Analysis of 24 patients with Achenbach's syndrome
Fatih Ada, Ferit Kasimzade
Abstract BACKGROUND Achenbach’s syndrome is a rare condition, and the etiology is unknown. It is most commonly seen in the volar plate of the hand distal interphalangeal joint.Patients diagnosed with Achenbach’s syndrome in cardiovascular surgery clinic were retrospectively compared with the literature.AIM To investigate the symptoms, findings, sociodemographic conditions, and laboratory data of patients diagnosed with Achenbach’s syndrome.METHODS The study is a retrospective review of 24 patients diagnosed with Achenbach’s syndrome at Afyonkarahisar State Hospital between March 2015 and November 2016, at Sivas Numune Hospital between November 2016 and November 2017,and at Cumhuriyet University Cardiovascular Surgery Department between November 2017 and November 2018. In the study, demographic characteristics of the patients, signs and symptoms of the disease, and laboratory data were analyzed retrospectively.RESULTS The cohort consisted of 83.33% female patients and 16.67% male patients. The disease was most commonly located in the index finger of the right hand. All of the patients complained of bruising and pain. No pathologic findings were present in the laboratory results. According to these results, it can be concluded that Achenbach syndrome is most commonly seen in the right index finger of middle-aged female patients.CONCLUSION Further research is needed to clarify Achenbach’s syndrome and to develop a diagnosis and treatment algorithm. As the awareness of this syndrome increases,large amounts of data will be obtained. According to current knowledge,Achenbach’s syndrome is not among the known causes of mortality or morbidity.However, it is unknown whether it is seen in brain or other vital organs.
Key words: Achenbach’s syndrome; Blue thumb; Digital hematoma; Digital hemorrhage;Hand; Pulse oximeter
INTRODUCTION
The etiology of Achenbach's syndrome, which is often encountered in the cardiac surgery clinics, yet forgotten during the diagnostic process, is not clearly known. This rare syndrome is frequently neglected in the diagnostic process because the disease does not clearly result in any mortality or morbidity, and therefore it is ignored.However, we are convinced that as the studies on this subject increase (such as studies to enlighten if this syndrome is a precursor to more serious illnesses or to reveal what happens in the vascular bed), the awareness about the disease will also increase.Achenbach’s syndrome is typically characterized by a digital hematoma and bruising that begins suddenly and painfully in one or several fingers and decreases within hours or days. There are no known risk factors such as trauma, drug use, bleeding disorder, or rheumatologic disease associated with the etiology of the syndrome. The disease was named after German doctor Achenbach as it was first diagnosed by him[1].We retrospectively analyzed the data of 24 patients with Achenbach's syndrome in our study and compared with the literature.
MATERIALS AND METHODS
The study is a retrospective analysis of 24 patients diagnosed with Achenbach’s syndrome at Afyonkarahisar State Hospital between March 2015 to November 2016,at Sivas Numune Hospital between November 2016 to November 2017, and at Sivas Cumhuriyet University Cardiovascular Surgery Department between November 2017 to November 2018. It was approved by the local ethics committees. Written consent forms were obtained from all patients. Patient information was obtained from patient cards and the hospital registry system. The anamnesis of the patients was carefully taken and the physical examinations were made to identify vascular and other pathological diseases. Subsequently, arterial and venous Doppler scans of the extremity veins, complete blood counts (to diagnose bleeding disorders), international normalized ratio, prothrombin time, and activated partial thromboplastin time tests were requested. Biochemical parameters were studied. Oxygen saturation was measured at the fingertips of the patients by pulse oximetry. Patients who did not use anticoagulants or antiaggregants in their history, normal Doppler ultrasonographic findings, normal pulse oximeter values, and no laboratory abnormalities were evaluated as Achenbach’s syndrome. Patients were treated with analgesics (if necessary), mucopolysaccharidepolysulphate containing cream or gel, cold applications, and just advised to rest the diseased hand. After 2 wk of treatment, it was observed that the patients did not have any complaints.
RESULTS
In total, 24 patients were studied retrospectively. Of these, 83.33% of the patients were female (n = 20) and 16.67% were male (n = 4). The mean age was 47.91 ± 11.72. As a result, it was concluded that this syndrome was seen in middle ages and occurs in females five times more than males. None of the patients had received anticoagulation and antiplatelet treatment. The arterial and venous Doppler findings showed no pathology. Only 16.67% of the patients were smokers and none of them had a history of alcohol use. A summary of the demographic data of the patients can be found in Table 1.
In the patients’ laboratory data, the mean number of platelets was 246.95 (PLT ×103/μL), the mean international normalized ratio was 1.05, the mean prothrombin time was 11.79 min, and the mean activated partial thromboplastin time was 29.54 min. Unlike other studies, we used a pulse oximeter in the differential diagnosis of arterial ischemia or digital ischemia, and we did not observe oxygenation impairment in the pulse oximetry that would suggest ischemia in any of the patients (Table 2).
When the symptoms and the location of the syndrome were examined, all the patients had pain and bruising in the affected area. The swelling was 54.1% and the paresthesia was 37.5%. The mean number of episodes was 3.04. When the affected area and finger were considered, the most common regions were right hand (54.1%)and index finger (33.3%) (Table 3). Herein, it can be concluded that the disease is most commonly seen at the right hand index fingers of middle-aged females.
DISCUSSION
There are few publications on Achenbach’s syndrome in the literature. However, the scarcity of these publications is not due to the rareness of the disease. Our clinical observations suggest that the disease is more common than generally thought.Although a large proportion of patients were referred to cardiac surgery clinics, some were referred to other departments such as family medicine, dermatology, internal medicine, hematology, rheumatology, plastic surgery, and orthopedics, or the patients were directed to these departments from cardiac surgery clinics.
In the absence of a known essential cause, Achenbach’s syndrome is characterized by an acute pain and numbness in the fingers. In addition to these complaints,swelling and paresthesia can be observed. In our study, all the patients had complaints of pain and bruising, yet swelling and paresthesia were present in only some of them. In the literature, two cases were identified in which the location of the disease was not the fingers. One of these cases was recurrent subconjunctival hemorrhage in the eye while the other was located in the wrist[2,3].
Although the etiology of Achenbach’s syndrome is unknown, Singer has hypothesized that in some patients increased capillary resistance and vascular fragility may trigger this disease even in a minimal trauma[4]. It has also been reported that acrocyanosis, gastrointestinal diseases, migraines, and biliary diseases may be related to the etiology of the disease[5]. Kämpfen et al[6]have proposed the etiology of vasospasm through a case in which ergotamine was used due to migraine. It has been suggested that Achenbach's syndrome may be associated with Raynaud’s syndrome and Chilblain’s disease in the secondary data gathered from Carpentier et al[7]. In the same study, this syndrome was found to be associated with tobacco use, alcohol consumption, and estrogen therapy while no relationship was observed with body mass index, education level, marital status, occupation, vibration, and trauma.Achenbach’s syndrome is 2-7 times more common in middle-aged women than in men[8-10]. Although the most common location of the disease varies in the sources, it has been observed more frequently in the middle and index fingers[7]. Achenbach’s syndrome is generally episodic[11,12]. In our study, the average number of episodes was 3.04, and the most common finger was the index finger (Figures 1 and 2).
Physical examination and anamnesis have a major role in the diagnosis of Achenbach’s syndrome. Laboratory and imaging techniques may be required for differential diagnosis (Table 4). However, in suspected cases, these methods should be used and unnecessary invasive procedures should be avoided[6,13]. Because of the possibility of mistaking the syndrome with many vascular, hematologic,dermatologic, and rheumatologic diseases, some laboratory and imaging methods might be required (such as complete blood count, coagulation factors, c-reactive protein, blood lipid level, and arterial and venous Doppler ultrasonography of the concerned extremity)[8,11,14]. In the literature, biopsies were performed for lesions in two cases[8,15]. In one of these cases, the epidermis showed hyperkeratosis and parakeratosis. In the other case, amorphous, eosinophilic amyloid deposition in thestroma and fibrin accumulation was observed. In both cases, no pathology was detected in microvascular structures. Capillaroscopy examination was not necessary for diagnosis, but Khaira et al[9]performed capillaroscopy in 11 patients, and no pathology was detected. Frerix et al[16]showed capillary hemorrhage in one case.Arterial and venous Doppler ultrasonography is a good non-invasive choice for evaluating the vascular bed[17]. No arterial or venous pathology was found in the Doppler ultrasonography in any of the studies performed.

Table 1 Demographic data of patients
Upon suspicion of arterial microembolism, invasive imaging methods can be used to investigate the origin of the microemboli[18]. While in the case reported by Weinberg et al[11], no pathology was observed in the upper extremity angiography, in the case of Robertson et al[19], slow flow was observed in the digital arteries. There are studies in which transthoracic echocardiography was used in the diagnosis of arterial embolism,and no cardiogenic embolic source had been found in these studies[10,11]. In our study,oxygen saturation was measured at the diseased fingertip by pulse oximetry in order to possibly detect microemboli. No abnormal oxygen saturation, which would suggest ischemia or embolism, was found in any of the patients. Achenbach’s syndrome should be considered in the differential diagnosis of symptoms similar to Raynaud’s syndrome with clinical episodic digital ischemia[20]. The rheumatologic aspect of the syndrome has been further investigated in case reports, but no rheumatologic relationship has been found other than Achenbach’s syndrome associated with rheumatoid arthritis reported by Manappallil et al[8,21,22].
Nowadays, many patients now refer to hospitals by searching their symptoms from the internet, from written and visual media, and from social media. This situation forces physicians not only to diagnose and treat, but also to help reduce the anxiety caused by incorrect or incomplete information. Patients with Achenbach’s syndrome who refer to the clinics are in urgent expectation thinking that there is a blockage of the blood vessels or a blood clot in the finger. For this reason, the unwarranted concerns of the patients should be eliminated properly. There are many different opinions in the general treatment of the disease. Some of these views suggest that there is no need for treatment because of the benign course of the disease and that only follow-up is sufficient[10,23,24]. On the other hand, there are publications in which treatment includes sargegrelate hydrochloride, acetylsalicylic acid 81 mg, long-acting diprimadol, heparin, or isosorbidedinitrate[8,11,19]. Though the etiology was unknown, if a bleeding point was definite, we did not apply anticoagulant, antiplatelet, or vasodilator treatments unless there was another compulsory indication. When necessary, patients were treated with analgesics, or with cream or gel containing mucopolysaccharidepolysulphate; occasionally cold applications were applied or the patient was advised to rest the diseased hand. After 2 wk of treatment, it was observed that the patients did not have any complaints.
Today we know very little about this syndrome. Further studies on the disease is important because we know that the disease is on the fingers, the palmar surface, the ankle, and the eye, but we do not know whether the brain and other vital organs have the same bleeding and hematoma[7]. Due to Achenbach’s syndrome, a probable hemorrhage or hematoma in the brain and other vital organs would be lifethreatening, so the disease should be further investigated.

Table 2 Laboratory data of patients
In conclusion, there is no doubt that many new studies will be done as the awareness of Achenbach’s syndrome increases. The etiology and prognosis of the disease is still a mystery. It is of great importance to know whether the syndrome is seen in the brain and vital organs. However, it is relieving to know that there is no proven mortality or morbidity of the disease and that the course of the disease is benign.
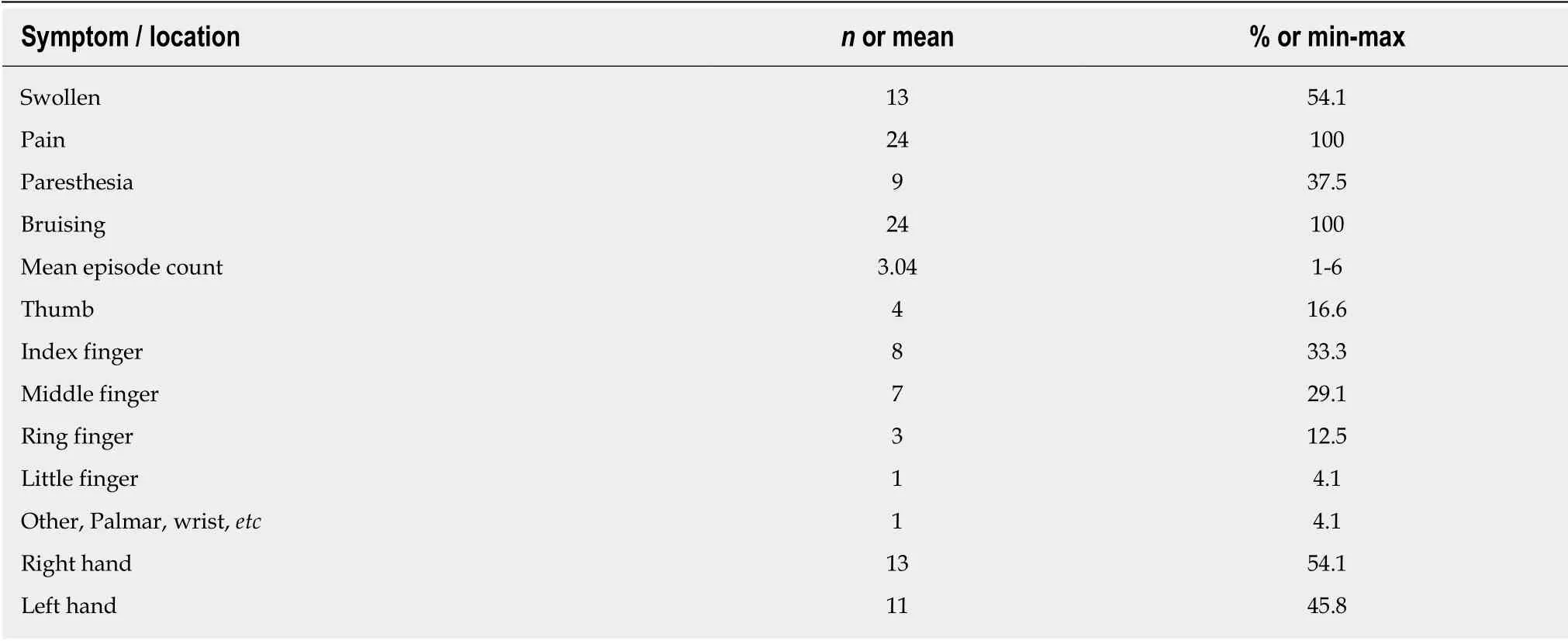
Table 3 Achenbach’s syndrome symptoms and location features
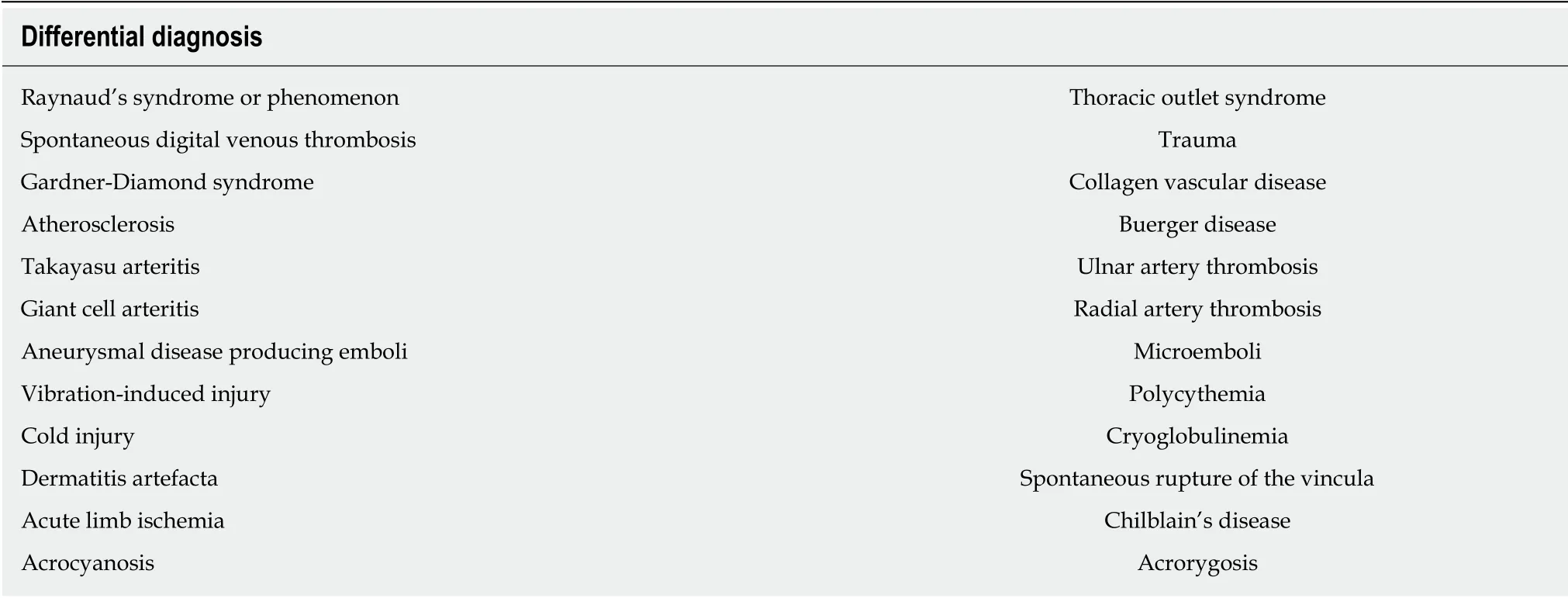
Table 4 Differential diagnoses

Figure 1 The bruising is located on the right hand ring finger.

Figure 2 The bruising is located on the right hand index finger.
ARTICLE HIGHLIGHTS

 World Journal of Clinical Cases2019年10期
World Journal of Clinical Cases2019年10期
- World Journal of Clinical Cases的其它文章
- Impact of perioperative transfusion in patients undergoing resection of colorectal cancer liver metastases: A population-based study
- Risk factors and clinical responses of pneumonia patients with colistin-resistant Acinetobacter baumanniicalcoaceticus
- Diagnostic value of two dimensional shear wave elastography combined with texture analysis in early liver fibrosis
- Selective dorsal rhizotomy in cerebral palsy spasticity - a newly established operative technique in Slovenia:A case report and review of literature
- Invasive myxopapillary ependymoma of the lumbar spine: A case report
- Electrohydraulic lithotripsy and rendezvous nasal endoscopic cholangiography for common bile duct stone:A case report
