糖尿病合并视网膜脱离术后高眼压的处理及危险因素探讨
石 蕊,谢安明,李 迪,车选义,Rechard Hom
(作者单位:1710068中国陕西省西安市,陕西省人民医院眼科;2710061中国陕西省西安市,西安交通大学第一附属医院眼科;317601美国宾夕法尼亚州萨鲁斯大学生物药剂系)
INTRODUCTION
P ersistent elevated intraocular pressure(IOP)has been implicated in optic nerve damage and irreversible vision loss[1],and is a common complication of vitrectomy with silicon oil tamponade for rhegmatogenous retinal detachment(RRD)[2-3],especially in patients with diabetes,who is regarded to be high risk population of primary open angle glaucoma(POAG).Axial elongation of the globe,seen in high myopia,can also cause retina degeneration,vitreous detachment and anterior chamber angle structural abnormality.Individuals with high myopia were historically the most susceptible population for RRD and POAG[4-6].Pars plana vitrectomy(PPV)with silicon oil(SO)tamponade has proven to be an effective management strategy for different posterior segment conditions including macular hole,epiretinal membrane,vitreous hemorrhage and retinal detachment[7-10].Few studies,however,have focused solely on high myopia and its risk for IOP elevation after vitrectomy in diabetic patients.
The present study seeks to identify the prevalence and the risks of transient IOP elevation during the early postoperative period for repair of RRD in high myopia patients with diabetes.Also,the risk increasing with glucocorticoid eye drop use during the postoperative period and when there was pre-existing POAG.Lastly,damage to the optic nerve head and any decrease in RNFL thickness after transient IOP elevation will also be observed to establish a rationale for managing transient IOP elevation after vitrectomy.
SUBJECTS AND METHODS
ParticipantsThe prospective study recruited one hundred diabetic patients between October 01,2016 and June 30,2017 from the Department of Ophthalmology of the First Affiliated Hospital of Xi'an Jiaotong University.All recruited patients were diagnosed as type 1 or 2 diabetes for at least 1y and received a comprehensive ophthalmic examination by staff ophthalmologists,consisting of best corrected visual acuity,IOP measurements,refractive error,slit-lamp examination,gonioscopy,and axial length by IOL Master.In addition,digital fundusphotograph and retinalnerve fiberlayer(RNFL)thickness of the unoperated eyes were collected before PPV surgery.After surgery,the same measures were performed just on the operated eyes until 3thday of surgery.All operated eyes were examined and followed until the silicone oil(SO)was removed for optimal surgical outcome and patient safety.
The inclusion criteria were adults from 40 to 65 years who had high myopia with RRD and were further defined with the following parameters:1) high myopia as defined by a spherical equivalent(SE)of≥-6.00 D or an axial length(AL) ≥26.0 mm;2)PPV as the primary surgery for RRD treatment;3)The use of SO(FCI,S5.7560)during vitreous tamponade for their PPV; 4) No proliferative vitreoretinopathy(PVR).Only the operated eyes in each patient were fully evaluated throughout the study.
All patients in both the control and experimental groups willingly consented in writing for inclusion in the study.The study also adhered to the tenets of the Declaration of Helsinki and to the common principles of an Institution Review Board of minimal risk.There were no experimental procedures or medications used and there was a minimal probability of harm or discomfort to patients as would be encountered in daily life or during the performance of routine physical examination and tests.
Exclusion CriteriaSubjects were excluded if there were:1)current or past glaucoma or uveitis of any kind;2)any damage in the anterior chamber or the presence of new vessels in the anterior chamber as detected by conventional gonioscopy;3)detachment of the ciliary body;4)current or history of prior ocular trauma;5)any intrusion of SO into the anterior chamber;6)SO emulsion;7)PPV in conjunction with any other ocular surgery.Also,patients could not be a participant in any other study concurrently.
Surgical TechniqueAll patients with planned PPV surgery for RRD with high myopia were operated on by the same experienced retinal surgeon at the Department of Ophthalmology of the First Affiliated Hospital of Xi'an Jiaotong University.Three days prior to surgery,each operative patient received topical levofloxacin eye drops in the planned operated eye to minimize ocular infection.Pars plana vitrectomy in all eyes was performed by the same surgeon with ConstellationVitrectomy System.A 23-gauge,3-port PPV,with a complete vitrectomy was carried out on all the patients to relieve the vitreous traction around the retinal breaks.A complete posterior vitreous detachment was induced whenever one was not already presentpreceding the completion ofvitrectomy surgical procedure.An air-fluid exchange with internal drainage of subretinal fluid was then performed and 4-9 mL of SO(Franc,S5.7560,5000cSt,10 mL) was instilled to displace air at the end of the surgery according to the volume of the vitreous.Consequently,the eyes were kept slightly hypotonic.
Postoperative Management and GroupingPatients were divided into two groups:one group received a combination antibiotic/steroid drop(Tobramycin/Dexamethasone)and an antibiotic drop,levofloxacin,after PPV and SO tamponade;the other group received just levofloxacin eye drops.Both groups received all their drops six times per for the first week.At the end of the first week and until the 30thday,both groups received just the levofloxacin eye drops.There were 53 eyes in the experimental group and 47 eyes in the control group.All operated eyes were followed for six months until all SO was removed.
Intraocular Pressure MeasurementThe IOP of all study participants were measured similarly with the Tomey FT1000 Non-Contact Tonometer,at 1d,5d,1wk,2wk and 1mo after surgery.Before each use,the tonometer was calibrated in accordance to the user's manual and only measurements<5%error was used.The IOP measurements were repeated three times,and the mean value of the three was used for data analysis.IOP >25 mmHg or increasing 5 mmHg on the basis IOP was set as the threshold for clinically significant elevated IOP.When any eye had an IOP between 25-40 mmHg,medications were initiated to reduce the IOP.If any eye experienced and an elevation of IOP greater than 40 mmHg during the postoperative period,then an anterior chamber paracentesis was employed and monitored to forestall hypotony.Following antiglaucoma surgery,IOP levels were recorded until stabilized.
OpticalCoherenceTomographyMeasurementAcquisition of spectral domain optical tomographic(SDOCT)images with the Topcon 3D OCT-1 Maestro Imaging System(ver.8.30)followed a standardized protocol both before and after surgery.Automatic alignment,focusing and capture of images ensured point-to-point matching of follow up scans.The peripapillary RNFL thickness,the optic nerve cup/dis(C/D)ratios and cup volumes were evaluated with three-dimension(3 D)scans(6.0×0.6 mm,512×128)proceeding pupillary dilation of all eyes before surgery and the operated eyes after surgery.RNFL thickness of the operated eyes was also measured on the third and the day when IOP decreased to normal and became stable immediately after surgery.Only clear,focused and well-centered images with no eye movements and“quality strength”of 25 or more were selected for further analysis.The total,superior,inferior,nasal and temporal RNFL thicknesses,C/D area ratios and optic cup volumes were calculated by the instrument's software and then subjected to analysis.Patients with retinal edema after vitrectomy were excluded from the final analysis.
Statistical AnalysisStatistical analysis was performed with Prism GraphPad Version 7.01.Mean and standard deviations of IOP and other parameters were calculated.Independent-Samples t-test was used to compare the difference between groups.Cases with elevated IOPs were examined with Chisquare“goodnessoffit” testwhereONH parameters comparison was made with Paired t-test.
RESULTS
This prospective study included 100 eyes of 100 high myopia patients with a mean age of 55.42±13.24 years and mean AL of 27.37±1.42 mm(Table 1).The mean preoperative IOPwas 18.31±5.43 mmHg,but IOP increased significantly at the first week(t=3.595,P=0.000),when IOP ranged from 10 to 62 mmHg(mean IOP:28.12±16.38 mmHg),and the end of the first month after vitrectomy(t=2.497,P=0.014).There were 42 patients who exhibited an IOP elevation during the follow-up time.A total of 42 eyes had an IOP elevation during the first week,with 39 eyes steadily increasing after the first week and was successfully managed by IOP lowering medications or even paracentesis. Finally, three eyes underwent glaucoma filtration surgery because of refractive elevated IOP levels.
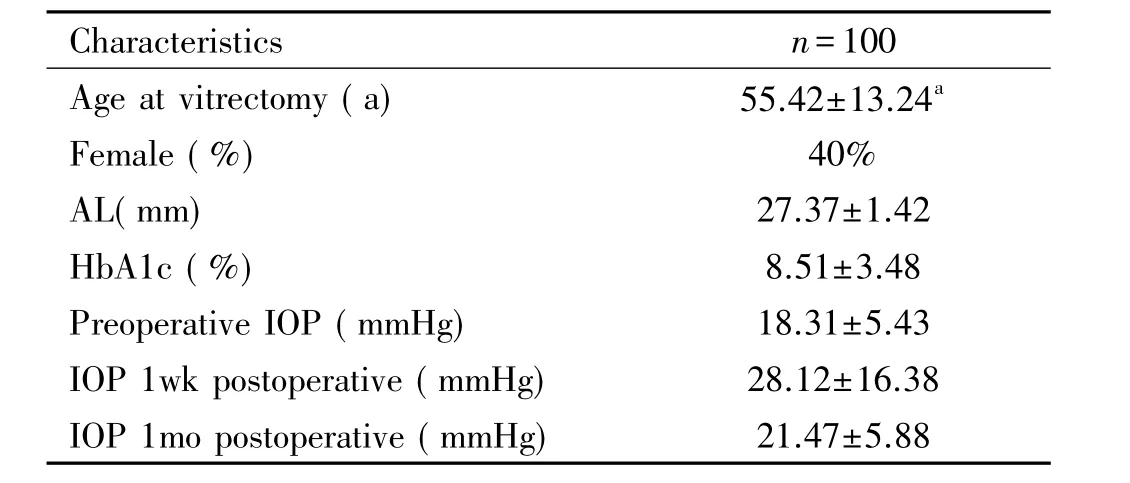
Table 1 Base line characteristics of the study participants
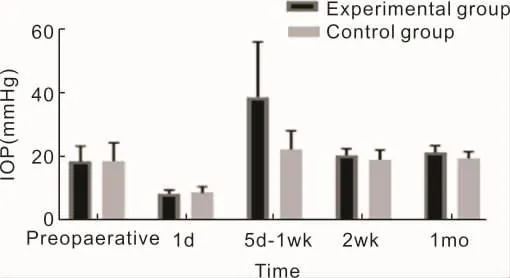
Figure 1 Optical coherence tomography measurement.
A statistically significantdifference was found in the occurrences ofIOP elevation between the two groups,especially 5-7d(1wk)after vitrectomy(χ2=12.588,P=0.000) (Table 2).The mean IOP was higher in the experimental group than in the control group in the first week after operation(t=3.284,P=0.002).At the end of the first month,the IOP in the experimental group remained higher than the control group(t=2.402,P=0.021)(Table 3,Figure 1).
RNFL thickness and ONH parameters were measured on the third day after PPV with silicon oil tamponade by OCT.However,11 eyes were excluded because of significant retina edema,which could influence the data analysis.In all,it was observed that 31 eyes had IOP elevation and keep on about one week,the average,superior and inferior RNFL layer were thinner,rim area was smaller,cup volume and vertical C/D radio was significant bigger after surgery(Table 4).
RNFL thickness and ONH parameters of the opposite eye were measured in all the participants and were compared between IOP elevation patients and the ones had no IOP increased afteroperation.The data shown that the average and inferior quadrant in patients with high IOP were thinner than other people(Table 5).
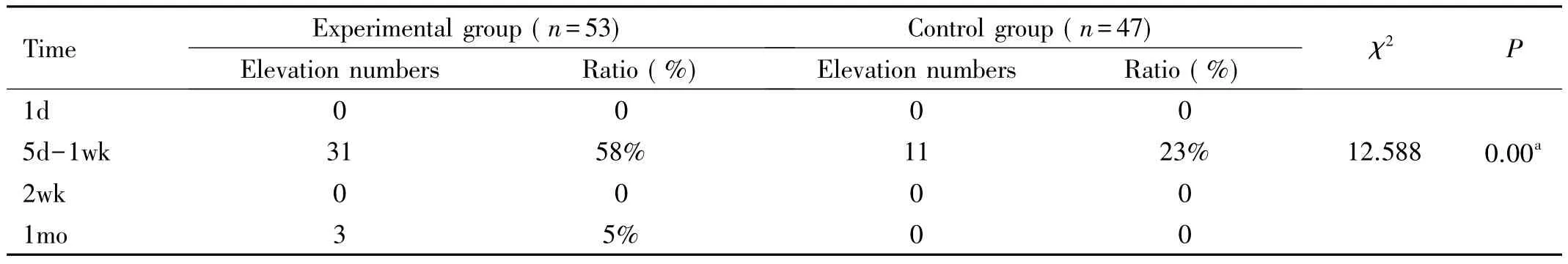
Table 2 Numbers of patients with elevated IOP postoperative
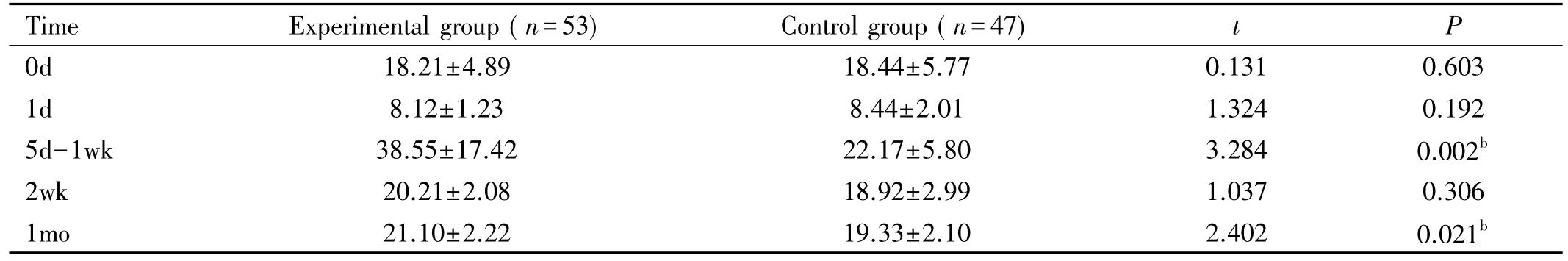
Table 3 Preoperative and postoperative IOPs between groups(mmHg)
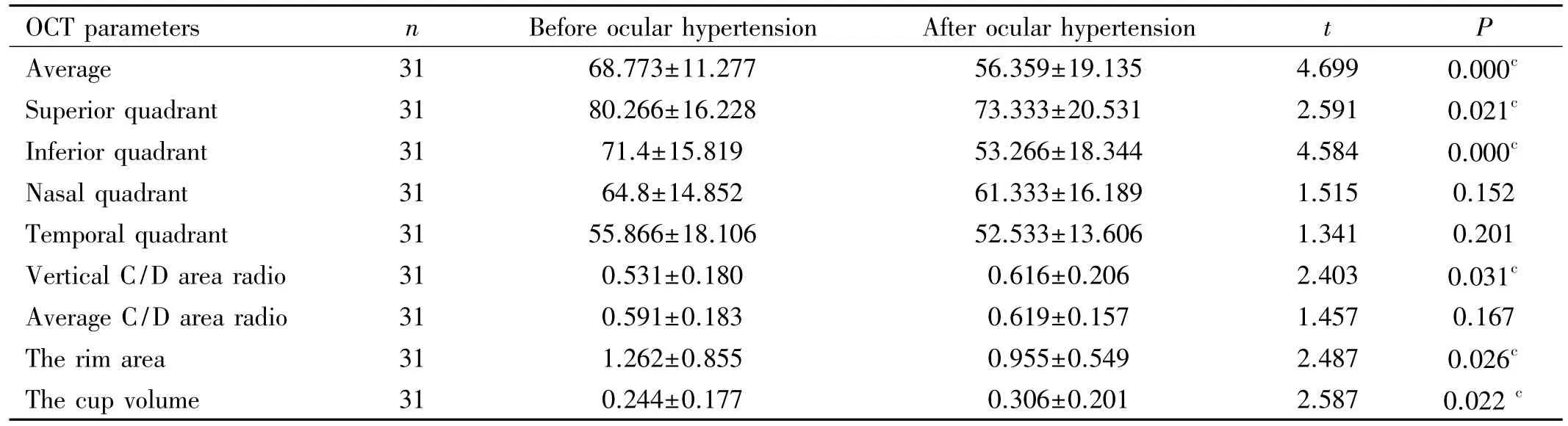
Table 4 Peripapillary RNFL thickness and optic disc status of the operation eye before and after ocular hypertension
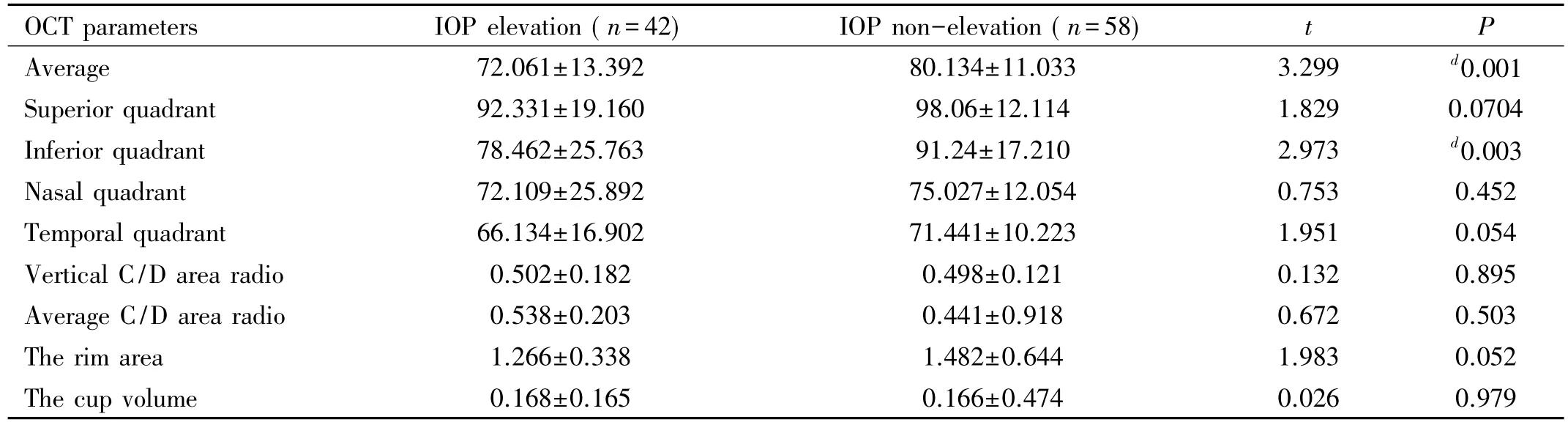
Table 5 Peripapillary RNFL thickness and optic disc status of opposite side of individuals
DISCUSSION
High myopia is a common ocular condition affecting billions of people in the world[11]. An increasing trend of eye complication,including RRD,has been one of the main reasons for vision loss in working people.In another hand,people with diabetes isanotherrisk group forretinal complication and POAG.There are more people underwent IOP elevation after vitrectomy with silicon oil tamponade than the ones with normal axial length,which is one of the major reasons for anterior chamber structure change[12],and fewer studies are available to discuss the relationship of high myopia with RRD in diabetic patients and IOP elevation after vitrectomy with silicon oil tamponade.
Potential mechanisms for such pressure elevation include trabecular meshwork edema, pupillary block,inflammation[13], combined surgery[14], retinal laser[15]posture and hemorrhage and time of RRD[16].It is considered that trabecular meshwork edema and inflammation induced by surgery were the leading causes for IOP elevation in patients who underwent vitrectomy,and glucocorticoid eye drops has been routine treatment for all patients after surgery to avoid IOP increasing.However,high myopia patients may have increased sensitivity to glucocorticoids because of their special eye anatomical structure[17],and they are at high risk of primary open angle glaucoma(POAG)[18-19],which can make glucocorticoid sensitivity more serious and more likely to elevate IOP after vitrectomy than in normal eyes.In addition,the risk of POAG is increasing when high myopia patients is diagnosed as diabetes. However, the relationship of glucocorticoid eye drops,pre-existing POAG and IOP elevation remains unclear in high myopia patients.
In the literature,corticosteroids have been linked to damage of the trabecular meshwork and a decrease coefficient of aqueous outflow[19].As the resistance to aqueous humor outflow increases, a secondary glaucoma will result[20-21].Clark et al[22]reported that dexamethasone could induce cytoskeletal changes and an increase in IOP.Zode et al[23]found that local administration of glucocorticoids can result in endoplasmic reticulum (ER) stress in the trabecular meshwork(TM)in a murine model of glucocorticoid-induced glaucoma.In addition,the highly specialized structure of anterior chamber angle in high myopia sensitizes to steroids,an otherwise effective mechanism in restraining inflammation induced by surgery.
The present study analyzed elevated IOP over the course of vitrectomy with silicon oil tamponade in high myopia patients with diabetes.We measured the IOP at the first day after surgery to exclude elevated IOP due to excess silicone oil injection.We found that postoperative IOPs in 5thto 7thdays and 1mo after surgery was significantly higher than before operation,respectively(t=3.595,P=0.000;t=2.497,P=0.014).And incidence of IOP elevation is higher than control group(χ2=3.284,P=0.002)during the first week following operation.As a result, we propose thattopicalocular dexamethasone treatment at the early stage postoperatively can ease inflammation in the trabecular meshwork on one hand and on the other hand,it might also be a potential risk factor for IOP elevation in the first week after operation.We believe that the resulting increase in IOP damages the structure and function of the trabecular meshwork and increases aqueous outflow resistance.
In our study,most patients can recover from secondary glaucoma with combined IOP lowering medications or anterior chamber paracentesis,which implies that glucocorticoid -induced IOP elevation is irreversible.However,there were three patients who needed filtering surgery for secondary glaucoma in experimental group and 11 patients in control group also underwent elevated IOP after vitrectomy,but they never use glucocorticoid eye drops at all,which suggested that there might be other reasons for postoperative IOP elevation in high myopia patients.
High myopia has consistently been associated with POAG in many population - based studies[24-26].However,POAG is usually overlooked because of the pathological changes in high myopia and patients with diabetes.Jones et al[21]reported that a history of past,current or suspected POAG,are all potential risk factors for glucocorticoid-induced IOP elevation.In the case of high myopia and PPV with silicon oil tamponade,a history of pre-existing POAG could also be an important risk factor for postoperative increase in IOP.
RNFL thinning as measured by the OCT has been regarded as a common characteristic of high myopia and POAG[27].For glaucoma discrimination,the ideal technology to measure RNFL thickness and ONH parameters was the OCT(AUC=0.943,P < 0.001)[28].In addition,Leung et al[27]showed that RNFL thinning in glaucoma patients occurred more frequently in the inferior retina,which is associated with the position of ganglion cell apoptosis according to the mechanism of glaucoma[29].The present study also analyzed the RNFL thickness and ONH parameters of the fellow,non-operated in the group of patients with IOP elevation and the group without IOP elevation.There was a statistically significant difference in the RNFL thickness overall average(t=3.299,P=0.001)and inferior quadrant(t=2.973,P=0.003)between two test groups.However, there was no statistically significant difference in rim area,cup volume and C/D in the two test groups.We propose that RNFL thinning and pre-existing POAG might be associated high-risk factors for postoperative IOP elevation.Whereas,the eyes included in this study was limited,and no glaucoma related examinations,such as visual field,were collected and analyze,so the relationship between POAG and vitrectomy postoperative IOP elevation still need further research.
Apoptosis of retinal ganglion cells and axonal loss is often present in the earliest stage[30],and precedes visual field damage in glaucoma[31].RNFL thinning is considered to be the earliest structural damage that can be measured(via the OCT) with the average RNFL thickness being a better predictor for early-stage glaucoma than rim area,cup volume or any other parameter for diagnosis of retina neurodegeneration in early- stage of glaucoma[28].However,because of the limitation of clinical research,research has not extensively reported the relationship of short-term IOP elevation and retinal neurodegeneration.
Hence,the present study discussed the instantaneous effects of IOP elevation on RNFL loss and optic disc parameters following PPV and IOP elevation.We foundthatIOP elevation can result in significant retinal neurodegeneration,even if for a very short time.Compared to the parameters before an elevation in IOP,RNLF thickness decreased in the overall average and superior and inferior quadrant thicknesses.As the rim area decreased,cup volume and vertical C/D increased.However,we did not observe early neuroretinal damage,because the duration of IOP elevation was unequal and could have been caused by the PPV surgery itself.
A limitation of our study was our inability to isolate the change in RNFL thickness that might have resulted from mild retinal edema after PPV surgery as Ohta et al[32]reports that can occur up to 12mo after surgery.Another limitation is the study design.The design does not assign causation.The design also cannot determine if the independent variable followed a temporal sequence of occurring before the effect(RNFL thickness change).Thus,more studies are needed to evaluate the IOP elevation and neuroretina damage.
In conclusion,there are numerous risk factors for IOP elevation followingvitrectomy,includingtheoveruseof glucocorticoid as well as preexisted suspected POAG in high myopia patients,especially with diabetes.Postoperative IOP elevation should be avoided because it can lead to damage to neuroretina even within a very short time.Therefore,regular POAG related ophthalmic examinations should be done in high myopia each time before vitrectomy.The judicious use of topical of glucocorticoid eye drops might be another way to diminish the incidence of IOP elevation.

