsin A, ER,PR, HER2, GCDFP-15, mammaglobin, and GATA3. There were six cases with negative TTF-1, three with negative napsin A, and only one with negative CK7.
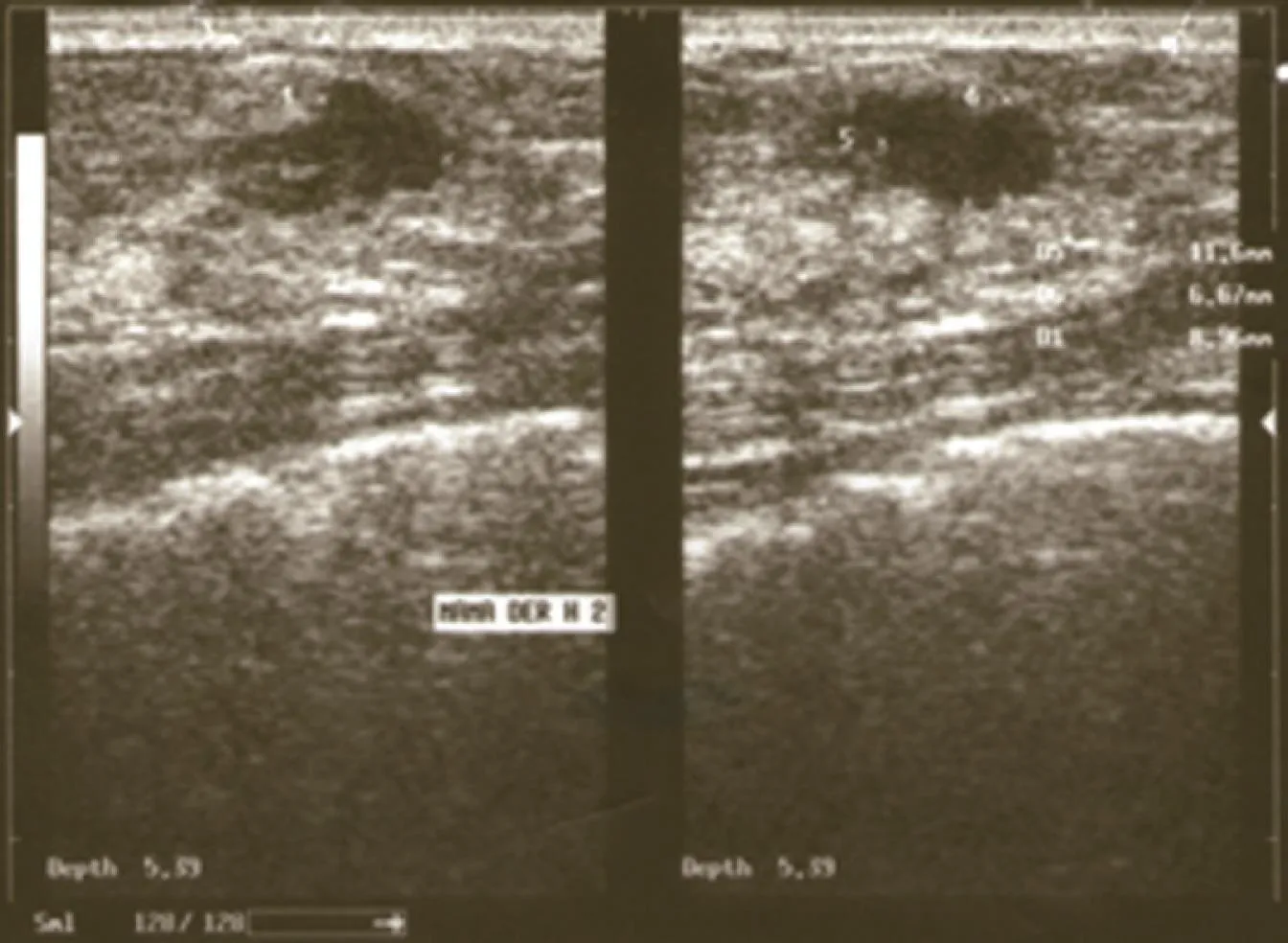
Figure2 Right breast ultrasound. Hypoechoic solid nodule (11.6 mm x 6.6 mm x 8.9 mm).
Discussion
The most common sites of lung cancer metastasis are the bones, lungs, brain, adrenal glands, liver, and extrathoracic lymph nodes, in descending order[45]. However,autopsy series have revealed that lung cancer may metastasize to nearly any organ.Williamset al[46]published the most extensive series, which included 169 cases of metastases to the breast from extra mammary solid tumors and reported that the most common histological type was malignant melanoma.
Distinguishing a breast metastasis from a primary breast cancer, based on mammography, may be extremely difficult since metastasis can mimic a primary malignancy or even a benign lesion. The absence of micro calcifications is considered a characteristic of metastatic lesions to the breast, with the exception of ovarian cancer[47]. On mammography, usually single lesions are observed, but sometimes multiple well-circumscribed lesions may be present[13]. In our case, there were no mammographic findings, and the breast lesion was discovered by ultrasonography.Although most of the lesions do not show any specific histological features, some authors have described different characteristics of breast metastasis from extra mammary malignancies. These features include a circumscribed tumor with multiple satellite foci, the presence of many lymphatic emboli and the absence of an intraductal component, which is the most relevant characteristic[1].
As outlined above, the distinction between metastasis from lung adenocarcinoma and primary breast adenocarcinoma may cause a diagnostic dilemma. For this, the contribution of immunohistochemistry is crucial. There is no single marker with 100%sensitivity and specificity that can solve this problem, hence an immunohistochemical panel is needed. Both breast and lung adenocarcinomas have overlapping CK7+/CK20- immunoprofiles in most cases. The frequency of ER expression in lung adenocarcinoma has been reported to vary from 7.6% to 27.2%, depending on the antibody used[48]. TTF-1 is positive in 73%-88% of lung adenocarcinoma cases, and there are very few reports of its positivity in breast cancer (less than 3% at least weakly or focally)[49]. Napsin A staining has been reported to be positive in 80%-90%of lung adenocarcinoma cases. This marker is usually negative in breast cancer, even though it has been found to be positive in less than 3% of breast adenocarcinoma cases[50]. Although TTF-1 is a reliable marker for lung adenocarcinoma, napsin A is more sensitive and specific. The combination of both markers provides the maximum benefit. On the other hand, 67%-95% of breast cancer cases express GATA3 (43%-73%of triple-negative cases), and its expression in lung adenocarcinomas is less than 10%[51].
Our patient had metastasis to her right breast, which is the same side affected by the malignant pleural effusion, consistent with the hypothesis by Huanget al[25]. To this end, they considered a stepwise mechanism involving parietal pleural seeding,followed by invasion into chest wall lymphatic vessels draining to ipsilateral axillary lymph nodes and retrograde lymphatic spreading to the breast. This mechanism of breast metastasis could be supported by findings of enlarged homolateral axillary lymph nodes. Moreover, Barberet al[52]demonstrated lymphatic communication between the breast and mediastinal lymphatic channels. These hypotheses could be confirmed by the fact that almost 80% of the cases reported from 2000 to date had ipsilateral lesions. Another potential type of spread could be hematogenous.However, if lung cancer spreads through this route, both breasts should have the same probability of being affected. This is not reflected in the reviewed cases, where only 5.4% of patients had bilateral breast involvement. The last possible explanation could be direct tumor invasion through the chest wall to the breast, but chest CT scans did not reveal this alteration in the reported cases. Therefore, lymphatic spreading might be the most reasonable mechanism of lung cancer dissemination to the breast.
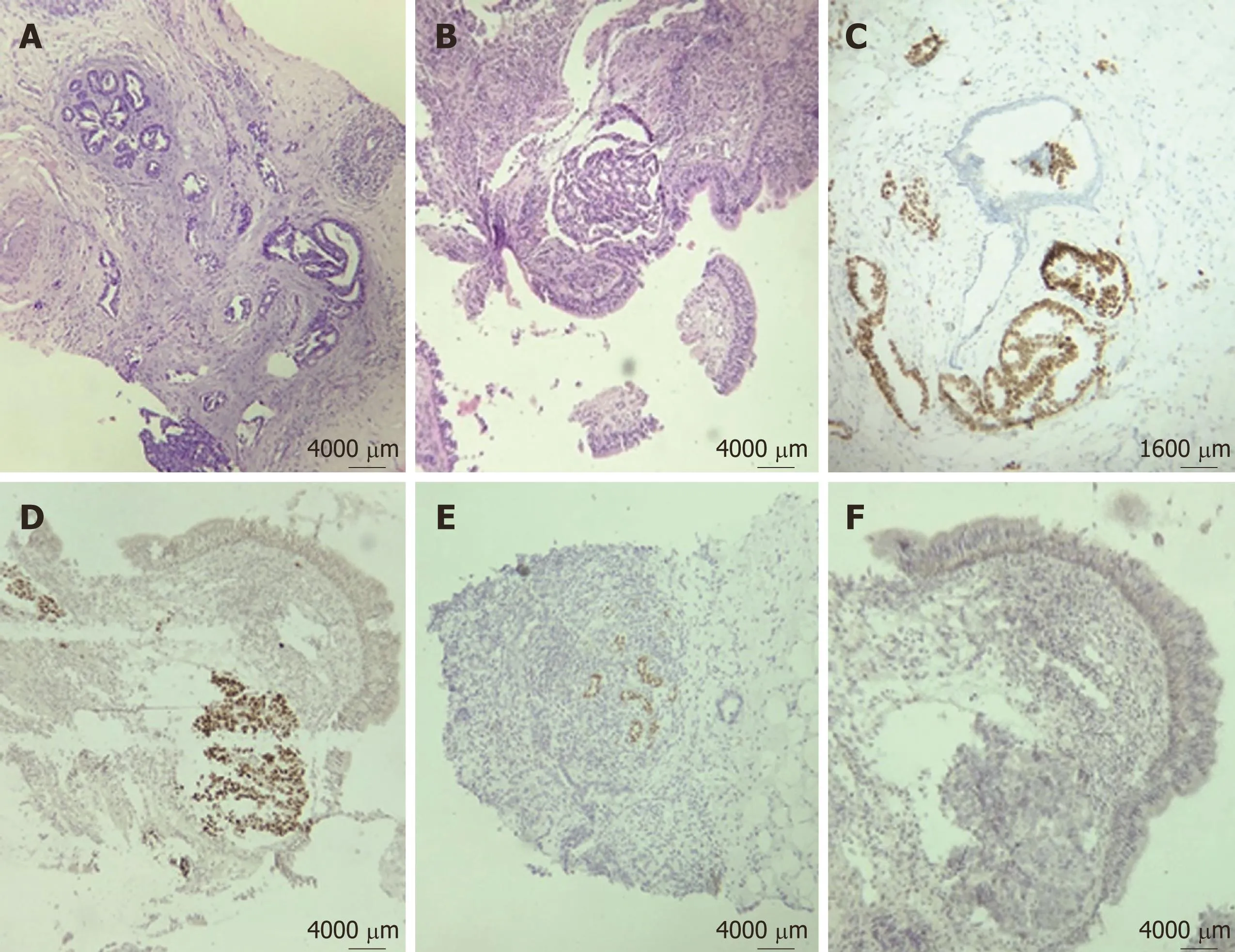
Figure3 Breast biopsy showed adenocarcinoma infiltrating into the adjacent parenchyma. A: Ducts were not involved by the tumor, and no evidence of in situ carcinoma was obtained (x 40); B: Bronchoscopy biopsy (HE) showed poorly differentiated adenocarcinoma (x 40); C, D: Immunohistochemical staining for thyroid transcription factor-1 was positive on both breast (C) and lung specimens (D); E, F: GATA3 staining was negative in both breast (E) and lung tissue (F).
CONCLUSION
Here, we present a rare case of synchronous isolated metastasis to the breast from lung adenocarcinoma in a young patient. This is the second report, together with that by Wanget al[14], in a woman under 30 years of age. Due to the infrequency of this phenomenon, the diagnosis may cause a significant dilemma. Clinical examination,radiological assessment, and pathological evaluation are essential. Nonetheless, in our opinion, immunohistochemistry makes a difference, playing a key role in the accuracy of the final diagnosis.
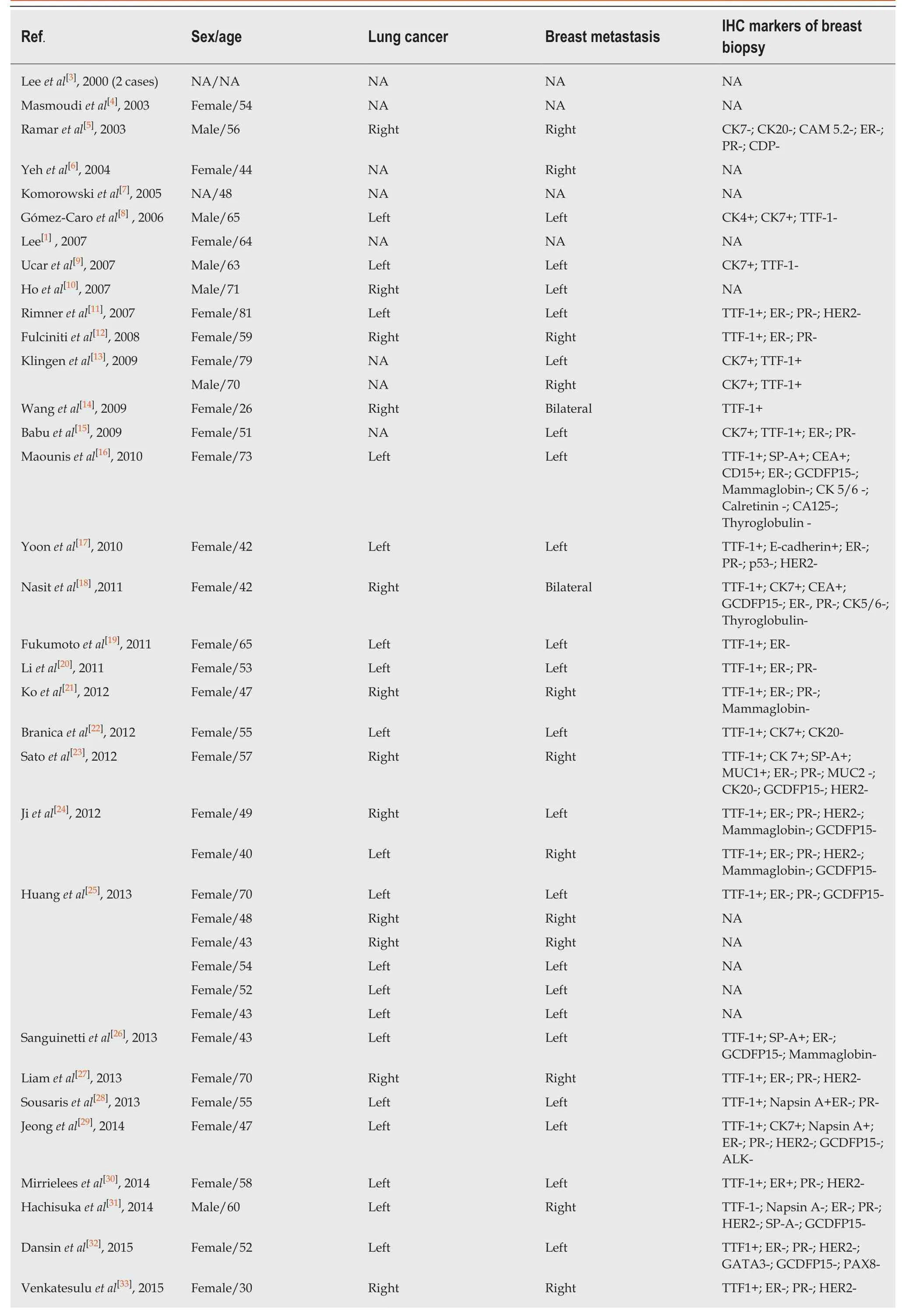
Table1 Breast metastasis from primary lung adenocarcinoma: Literature review 2000-2018
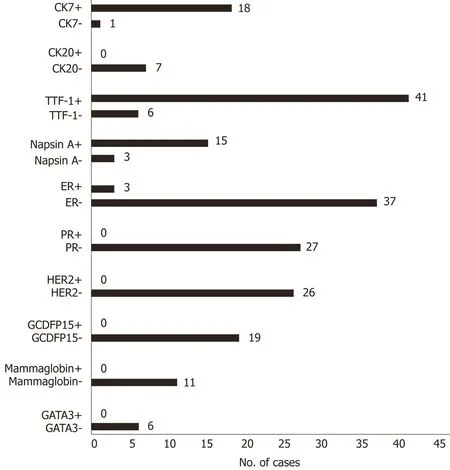
Figure4 Distribution of immunohistochemical markers on the breast biopsies in the reviewed cases (including ours). ER: Estrogen receptor; PR:Progesterone receptor; HER2: Human epithelial growth factor receptor 2; TTF-1: Thyroid transcription factor 1; CK7: Cytokeratin 7; CK20: Cytokeratin 20; GCDFP15:Gross cystic disease fluid protein 15; GATA3: GATA-binding protein 3.