Comparison of endothelial cell changes by specular microscopy between Ringer’s and Ringer’s lactate during phacoemulsification
Abstract
INTRODUCTION
Cataract extraction is now a common surgical procedure performed daily in most ophthalmic surgical theaters. Endothelial cell loss to a mild or a moderate percent is inevitable after the cataract surgery[1-4]. At first, salt solution, Ringer’s solution, and plasmalyte 148 were used for cataract surgery as irrigating solutions[5-6]. After that, a more physiological solution, named balanced salt solution (BSS) was developed. BSS has an unique chemical composition, as it contains the magnesium element which is necessary for the Mg-ATPase endothelial pump and the acetate citrate buffering system together with potassium and calcium (Table 1).
Table1Chemicalcompositionofdifferentirrigatingsolutions

ParametersHumanaqueoushumorRingersRingerslactateBSSBSSplusSodium(mEq/L)162.9147.5131155.7160Potassium(mEq/L)2.2-3.94510.15Calcium(mEq/L)1.84.523.31Magnesium(mEq/L)1.1--1.51Chloride(mEq/L)131.6156111128.9130Bicarbonate(mEq/L)20.15---25Phosphate(mEq/L)0.62---3Lactate(mEq/L)2.5-29--Glucose(mEq/L)2.7-3.7---5Ascorbate(mEq/L)1.06----Citrate(mEq/L)---5.8-Acetate(mEq/L)---28.6-Glutathione(mEq/L)----0.3PH7.386.0-7.26.0-7.27.67.4Osmolality(mOsm/L)304310278298305
BSS: Balanced saline solution.
The BSS has PH more than 7 and shows little hypotonicity to the aqueous[7-8]. Later in the seventies, BSS plus which is considered a newer generation of irrigating solutions was developed[5-6]. The new irrigating solution has bicarbonate, glucose and glutathione added to the original BSS which helps maintaining the function of the endothelial cells. BSS Plus ionic composition is closely similar to that of the aqueous fluid[8].
Despite the superiority of BSS and BSS plus, their widespread usage has always been limited by relatively higher cost, especially in regions with limited resources. This limitation has made cheaper solutions like Ringer’s and Ringer’s lactate (RL) more widely used as irrigating fluids in cataract surgeries in certain regions[8]. Ringer’s solution contains calcium chloride, potassium chloride, sodium chloride, and sodium bicarbonate which help in balancing the PH. Ringer’s lactate contains potassium, calcium, and lactate ions, which maintain corneal endothelial cells for long periods (Table 1). Calcium is necessary for the protection of the function of the endothelial cells. Ringer’s lactate shows hypotonicity and has PH slightly less than 7. The osmolality of BSS, aqueous, and Ringer’s lactate is 302, 302, and 280 mOsmol/L respectively. The PH of BSS, aqueous, and Ringer’s lactate is 7.4, 7.4, and 6.0 respectively[9].
In everyday practice Ringer’s and RL solutions are used interchangeably in cataract surgery. There are few studies reporting the difference in using either of these solutions during phacoemulsification to be able to draw a conclusion if one of them is more superior than the older. The current study aimed at investigating whether there was a significant difference between using Ringer’s and RL solutions when used as irrigating solutions during phacoemulsification and their effect on corneal endothelium.
SUBJECTS AND METHODS
This was a prospective randomized interventional double blinded clinical study that included 100 eyes of 100 patients aged between 50 to 65 years suffering from a visually significant age-related cataract and scheduled for routine uncomplicated phacoemulsification with implantation of a hydrophobic acrylic intraocular lens (IOL) in the capsular bag. The study adhered to CONSORT guidelines. Patients were excluded from the study if they had coexisting corneal pathologies, uveitis, dense brown cataract, glaucoma, diabetes, previous ocular surgery, any intraoperative complication or excessive manipulations affecting corneal endothelial integrity, and preoperative endothelial cell count less than 1500 cells/mm3. Included eyes had lenticular changes with nuclear cataract of grade 2-3 according to lens opacities classification system III (LOCS III)[10-11]in which cataract severity was evaluated using slit lamp by a single examiner.
The included eyes were randomly divided into two equal groups (each group included 50 eyes). Group 1 received Ringer’s solution and group 2 received Ringer’s lactate as an irrigating solution during phacoemulsification. The randomization method was by coin flipping and was done before any examination or investigations. This research was approved by the Local Ethics Committee of Faculty of Medicine, Alexandria University, Egypt. The tenets of declaration of Helsinki were followed. All patients signed an informed consent at the time of inclusion before any intervention.
All patients were subjected to complete preoperative ophthalmic examination including: uncorrected and best corrected visual acuity, manifest refraction, slit lamp examination with careful examination of the cornea to exclude the presence of any corneal pathology, lens opacity grading using LOCS III classification[10-11], measuring the intraocular pressure, and detailed fundus examination under pupillary dilatation.
Table2ComparisonofsurgicaldatabetweenstudygroupsMean±SD
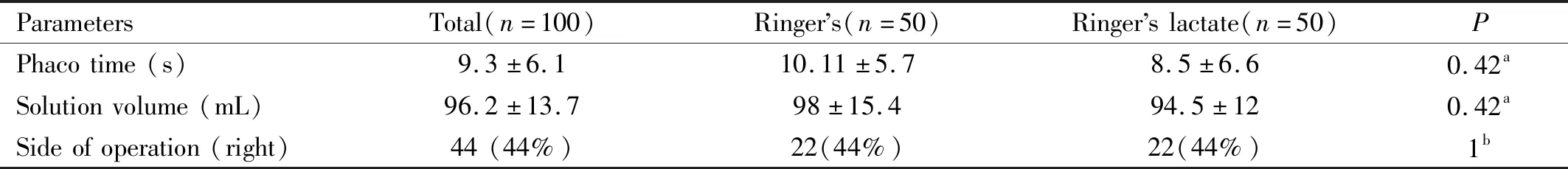
ParametersTotal(n=100)Ringers(n=50)Ringerslactate(n=50)PPhacotime(s)9.3±6.110.11±5.78.5±6.60.42aSolutionvolume(mL)96.2±13.798±15.494.5±120.42aSideofoperation(right)44(44%)22(44%)22(44%)1b
aIndependent-samplet-test;bChi-square test.
Central corneal thickness (CCT) was assessed by ultrasonic pachymetry (Ocuscan, Alcon, Texas, USA). The patient looked at a fixation target while the ultrasound probe was placed perpendicular to the central cornea without applying any excessive pressure. An average of three good quality readings was taken. Corneal endothelium was examined by using noncontact specular microscopy (Tomey EM-3000, Tomey Corporation, Nagoya, Japan). Three good quality measurements were done for the eye, and the mean of measurements was calculated. The patient was asked fix on a light source and the operator aligned the image of the patient’s eye using a joystick. Then, the instrument acquired automatic measurements. The variables that were measured in all cases included: average size of endothelial cells(in μm2), coefficient of variation of size (CV), polymegathism which is a measurement of the variability of the cell size, standard deviation of size (SD) (in μm2), endothelial cell density (ECD) (in cells/mm2), and hexagonality (%). All cases were measured by a single operator. Each patient was examined twice, before surgery and three months postoperative.
SurgicalTechniquePreoperative medications included topical administration of a 4thgeneration fluoroquinolone antibiotic. Moxifloxacin 0.3% (Vigamox, Alcon) and non-steroidal anti-inflammatory drug (NSAID), nepafenac 0.1% (Nevanac, Alcon) 4 times for 2d before surgery. Pupillary dilatation was started 2h before the scheduled time for the surgery using 1% tropicamide and 1% cyclopentolate eye drops instilled every 15min.
A single surgeon (Abou Samra A) performed all surgeries under topical anesthesia using xylocaine 4% with intravenous sedation using a reproducible surgical technique. A 2.4 mm two-plane superior clear corneal incision was made with a metal blade. Viscoat© (Alcon Laboratories S.A, Ltd) was injected to maintain the depth of the anterior chamber and to coat the corneal endothelium. The nucleus was emulsified with INFINITI© System (Alcon Laboratories Inc., Fort Worth, Texas, USA), with Ozil-compatible hand piece and Kelman-style 45° phacoemulsification tip using the four-quadrant divide and conquer technique. The following parameters were used: a phacoemulsification power of 0-30%, a vacuum of 90-400 mmHg, and an aspiration flow rate of 25-85 mL/min. The bottle height was raised to a 110 cm during the fragment removal. Then a foldable hydrophobic acrylic (Acrysof, Alcon Inc., Fort Worth, Texas, USA) IOL was implanted inside the bag.
Any intraoperative elongation of the operation time (average surgery takes 5-10min at maximum), incisional burns, or any complicated cases was excluded from the study. The following intraoperative data were recorded: the volume of irrigation fluid used, surgical clock time, and effective phaco time (average ultrasound power multiplied by average ultrasound time and divided by 100).
After the operation, topical Moxifloxacin 0.3% (Vigamox, Alcon) and steroids eye drops, prednisolone acetate 1% (Econopred plus, Alcon) were prescribed 4-5 times daily for 4wk. In addition, Dexamethasone and Tobramycin ointment (Tobradex, Alcon) was prescribed at bedtime for 2-3wk. Postoperatively, the patient was examined on 1d, 1wk, 1mo, and 3mo. At each follow-up visit, special attention was taken to the presence of abnormalities in cornea clarity, Descemet’s folds, and/ or intrastromal or epithelial edema. Pachymetry and Specular microscope were done 3mo postoperatively.
Data analysis was performed using the software SPSS for Windows version 20.0 (SPSS Inc., Chicago, USA). Quantitative data were described using range, mean and standard deviation. Normality of data samples was evaluated using the Kolmogorov-Smirnov test. Studentt-tests (independent samplet-test and pairedt-test) were used for comparisons between different means. Chi-square test was used to compare between different percentages. Pearson Correlation coefficient was used to assess the correlation between different variables. Differences were considered statistically significant when the associatedPwas less than 0.05.
RESULTS
The study included 100 eyes of 100 patients divided equally into two groups. The first group with Ringer’s solution had a mean age of 57.5±8 years and the second group with RL solution had a mean age of 58.6±9 years. There was no statistically significant difference between the two groups (P=0.57). The percentage of females was 70% and 68% in group 1 and group 2 respectively. Also, there was no statistically significant difference between both groups as regarding nuclear grading of the cataract density according to LOCS III classification.
Table 2 shows the comparison of surgical data between the study groups. The mean effective phaco time and the mean irrigating solution volume levels were lower in Ringer’s lactate group but this difference was statistically insignificant. The mean effective phaco time was 10.11±5.7s and 8.5±6.6s in Ringer’s and RL groups respectively (P=0.42). The mean volume of irrigating solution used was 98±15.4 mL and 94.5±12 mL in groups 1 and 2 respectively (P=0.42). In both groups, 22 eyes were on the right side.
Table3Comparisonofpreoperativepachymetryandspecularmicroscopicmeasurementsbetweenstudygroupsmean+SD

ParametersTotalRingersRingerslactatePECD(cells/mm2)2521±2562390±247.82652±215.90.001aCV(%)36.5±6.237.7±4.635.3±7.30.213SD(μm2)146.9±35.3158.55±33.1135.25±34.30.035aHexagonality(%)47.5±11.142.65±7.852.35±11.90.004aAVG(μm2)400.5±48418.8±51.9382.2±37.60.014aCCT(μm)513.1±42.8505.3±48.9520.9±35.10.254Polymegathism(%)25.57±4.924.88±4.526.36±5.40.43
ECD: Endothelial cell density; CV: Coefficient of variation; SD: Standard deviation; CCT: Central corneal thickness; AVG: Average cell size;aStatistically significant.
Table4Comparisonof3mopostoperativepachymetryandspecularmicroscopicmeasurementsbetweenstudygroupsmean+SD
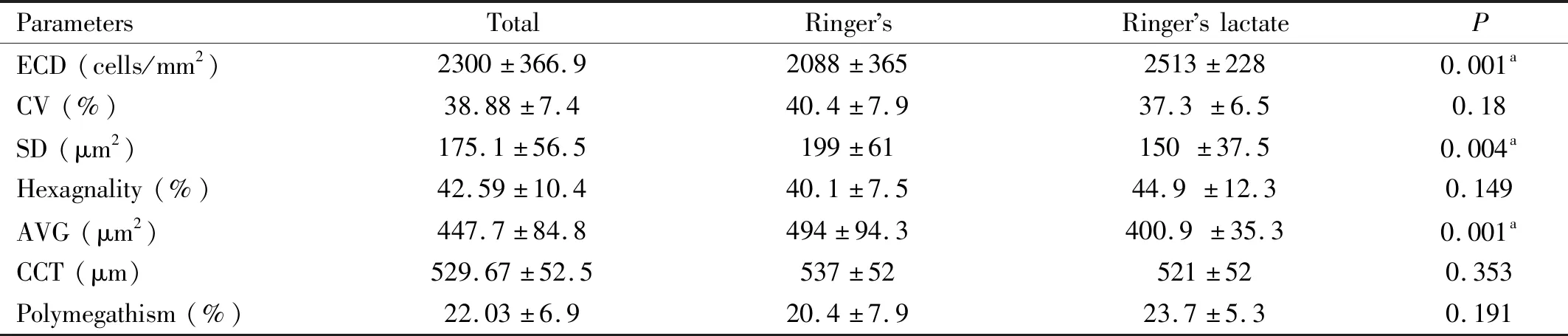
ParametersTotalRingersRingerslactatePECD(cells/mm2)2300±366.92088±3652513±2280.001aCV(%)38.88±7.440.4±7.937.3±6.50.18SD(μm2)175.1±56.5199±61150±37.50.004aHexagnality(%)42.59±10.440.1±7.544.9±12.30.149AVG(μm2)447.7±84.8494±94.3400.9±35.30.001aCCT(μm)529.67±52.5537±52521±520.353Polymegathism(%)22.03±6.920.4±7.923.7±5.30.191
ECD: Endothelial cell density; CV: Coefficient of variation; SD: Standard deviation; CCT: Central corneal thickness; AVG: Average cell size.astatistically significant.
Table5Comparisonofpercentageofchangeinpostoperativepachymetryandspecularmicroscopicmeasurementsbetweenstudygroups(dataarepresentedasmeanandinterquartilerange)
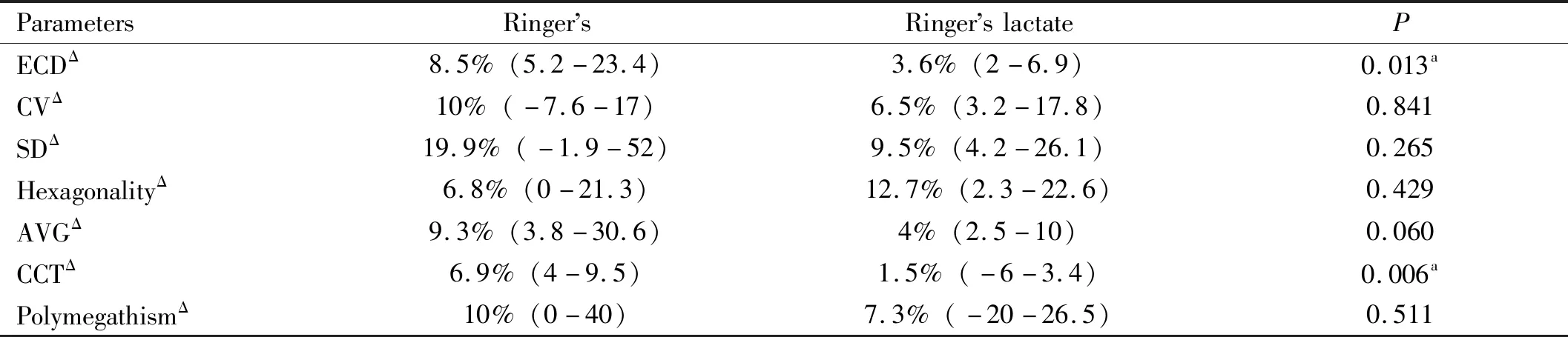
ParametersRingersRingerslactatePECDΔ8.5%(5.2-23.4)3.6%(2-6.9)0.013aCVΔ10%(-7.6-17)6.5%(3.2-17.8)0.841SDΔ19.9%(-1.9-52)9.5%(4.2-26.1)0.265HexagonalityΔ6.8%(0-21.3)12.7%(2.3-22.6)0.429AVGΔ9.3%(3.8-30.6)4%(2.5-10)0.060CCTΔ6.9%(4-9.5)1.5%(-6-3.4)0.006aPolymegathismΔ10%(0-40)7.3%(-20-26.5)0.511
Δ: Degree of change; ECD: Endothelial cell density; CV: Coefficient of variation; SD: Standard deviation; CCT: Central corneal thickness; AVG: Average cell size.aStatistically significant.
Table 3 shows the Specular microscopic data collected preoperatively which revealed significant differences in some parameters. Mean central ECD in group 1 was 2390±247.8 cells/mm2, whereas the mean value in group 2 was 2652±215.9 cells/mm2(P=0.001). Mean SD in group 1 was 158.55±33.1, and in group 2 was 135.25±34.3 (P=0.035). Mean hexagonality in group 1 was 42.65±7.8, and in group 2 was 52.35±11.9 (P=0.004). Mean average cell size in group 1 was 418.8±51.9, and in group 2 was 382.2±37.6 (P=0.014).
Some of the specular microscopic data showed statistically significant difference 3mo postoperatively between the two groups (Table 4). Mean central ECD in group 1 was 2088±365 cells/mm2whereas the mean value in group 2 was 2513±228 cells/mm2(P=0.001). Mean±SD in group 1 was 199±61, and in group 2 was 150±37.5 (P=0.004). Mean average cell size in group 1 was 494±94.3, and in group 2 was 400.9±35.3 (P=0.001).
Table 5 demonstrates a comparison between Ringer’s group and Ringer’s lactate group regarding the postoperative changes in specular microscopic measurements. The differences in the degree of changes of CV, SD, hexagonality, average cell size and polymegathism between groups were not found to be statistically significant. However, there was a statistically significant difference in the following parameters.
ECD decreased in group 1 by a mean of 8.5%, and in group 2 by a mean of 3.6% (P=0.013); CCT increased in group 1 by a mean of 6.9% and in group 2 by a mean of 1.5% (P=0.006). By correlating the percentage of change in pachymetry and specular microscopic parameters with age, some parameters had significant correlation:ΔECD (r=0.406,P=0.009),ΔCV (r=0.496,P=0.001), andΔSD (r=0.473,P=0.002). By correlating the percentage of change in pachymetry and specular microscopic parameters with effective phaco time, some parameters had significant correlation:ΔECD (r=-0.378,P=0.016) andΔaverage cell size (r=0.324,P=0.041). By correlating the percentage of change in pachymetry and specular microscopic parameters with volume of irrigation solution used, there was no significant correlation.
DISCUSSION
Phacoemulsification cataract surgery, the most commonly performed surgery in ophthalmology, has always been associated with damage to the corneal endothelium[12]. ECD decreases at a higher rate after cataract surgery than it does in healthy corneas with no previous operations[13].
Previous studies have shown that the optimum irrigation solution that protects the corneal endothelial cell function needs to have a similar composition to the aqueous humor, beside adding an antioxidant[5]. There are few studies investigating the difference in using either of Ringer’s or Ringer’s lactate solutions during phacoemulsification to be able to draw conclusions if one is more superior. Up to our knowledge only a single study has reported comparable results for Ringer’s and Ringer’s lactate solutions[9].
As this study was a randomized clinical study, we did not determine the sex of the included patients before surgery, but females outnumbered males in this study (around 70% of patients). The higher prevalence of cataract in females has been noted in other studies that also report that cataract-related blindness is more common in females[14].
It was previously documented in literature that central endothelial cell density decreases throughout life at an average rate of about 0.6% per year[15]. Specular microscopy had demonstrated a gradual decrease in ECD with age, accompanied by an increased CV and a decreased proportion of hexagonal cells[16]. In our study cohort, this fact was confirmed by correlating specular microscopic changes with patient’s age, advancing age was noted to significantly correlate with the degree of corneal endothelial cell loss as it was observed that there is a significant decrease in ECD as age advances (r=0.406,P=0.009). This pinpoints the importance of matching age between study groups to exclude it as a confounding factor for any changes in the pattern of post-operative endothelial cell loss in either of the two groups. Diabetes is known to affect tissue healing and regeneration. It has been found to exaggerate the degree of cell loss after cataract surgery[17]. Therefore, cases suffering from diabetes were excluded.
According to the results of our study, there was significant correlation between degree of loss in endothelial cells and the effective phaco time (P=0.016). The comparable phaco time used in both groups was essential to eliminate any bias in the results when comparing the two groups. The amount of solutions used was nearly equal for both groups (98±15.4 mL and 94.5±12 mL in groups 1 and 2 respectively). There was no correlation between the volume of irrigating fluids used and changes in endothelial parameters. In a previous study that compared between RL and BSS plus[7]according to the endothelial cell density reduction in relation to phaco time and irrigation volume, there was no significant correlation with phaco time and irrigation volume used and endothelial cell density reduction. This is consistent with findings of the present study that found no significant correlation between irrigation volume and corneal endothelial attrition. Our findings vary, however, from the previously cited study in relation to phaco time effect on ECL, which may be due to various factors such as different surgical technique, incision type and location, and cataract density.
The current study included uncomplicated cases performed by an experienced surgeon (Abou Samra A) who performed all surgeries with less than 27s of phacoemulsification time (phacoemulsification power range from 0 to 30%) and with less than 120 mL for all surgeries and there was no intraoperative or postoperative complications such as Descemet’s membrane detachment, iris trauma, posterior capsule rupture or endophthalmitis during the study.
The change in CCT in microns was calculated by noting the difference between CCT at 3mo follow-up visit and the preoperative CCT. Kohlhaasetal[18]reported no further postoperative loss of endothelial cell after four weeks, which suggests that wound healing is complete by this time. This postulate accords well with the findings of Chengetal[19]and Amonetal[20]who also observed preoperative corneal thickness values to be restored within a similar period of time.
Comparison of baseline specular microscopic measurements between study groups revealed statistically significant differences between the 2 study groups as regards ECD, SD, hexagonality and average cell size. This means that group 1 patients had significantly inferior baseline mean measurements of endothelial cell count and density. This finding might be one of the limitations of the study. It is not entirely known whether a worse baseline state of corneal endothelial integrity is considered a risk factor for more attrition post cataract surgery if other contributing factors (namely fluid volume, phaco time, comorbidities, age and type of irrigating solution) were controlled. The differences between the study group in ECD and AVG persisted postoperatively. However, the difference in hexagonality between study groups postoperatively became statistically insignificant (P=0.149). During the study we noted that measuring hexagonality was usually tedious and the machine readings were considerably inconsistent which limits the reliability of this specific measurement and bars us from drawing firm conclusion about the changes in this parameter.
In the current study, the mean decrease in postoperative ECD with Ringer’s solution was 8.5%vs3.6% with RL solution (P=0.013). Cellular loss is associated with increased polymegathism as adjacent non-dividing cells that migrate and enlarge to fill the void, polymegathism then normalizes as sizes equalize with time. ECD and CCT changes were significantly higher in the Ringer’s group. Consequently, it can be concluded that Ringer’s lactate had some degree of protection to the cornea against postoperative edema. The explanation to this finding may be related to the fact that Ringer’s lactate solution is hypotonic and slightly acidic when compared with Ringer’s solution[21]. Standardization of the surgical technique by a single experienced surgeon eliminated mechanically induced trauma as a cause for endothelial damage. The similarity in the distribution of type and grade of nuclear sclerosis eliminated energy dissipation as a cause for increased corneal thickness. Indeed, Table 3 shows the preoperative data showing significantly different measurements in some items. This led to a significant difference in the postoperative finding as expected (Table 4). However, Table 5 shows the comparison of the percentage of changes regardless of the absolute number. This overcame the bias resulting from unmatched preoperative parameters.
Kissetal[22]and Puckettetal[23]reported a similar results with the preservation of endothelial cells with the use of balanced saline solution Plus or RL as an irrigation solution used in uneventful phacoemulsification and extracapsular surgery, respectively. Joussenetal[24]reported that using BSS Plus as an irrigation solution during phacoemulsification surgery resulted in less swollen corneas on 1d postoperative in comparison with corneas irrigated with RL solution. Vasavadaetal[8]also reported the same finding. Nayaketal[25]compared the effect of phacoemulsification on the corneal endothelium using BSS Plus and Ringer’s lactate as irrigating solutions. Primary outcome was ECD at up to 6mo postoperative. The percentage of endothelial cell loss was not significantly different at 1wk, 1mo, or 6mo postoperative.
Up to our knowledge, there was only one study in the literature that compared Ringer’s to Ringer’s lactate as irrigating solutions during phacoemulsification surgery[9]. This study found a trend with Ringer’s lactate to cause less postoperative ECL and edema but this did not reach the degree of statistical significance. In our study, the potential protective effect of using Ringer’s lactate on ECL is partly confounded by the poorer baseline status of the patients in the Ringer’s group. The evidence from the two groups is thus not robust enough to build solid conclusions. Further studies are required to investigate this important point.
Regarding the effect on postoperative CCT, the strong findings from the current study of the milder impact of Ringer’s lactate together with the suggestion of this effects from data from the previously cited study[9]makes it possible to draw firmer conclusion about such a protective role. However, it should be mentioned that CCT is not independent, as ECD loss increases, the corneal edema increases and that lead to increase CCT.
In conclusion, Ringer’s and Ringer’s lactate solutions are associated with notable changes in corneal ECD, morphology, and function during uncomplicated phacoemulsification in patients with normal endothelial cell counts. The use of Ringer’s lactate as an irrigating solution is associated with less ECL postoperatively in comparison to Ringer’s solution and associated with decreased postoperative edema.